Case report:
Idiopathic meconium peritonitis as a surgical emergency: A case report in a newborn
Palabras clave: Meconium; Peritonitis; Cyst; Obstruction; Postoperative; Ileus; Digestive System Abnormalities; Prenatal Diagnosis.
Keywords: Peritonitis; Meconio; Quistes; Obstrucción intestinal; Ileus; Complicaciones postoperatorias; Anomalías del sistema digestivo; Diagnóstico prenatal.
Ana Jiménez–Uribe
Medical Intern,
Faculty of Medicine
Universidad de los Andes
Bogotá D.C. – Colombia
Armando Rojas
Chief, Pediatric Surgery Unit
Fundación Santa Fe de Bogotá
Universidad de los Andes
Bogotá D.C. – Colombia
Fernando Fierro
Pediatric Surgeon – Fundación Santa Fe de Bogotá
Universidad de los Andes
Chief, Department of Surgery – Hospital de la Misericordia
Universidad Nacional de Colombia
Bogotá D.C. – Colombia
Corresponding author:
Ana María Jiménez Uribe.
Carrera 68C #22b – 71
Edificio Alameira. Torre 2. Apto. 702
Email: am.jimenez1564@uniandes.edu.co
SUMMARY
Meconium peritonitis is a rarely described condition that is typically found in fetal and perinatal patients. It manifests in different ways and requires an early diagnosis. In this case report, a clinical suspicion of the disease was made at the antenatal period through an obstetric ultrasound scan showing an abdominal mass in both the bottom and top right quadrants. The patient initial symptoms were those of acute intestinal obstruction. Nevertheless, these symptoms improved after surgical approach was timely performed. Based on this outcome, it can be concluded that a favorable outcome to this pathology depends on its early diagnosis, since an early diagnosis decreases morbidity and mortality chances.
Introduction
Meconium peritonitis is a non-infectious chemical inflammatory response secondary to intestinal perforation in the fetal period (1). It manifests in several ways, including cyst or meconium pseudocyst (2), where the most common complication is intestinal obstruction, a surgical emergency that rapidly alters the patient’s general condition, since its symptoms include emesis, oral feed intolerance and severe dehydration, therefore it requires a rapid and specialized approach, particularly in this age group (3).
In this case, multiples studies and an early diagnosis allowing the anticipation of possible complications were required. Likewise, an analysis of the patient’s clinical condition was necessary to decide aspects such as when to perform the surgery, pre-surgical studies, surgical approach and postoperative actions that prevented the development of pathologies such paralytic ileus.
Clinical case
A 19-day-old female patient from Manizales, Colombia, who was referred by her pediatrician due to a prenatal diagnosis consisting of an ultrasound showing abdominal mass with a fixed bowel loop compatible with possible meconium peritonitis. The patient had a left femur fracture secondary to perinatal trauma caused by fetal extraction through caesarean section. There were not complications during the term of pregnancy and, apart from folic acid during the first trimester, the mother did not consume any medication. The patient was asymptomatic in the outpatient evaluation, thus her case was referred to the surgical board of the Fundación Santa Fe de Bogotá, who decided to schedule a mass resection surgery.
When the girl was 24 days old, her mother took her to the emergency department due to abdominal distention and several emetic episodes. After performing the patient’s physical assessment it was determined that she was active, her general condition was regular and that she had a left femur immobilization harness (fracture caused by labor dystocia). She had a distended abdomen, painful on palpation, with a mass located in her upper abdomen. The mass size was 5cm x 5cm approximately and it was delimited, solid and fixed. Later, this finding was confirmed through an abdominal ultrasound. In addition, it was observed that the size of the mass did not increase: it remained at 42 mm x 41 mm. Finally, an abdominal x-ray showed a calcified mass with signs of possible partial intestinal obstruction (see Figure 1).
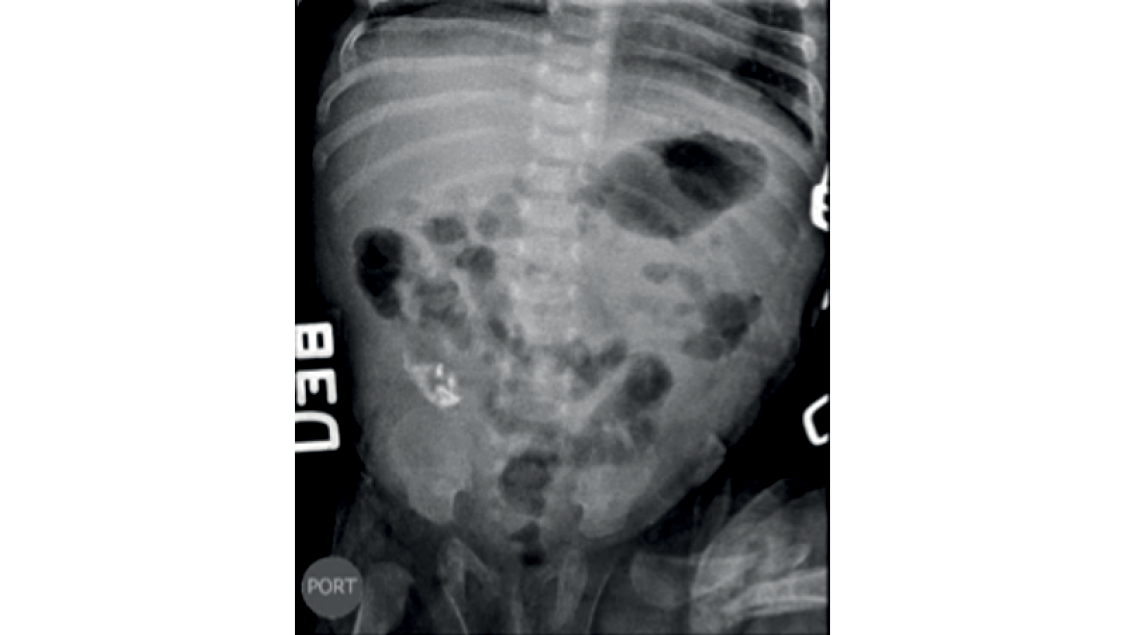
Fig 1. Abdominal x-ray. 42 mm x 41 mm calcified mass with signs of possible partial intestinal obstruction.
Source: Images obtained from the data collected in the study.
Due to the peritonitis acute clinical manifestation, the patient was sent to the operating room where the surgeons found an abdominal mass of approximately 7 x 7 cm with two cavities in the right hemiabdomen that adhered to the parietal peritoneum. The largest portion consisted of a solid mass of apparently meconium content, whereas the small portion was cystic, with non-fetid fibrinous membranes (see Figures 2a, 2b and 2c). Additionally, several adhesions in jejunoileal loops of bowel (see Figure 2d) and a 0.3 cm diameter antimesenteric intestinal perforation located at 10 cm from the ileocecal valve were observed. Finally, a 0.5 cm high broad-based Meckel’s diverticulum located at 20 cm from the ileocecal valve was also found (see Figure 2e).
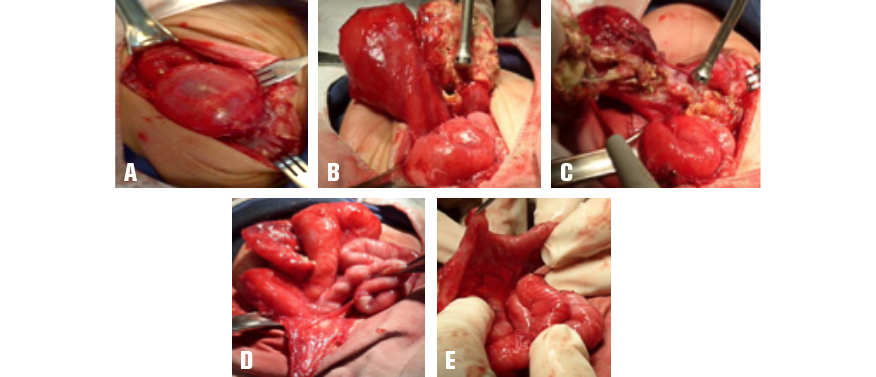
Fig 2A, 2B and 2C. 7 x 7 cm mass with two cavities: the first cavity is large and solid and has meconium content, while the second is cystic and has non-fetid fibrinous membranes. Fig 2D. Jejunoileal adhesions. Fig 2E. Antimesenteric intestinal perforation found 10 cm away from the ileocecal valve.
Source: Images obtained from the data collected in the study.
Taking these findings into account, a complete resection of the mass, a release of intestinal adhesions and a suture of the intestinal perforation, in a transverse direction, were made. Because of the size of the Meckel’s diverticulum its resection was not deemed suitable. Subsequently, pathology samples were taken and the patient was transferred to the pediatric intensive care unit, where she started receiving parenteral nutrition.
The follow-up abdominal x-ray showed a smaller amount of gas in the gastric chamber, as well as residual heterogeneous calcifications in the right hemiabdomen (see Figure 3). Pathology results allow identifying “an ileal perforation with dystrophic calcification, adhesions of richly vascularized fibrous tissue that was chronically inflamed, a peritoneal cyst associated with mixed inflammation and fibrosis, and meconium peritonitis”, which led to dismiss an intestinal duplication diagnosis.

Fig 3. Postoperative abdominal x-ray taken 24 hours after the surgery was performed.
Source: Images obtained from the data collected in the study.
In the postoperative period, the patient had a four days development ileus, which is an expected outcome from the surgical intervention and the pathology she underwent. In the fifth postoperative day she successfully tolerated oral feeding and in the sixth postoperative day she had her first liquid bowel movement, so it was decided to quit parenteral nutrition and keep feeding her orally. Since there were no complications during her recovery, the patient was discharged in the seventh postoperative day.
DiscussioN
Fortunately, the case reported here had an early diagnosis that was made in utero at week 24 of gestation from the identification of a calcified mass, which is a pathognomonic sign of meconium peritonitis (3). This allowed the pediatric surgery unit to have a prior knowledge of the case, which in turn made possible choosing an appropriate treatment plan. Furthermore, since prenatal and postnatal images of the patient were available it was possible to define the surgical approach to be performed, as well as the location and size of the mass.
The positive aspect of the physical examination was the presence of a palpable abdominal mass, which is something unusual and is commonly associated with symptoms such as abdominal distension, ascites, and intra-abdominal calcifications, among others (4). On the other hand, despite scheduling a mass resection surgery because of the asymptomatic condition of the patient, the procedure was performed as a surgical emergency due to the manifestation of acute obstructive symptoms that developed in a short time. However, the identification of the obstructive condition and its prompt medical-surgical management allowed an adequate progress and favorable development of both the surgical intervention and the postoperative recovery.
As for surgical management, a pseudocyst mass compatible with a meconium cyst was found. The mass was associated with a 0.3 cm diameter ileal perforation with necrosis in its borders and did not have underlying vascular involvement, thus resecting a part of the ileum was not necessary, a typical complication in this pathology (5,6), obtaining a better prognosis. It is important to emphasize that during the course of the disease, an added left femur fracture was always considered. Fortunately, such fracture did not cause any complications. Findings made during the surgical procedure suggested a possible intestinal duplication, since the walls of the mass resembled those of the intestine, but this option was later discarded by the pathology report.
Meconium peritonitis may be secondary to several etiologies, including intestinal atresia, volvulus, congenital flange, and meconium plug syndrome (2,7), the latter being the most common cause. A low percentage of these patients show a clinical picture of idiopathic origin, also known as simple meconium peritonitis (5), which, after discarding intestinal duplication, is the most probable diagnostic suspicion for the case reported here. This condition has been associated with transient vascular insufficiency or hypoxia of the fetal bowel, as well as with certain fetal intestinal infections, however such associations have not been yet fully established (6,5).
Regarding medical-surgical management in this case, surgical intervention instructions should be emphasized, including intestinal obstruction or persistent drainage of meconium to the abdominal cavity, which can lead to progressive abdominal distention, respiratory distress, or sepsis (7). Therefore, the surgical emergency instruction reported here was appropriate. At the beginning of the clinical picture, resecting the mass, due to its size rather than to gastrointestinal symptoms, was considered as an appropriate option in the context of an asymptomatic patient, given the risk of complications.
In conclusion, meconium peritonitis is a condition poorly described in the literature. In addition, it has a broad spectrum of both etiologies and probable short-term complications (1). Its clear method of diagnosis allows the medical staff to provide a rapid and adequate management (3). This case report shows how meconium peritonitis complications can develop acutely and unexpectedly. Fortunately, complications experienced by the patient had a favorable outcome since they were treated in a timely manner, which substantially decreased the probability of morbidity and mortality.
Conflicts of interest
The authors of this study state there were not conflicts of interests in writing this case report up (fees, personal benefits) or personal conflicts (directed towards a service or research unit) between authors and medicine manufacturers or surgical material suppliers.
Funding
None stated by the authors.
References
1.Lee YC, Chen CJ. Meconium pseudocyst: a classical and successfully treated case. J Formos Med Assoc. 2009;108(3):247-252. http://doi.org/bw85s2.
2.Tsai MH, Chu SM, Lien R, Huan HR, Luo CC. Clinical manifestations in infants with symptomatic meconium peritonitis. Pediatr Neonatol. 2009;50(2):59-64. http://doi.org/cvjpv2.
3.del Ciampo IR, Oliveira TQ, del Ciampo LA, Sawamura R, Torres LA, Augustin AE, et al. Early manifestations of cystic fibrosis in a premature patient with complex meconium ileus at birth. Rev Paul Pediatr. 2015;33(2):241-5. http://doi.org/f27fps.
4.Dirkes K, Crombleholme TM, Craigo SD, Latchaw LA, Jacir NN, Harris BH, et al. The natural history of meconium peritonitis diagnosed in utero. J Pediatr Surg. 1995;30(7):979-982. http://doi.org/dg28xd.
5.Uchida K, Koike Y, Matsushita K, Nagano Y, Hashimoto K, Otake K, et al. Meconium peritonitis: Prenatal diagnosis of a rare entity and postnatal management. Intractable Rare Dis Res. 2015;4(2):93-7. http://doi.org/bqm2.
6.Barthel ER, Speer AL, Levin DE, Naik-Mathuria BJ, Grikscheit TC. Giant cystic meconium peritonitis presenting in a neonate with classic radiographic eggshell calcifications and treated with an elective surgical approach: a case report. J Med Case Rep. 2012;6:229. http://doi.org/fzcxfb.
7.Lee G, Chandran S, Rajadurai VS. Calcified meconium pseudocyst: X-ray diagnosis of meconium peritonitis at birth. BMJ Case Rep. 2015;2015:bcr2015211052. http://doi.org/bqm3.
8.Ionescu S, Andrei B, Oancea M, Licsandru E, Ivanov M, Marcu V, et al. Postnatal Treatment in Antenatally Diagnosed Meconium Peritonitis. Chirurgia (Bucur). 2015;110(6):538-44.