THORACOSCOPIC MANAGEMENT OF AN ESOPHAGEAL LUNG REPORT OF A CASE
Ivan Dario Molina-Ramirez1,
Santiago Correa-Salazar1,
Lina Eugenia-Jaramillo2,
Mizrahim Mendez-Manchola1,
Edgar Dario Alzate-Gallego1,
Ana Fernanda Garces-Martinez1,
Fernando Fierro-Avila1.
1. Department of Pediatric Surgery,
Fundación Hospital de la Misericordia,
Universidad Nacional de Colombia.
2. Department of Pathology,
Fundación Hospital de la Misericordia,
Universidad Nacional de Colombia.
Correspondence to:
Santiago Correa,
Bogotá DC, Colombia.
Phone Number 571-3002088776
Email : tiagosan25@hotmail.com
Esophageal lung is a rare bronchopulmonary foregut malformation in which the main stem bronchus arises from the esophagus. Since the description by Keely et al. in 1960, fewer than 25 cases have been reported. We present a case of a 4-month- old female, who was referred to our institution after 2 months of management for recurrent respiratory infections. Contrast studies were performed during the evaluation and a right bronchography was identified in the esophagogram. Bronchoscopy was performed confirming the atresic right bronchus. Complementary imaging and a cardiology evaluation confirmed the absence of major vascular anomalies—in particular, a pulmonary artery sling that has been described in relation to this entity. Due to the hypoplastic lung in the absence of major vascular anomalies, thoracoscopic pneumonectomy was deemed possible. The procedure was performed with four ports and 3 mm equipment was used. Special attention was paid to first identifying and dissecting the vascular structures, and then the arising esophageal bronchus was dissected. The hypoplastic lung was extracted through a small incision inferior to the axilla. We consider that because of the hypoplastic lung and vessels, the thoracoscopic approach is safe and feasible for the management of the esophageal lung and even for the esophageal bronchus in the absence of major vascular anomalies.
Keywords: Esophageal lung, esophageal bronchus, thoracoscopic pneumonectomy.
INTRODUCTION
Esophageal lung is a rare bronchopulmonary foregut malformation in which the main stem bronchus arises from the esophagus (1). Symptoms of this entity are described as nonspecific, with chronic cough, recurrent pulmonary infections and respiratory distress as the usual presenting features (2). Usually, the treatment of choice has been the division of the communicating tissue and the resection of the anomalous lung tissue (1). We present a case of a 4-month-old female with a right esophageal lung managed with a right pneumonectomy using the thoracoscopic approach.
CASE REPORT
A 4-month-old female was referred to our institution after 2 months of management for recurrent respiratory infections. She was born at 34 weeks of gestation and weighed 1600 grams, requiring 17 days in the neonatal care unit for apneas and a hypoplastic right lung.
Several studies were performed during these 2 months. Chest X-rays showed right diffuse infiltrates and a markedly hyperinsufflated left lung (fig 1). Due to the persistent respiratory involvement, upper gastrointestinal series were made, in which a right bronchography was identified in the esophagogram (fig 2). An echocardiogram and CT scan with vascular reconstruction were also performed and no major vascular anomalies were identified;the pulmonary artery sling, an entity that has been specifically reported in association with the esophageal lung was ruled out in particular. A citomegalovirus infection was confirmed and treated.
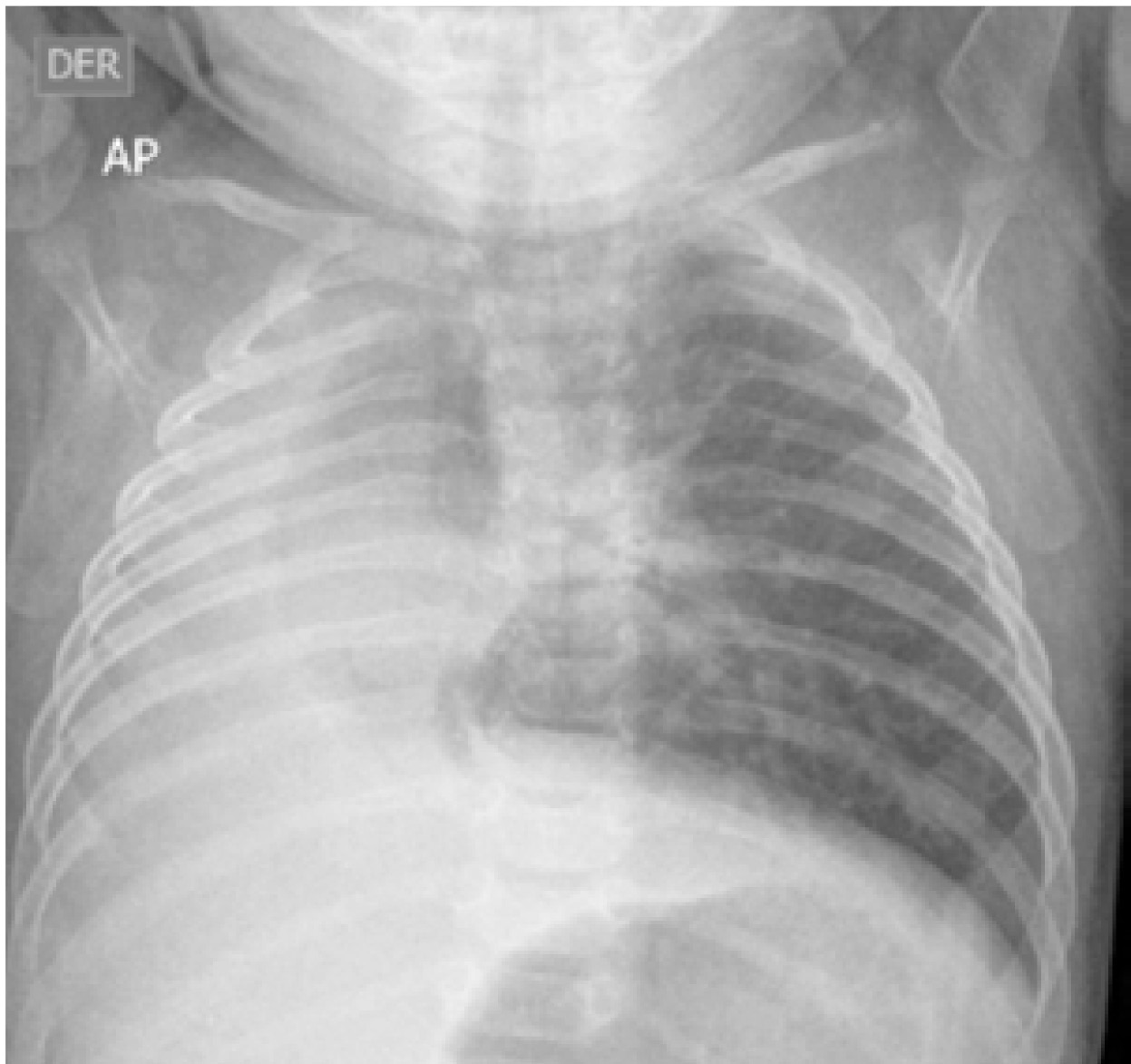
Fig 1. Chest X-ray. Right diffuse infiltrates and markedly hyper insufflated left lung.
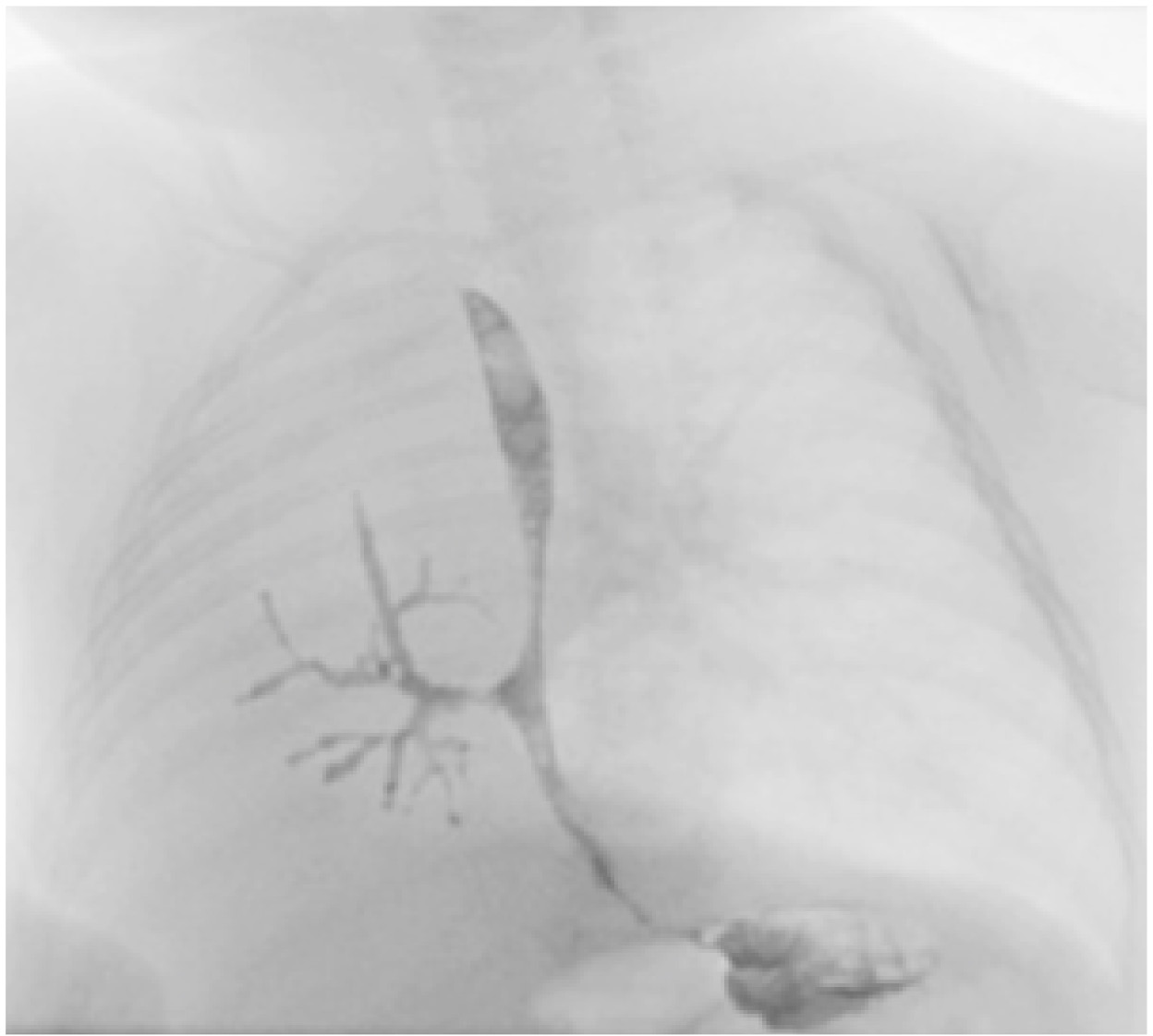
Fig 2. Esophagogram, with right bronchography.
Upon arrival to our institution, a multidisciplinary group evaluated the patient. She presented as nutritionally impaired with respiratory distress, requiring supplementary oxygen and nutritional support. A cardiology evaluation confirmed again the absence of major vascular anomalies with a hypoplastic right lung artery.
Due to the hypoplastic lung in the absence of major vascular anomalies, a thoracoscopic pneumonectomy was deemed possible and she was scheduled for surgery.
Immediately before surgery, a rigid bronchoscopy and esophagoscopy were performed. An atresic right bronchus was confirmed (fig 3) and the right bronchus arising from the esophagus was identified.
The patient was placed in the left lateral decubitus position, and four ports were placed with one port of 5 mm and three ports of 3 mm. 3 mm equipment was used. A hypoplastic right lung was confirmed and the absence of lobes was noted. Special attention was paid in the identification of the vascular structures at the pulmonary hilum that was covered by enlarged lymph nodes (fig 4). After these structures were identified, the esophagus was visualized and the right bronchus arising from the esophagus was dissected circumferentially (fig 5). 5 mm hemo-loks were used to ligate proximally and distally the anomalous arising bronchus, which was subsequently transected with scissors. Then, the pulmonary artery (fig 6) was ligated proximally and distally with 5 mm hem-o-loks and transected with scissors. Finally, the pulmonary veins were ligated with 5 mm hem-o-loks proximally and transected. After the vascular structures and esophageal bronchus were divided, the hypoplastic lung was extracted through a small incision inferior to the axilla.
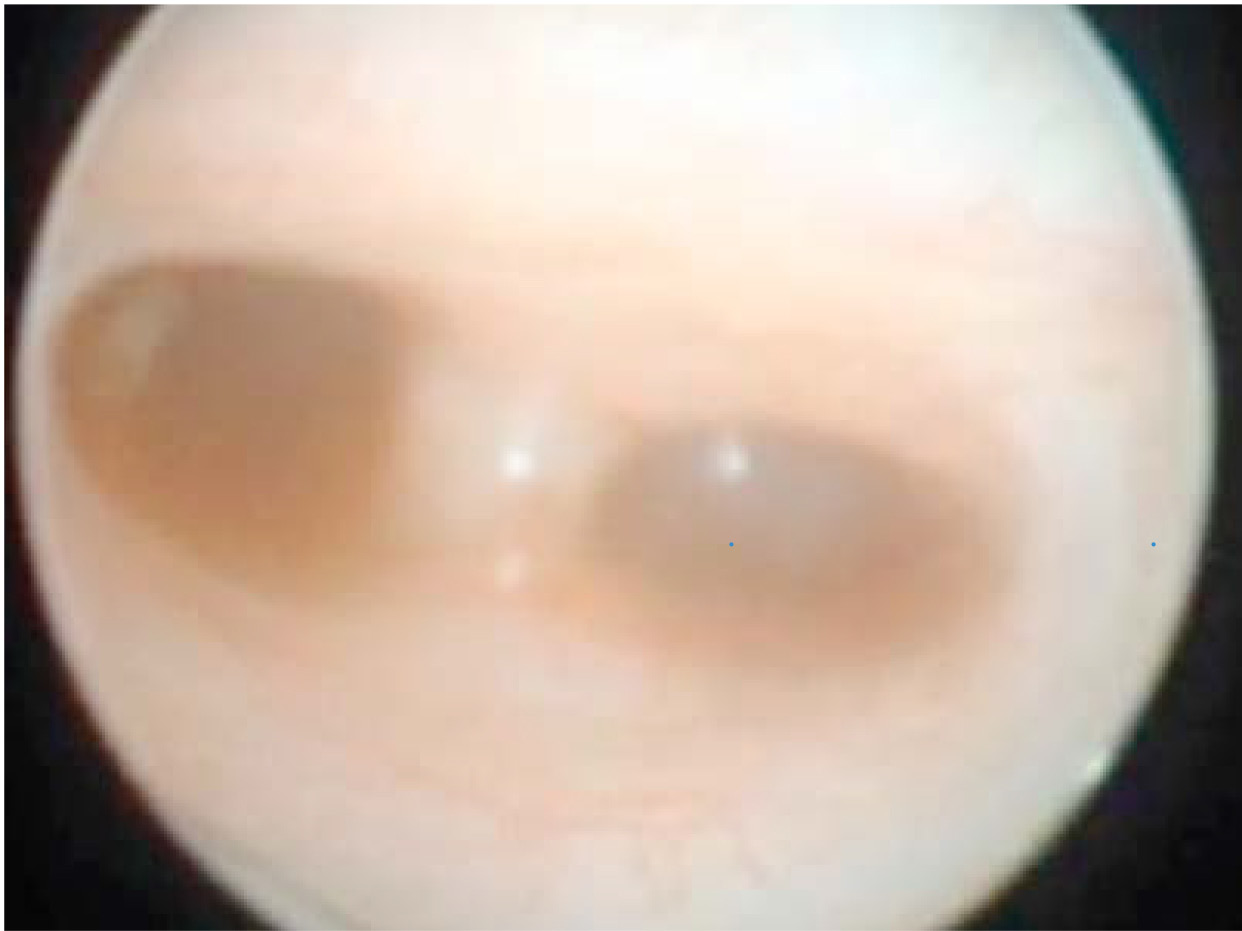
Fig 3. Bronchoscopy. Atresic right bronchus.
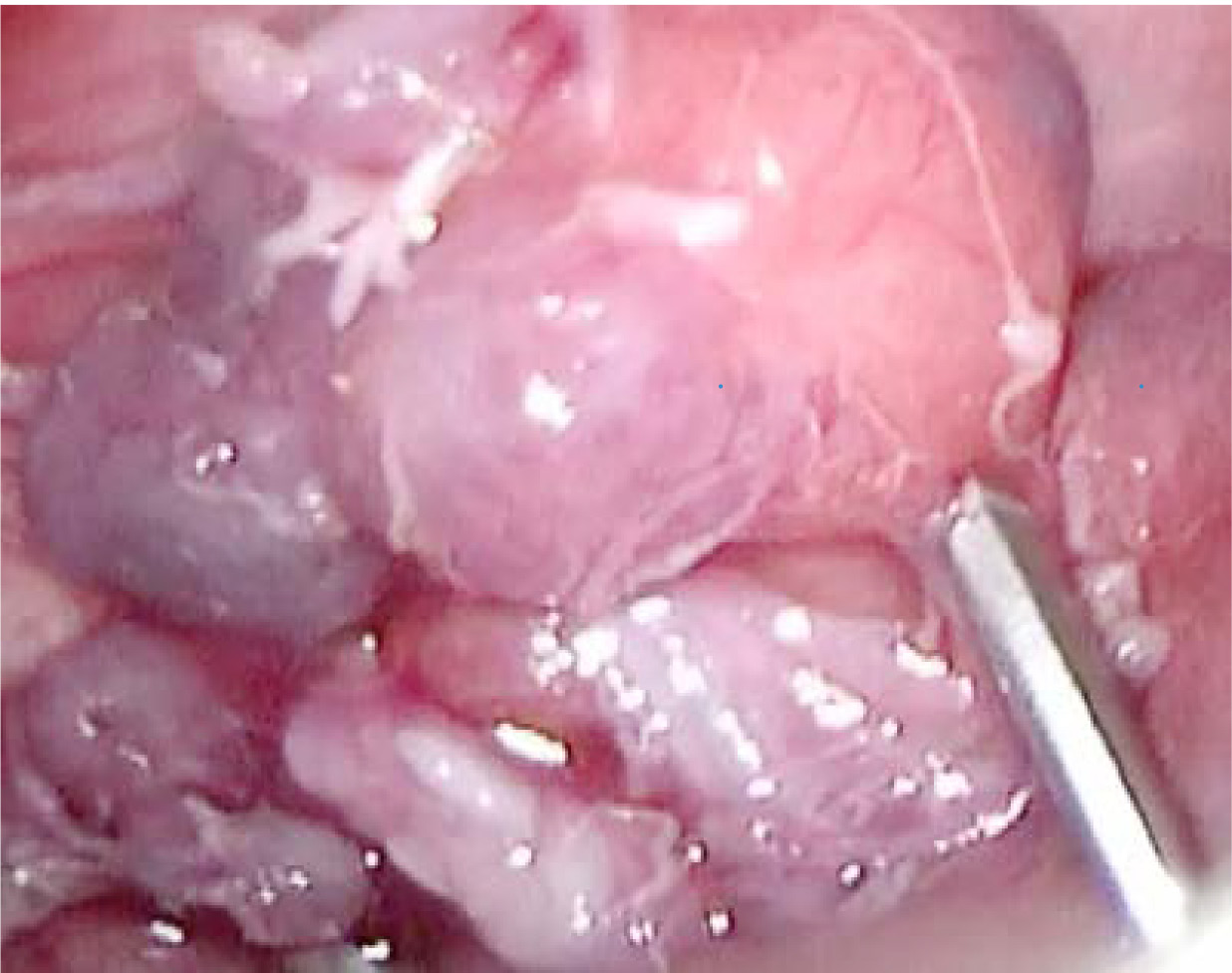
Fig 4. Enlarged lymph nodes covering the hilum

Fig 5. Main Bronchus (MB) arising from the esophagus (E).

Fig 6. Hypoplastic right pulmonary artery.
The patient was kept in hospital for one month after surgery due to a was initiated early in the postoperatory period through a nasogastric tube and oral intake was initiated after extubation was performed. The patient was discharged with low flow supplementary oxygen. In tests performed at the second, third, and fourth month, the patient was doing well with adequate scarring process but still with a low flow supplementary oxygen requirement. (fig 7). Nevertheless, due to a markedly hyperinsufflated left lung and right mediastinal shift (fig 8), the possibility of right pneumonectomy syndrome was taken into account. Unfortunately, the patient died after 7 months due to a viral community -acquired pneumonia.

Fig 7. Outpatient control.

Fig 8. Control chest X-ray. Persisted hyperinsufflated left lung with right mediastinal shift.
Pathology evaluation of the surgical specimen showed a small, rubbery lung without lobulation, which weighed half of that expected for her age (15.5/33 g) (fig 9). The alveoli were small, delineated by cuboidal epithelium and there was marked lymphocytic infiltrate with presence of lymphoid follicles and well-formed germinal centers in bronchiolar walls as a sign of chronic infection (Fig 10).

Fig 9. Right pneumonectomy: small, rubbery airless lung without lobulation.
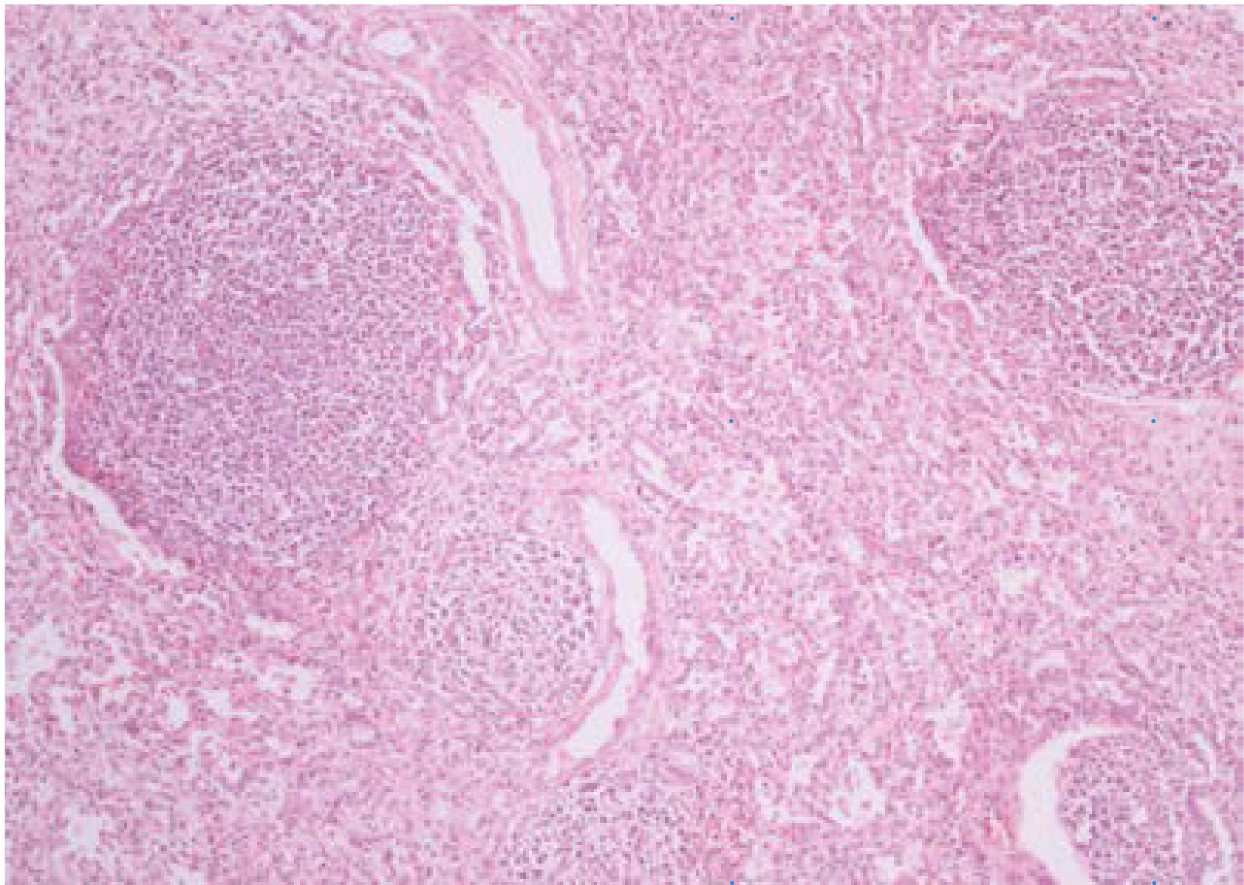
Fig 10. Lung parenchyma with marked lymphocytic infiltrate, presence of lymphoid follicles and well-formed germinal centers (H&E 100X)
DISCUSSION
The esophageal lung and esophageal bronchus are rare bronchopulmonary foregut malformations (1)(4). Since the description by Keely et al. in 1960, fewer than 25 cases of esophageal lung have been reported (1). The etiology is still unknown, but the evidence of squamous epithelium and respiratory epithelium in the communicating tissue between the lung and the esophagus supports the ventral foregut budding theory (3).
Most cases have been reported in the right side as in our case (1). Clinical presentation as described above is nonspecific, with chronic cough, respiratory distress and recurrent pulmonary infections (2).
This kind of pathology strongly supports the necessity of upper gastrointestinal tract images with contrast in patients with chronic respiratory symptoms, as it was used to diagnose this patient and repeated by many authors like Robin Cotton. Other malformations have been described in relation to this condition, such as esophageal atresia, duodenal atresia or stenosis, congenital heart disease and pulmonary artery sling (1)(4). These must be studied before surgery.
Traditionally, the treatment of choice has been the division of the communicating tissue and the resection of the anomalous lung tissue (1,6). Nevertheless, Lallemand et al., reported two successful reimplantations of esophageal bronchus to the trachea in the neonatal period (5,6), which may be only achievable early in life and has not been reported for complete lung communication. Even though reports of right postneumonectomy syndrome have not been found in the reviewed literature, this option should be considered. Due to the hyperinsufflated left lung and the absence of the right lung after surgery, there will be a continuous shifting of the mediastinum to the right, raising the possibility of developing this syndrome.
As in the opinion of the authors of this report, despite the unrelated death of the patient, we consider that due to the hypoplastic lung and vessels, the thoracoscopic approach is safe and feasible for the management of the esophageal lung and even for the esophageal bronchus in the absence of major vascular anomalies.
References
1. Sugandhi N, Sharma P, Agarwala S, Kabra SK, Gupta AK, Gupta DK. Esophageal lung: presentation, management, and review of literature. J Pediatr Surg. 2011;46(8):1634-7. doi: http://doi.org/fm239r.
2. Katz R, Pitt R, Kim D, Wingrove B. Thoracoscopic pneumonectomy for communicating bronchopulmonary foregut malformation in a 4-month- old child. J Pediatr Surg. 2010;45(2):427-9. doi: http://doi.org/cdpbhh.
3. Katayama Y, Kusagawa H, Komada T, Shomura S, Tenpaku H. Bronchopulmonary foregut malformation. Gen Thorac Cardiovasc Surg. 2011;59(11):767-70. doi: http://doi.org/bdrx2x.
4. Pimpalwar AP, Hassan SF. Esophageal bronchus in an infant- a rare cause of recurrent pneumonia. J Pediatr Surg. 2012;47(1):e5-8. doi: http://doi.org/fzqbp8.
5. Lallemand D, Quignodon JF, Courtel JV. The anomalous origin of bronchus from the eso phagus: report of three cases. Pediatr Radiol. 1996;26(3):179-82. doi: http://doi.org/c8f7n7.
6. Yankovic F, Varela P, Casado C, Herrera O, Casado C, Herrera O, Latorre JJ. Pulmón esofágico: Caso clínico. Rev Chil Pediatr. 2006;77(6):604-7. doi: http://doi.org/fvwcdh.