Resumen
Introducción. La insuficiencia venosa crónica puede tener complicaciones graves como úlceras flebostáticas en las extremidades inferiores. Se ha establecido que la aplicación de plasma rico en plaquetas autólogo (PRP) es una opción segura y eficaz en el tratamiento de las úlceras crónicas, siendo empleado como terapia adyuvante. El uso de PRP ozonizado en el tratamiento de estas úlceras no ha sido muy estudiado, pero clínicamente puede ser una alternativa beneficiosa.
Presentación del caso. Mujer de 65 años, diagnosticada con insuficiencia venosa crónica a los 42 años, quien asistió a consulta externa por el servicio de angiología y cirugía vascular por una úlcera flebostática en una de sus extremidades inferiores. La paciente recibió cinco aplicaciones de PRP activado con ozono-cloruro de calcio y membranas de fibrina como tratamiento complementario. A partir de la segunda aplicación se observó una mayor epitelización en el área de la lesión; la cicatrización completa de la úlcera se logró 6 semanas después de finalizado el tratamiento. No se registraron reacciones adversas graves y la paciente refirió una disminución del dolor y mejoría en la realización de actividad física.
Conclusiones. La aplicación local de PRP activado con ozono-cloruro de calcio y membranas de fibrina resultó ser una intervención útil para el tratamiento de la úlcera flebostática en el miembro inferior de la paciente reportada, ya que este estimuló la epitelización y cierre de las heridas, lo cual le mejoró la calidad de vida.
Abstract
Introduction: Chronic venous insufficiency may lead to serious complications such as phlebostatic ulcers in the lower limbs. It has been established that the use of autologous platelet-rich plasma (PRP) is a safe and effective option in the treatment of chronic ulcers as an adjuvant therapy. The use of PPR combined with ozone in the treatment of these ulcers has not been extensively studied, but it may be a beneficial alternative in clinical terms.
Case presentation: A 65-year-old woman, diagnosed with chronic venous insufficiency at the age of 42, visited the angiology and vascular surgery outpatient department due to a phlebostatic ulcer in one of her lower extremities. The patient received five injections of PRP activated with ozone-calcium chloride and fibrin membranes as a complementary treatment. From the second administration onwards, increased epithelialization was observed in the area of the lesion; complete healing of the ulcer was achieved 6 weeks after the end of the treatment. No serious adverse reactions were reported, and the patient stated that pain decreased and physical activity improved.
Conclusions: The local administration of PRP activated with ozone-calcium chloride and fibrin membranes proved to be a useful intervention for the treatment of the phlebostatic ulcer in the lower limb of the patient reported, since it stimulated epithelialization and wound closure, improving her quality of life.
Introduction
Most chronic ulcers in the lower limbs are associated with venous disorders. Venous hypertension damages the vessel walls and ultimately tissue hypoxia leads to skin breakdown (1). The prevalence of non-healing venous ulcers is between 1% and 2% among the general population (2-4), accounting for almost 75-80% of all vascular ulcers (4).
Venous ulcers are a serious public health problem at a global level due, among other factors, to their chronicity and constant recurrences. Likewise, these ulcers cause both local and systemic disorders in the patient, leading to a deterioration in their quality of life (5,6).
The objective of the treatment for these ulcers is to achieve the fastest possible healing, so therapy is based on two aspects: treating the primary triggering cause and treating the ulcerated area with drugs, dressings, or compounds that together stimulate the restitution of the healing processes (7).
Over the past two decades, emerging cell therapies, such as autologous platelet-rich plasma (PRP), have become relevant in the treatment of venous ulcers because of their potential for regenerative medicine (8,9). PRP is a conglomerate of thrombocytes, cytokines and different growth factors (GF) secreted by platelet alpha granules, which activate the natural healing process. Therefore, its use in the treatment of chronic wounds and ulcers not only promotes healing, but also prevents lower limb amputations resulting from wound complications that do not improve (6,10,11).
Medical ozone has been used as a PRP activator, given that studies such as those by Valacchi et al. (12) and Re et al. (13) have shown that platelet aggregation is stimulated when heparinized plasma is ozonized, also enhancing the release of GF. Thus, when ozone comes into contact with PRP, ozonides and other molecules are generated and activate different enzymes when they enter the thrombocytes, enhancing the formation of pro-resolving mediators (prostaglandins, thromboxanes, among others). This allows the release of GFs in less time and activates different metabolic processes of physiological repair (14).
The aim of this study was to report the results obtained in the treatment of a patient with phlebostatic ulcer who was administered PRP activated with ozone-calcium chloride (ozonized) and fibrin membranes to treat her lesion.
Case presentation
A 65-year-old woman, retired and resident of La Lisa municipality in the province of Havana (Cuba), who lived with her family (children and grandchildren) in a house in good conditions and was able to carry out her daily living activities independently, attended a specialized angiology and vascular surgery appointment at the Pedro Kourí Institute of Tropical Medicine (IPK), a tertiary care hospital, in November 2019. During this visit, she reported that she did not have any toxic habits (alcoholism, smoking, or other addictions) and followed a low-sodium diet. Her underlying diseases included hypertension under pharmacological treatment (1 tablet of captopril 25mg and 1 tablet of hydrochlorothiazide 25mg per day) and chronic venous insufficiency of the lower limbs, which had been diagnosed 23 years earlier. Due to the latter condition, the patient had had several ulcerative lesions in the lower limbs with variable opening and closing periods.
The initial physical examination showed that the patient was overweight. Vascular examination revealed trophic skin changes in the last third of the left lower limb, presenting a class C6 ulcerous lesion (according to the Clinical, Etiological, Anatomical and Pathophysiological Classification for venous ulcers) of approximately 7-8cm in diameter with defined borders, dirty bed with scant yellowish secretion, and some slough. This lesion, as indicated by the patient, had appeared 4 months earlier (Figure 1).

Figure 1. Phlebostatic ulcer before surgery with platelet-rich plasma activated with ozone and fibrin membranes.
Source: Image obtained while conducting the study.
The following day, at a second appointment, a bacterial exudate culture and an antibiogram of the lesion were performed, as well as a vascular hemodynamic study to quantify the degree of venous insufficiency. The culture result reported the presence of Pseudomonas aeruginosa susceptible to ciprofloxacin.
The result of the vascular hemodynamic study reported insufficiency of both femoral vein valves, as well as left internal saphenous vein valve insufficiency, with no other alterations. Given the findings, outpatient treatment with ciprofloxacin (2 tablets of 250mg every 12 hours for 10 days) orally was indicated considering antibiogram sensitivity; likewise, local treatment with 2% acetic acid dressings for 5 days was simultaneously instituted. The patient did not receive compression therapy because she reported being allergic to the elastic material of the bandage.
At the next appointment, which took place after the patient had completed the indicated antibiotic treatment, a culture of the evolving bacterial exudate showed that the local infection was under control. Given the need to speed up the healing of the lesion and avoid new bacterial colonization, a specialist in angiology and vascular surgery with experience in regenerative medicine and ozone therapy treatments decided to prescribe a cycle of 5 treatments every 7 days with the combination of platelet-rich-plasma activated with ozone and fibrin membranes; this treatment was started 2 days after completing the antibiotic treatment.
The preparation and administration of both the platelet-rich-plasma and ozone therapy and fibrin membranes was carried out in the operating room of the IPK in full compliance with biosafety standards and was performed by a team consisting of a specialist in pharmacology, a licensed nurse, and a physician specializing in angiology and vascular surgery.
The blood required to obtain PRP and fibrin membranes was drawn from the peripheral vein of the upper limb of the same patient immediately before each intervention. To this end, 5 tubes without anticoagulant and 2 heparin tubes, both 9mL vacuum tubes (Vacuette®), were used. These tubes were placed in a Medifuge centrifuge (Silfradent®) and, once centrifugation was completed, the CD34+ cell-rich fraction was separated from the portion of blood plasma obtained in the tubes with heparin, then the PRP fraction, and finally the platelet-poor plasma (PPP) fraction. One syringe per fraction and an 18G x 75mm spinal needle were used to retrieve these fractions.
The PPP portion was placed in an albumin denaturation equipment (Silfradent®) for gelation (plasmagel). The PRP was activated with ozone at 60 µg/mL using the Ozonobaric P® generator with 10% calcium chloride. The three fractions were then combined and homogenized.
Fibrin membranes were obtained from the clot formed in the plasma fraction in the tubes without anticoagulant (Figure 2).

Figure 2. Fibrin membrane obtained from tubes without anticoagulant.
Source: Image obtained while conducting the study.
The lesion was cleaned with physiological saline solution before administering the prepared material, and then the ulcer was irrigated with PRP activated with ozone, and covered with fibrin membranes and a dressing that was kept for three days (Figure 3).

Figure 3. Phlebostatic ulcer after administering platelet-rich plasma activated with ozone and fibrin membranes.
Source: Image obtained while conducting the study.
The administration of the preparation containing PRP combined with ozone on the lesion had a favorable effect on the evolution of the lesion since it was observed that the granulation tissue in the ulcer bed and the skin healed rapidly after the second administration, decreasing the initial diameter (Figures 4 and 5).

Figure 4. Phlebostatic ulcer after the second administration of platelet-rich plasma activated with ozone and fibrin membranes.
Source: Image obtained while conducting the study.

Figure 5. Phlebostatic ulcer after fifth administration of platelet-rich plasma activated with ozone and fibrin membranes.
Source: Image obtained while conducting the study.
Complete healing of the lesion was achieved six weeks after the last administration of the PRP activated with ozone and fibrin membranes (Figure 6).

Figure 6. Complete ulcer healing six weeks after the last administration of platelet-rich plasma activated with ozone and fibrin membranes.
Source: Image obtained while conducting the study.
In total, 5 rounds of PRP activated with ozone and fibrin membranes were administered, and no related adverse reactions were observed. The procedure was well tolerated by the patient and there was no infection; in fact, the patient reported a decrease in the perception of physical pain and an improvement in her ability to perform physical activity after this treatment.
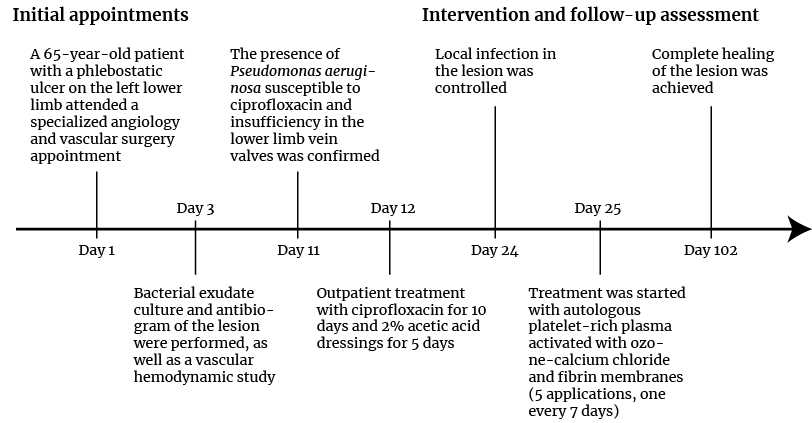
Figure 7. Case timeline.
Source: Own elaboration.
Once the treatment was completed and due to the impossibility of using elastic containment as a result of the mentioned allergy, the patient was instructed to maintain a hygienic-dietary regimen, rest her veins, and use diosmin (1 tablet of 500mg every 12 hours for 6 months). Heparin sodium cream (25g once a day for 6 months) was prescribed as a local skin treatment.
Before and after each scheduled procedure, a physical examination of the patient was performed as part of the intervention’s follow-up. In these examinations, the physician evaluated the evolution of the lesion (photographic evidence), the occurrence of adverse reactions, compliance with therapeutic indications, and the patient’s perception of quality of life assessed by means of a modified version of the MOS-12 (Medical Outcomes Study) questionnaire.
Before starting treatment, the patient was informed about the characteristics of the treatment, its benefits and risks, as well as her right to withdraw the interventions when she deemed it appropriate. She was also asked to sign an informed consent form as proof of her approval to receive the treatment.
Discussion
Phlebostatic ulcers are a serious health problem due to their chronic nature and their high prevalence in elderly patients (15). Different studies have demonstrated the potential of PRP to improve the healing mechanisms of skin ulcers (6,7,16). In this regard, Chicharro-Alcántara et al. (17) argue that the administration of this substance is based on the ability of the high concentrations of platelet-derived growth factor to promote the regeneration of epithelial and endothelial cells. Furthermore, as stated by Xia et al. (10), since autologous PRP preparations are well tolerated by patients, their administration is safe and causes few adverse reactions. In view of the aforementioned, the present case was based on the hypothesis that the administration of PRP activated with ozone and fibrin membranes could be used as a complementary treatment for phlebostatic ulcers.
In the reported patient, complete healing of her ulcer was observed in a short period of time, and this is similar to what has been reported in other studies with a larger number of patients in which PRP has also been used (6,7). Concerning conventional treatments, such as compressive therapies, some studies report healing times of at least three to six months (18,19).
In the present case, no adverse reactions related to the administered therapy were reported, which is consistent with what is found in the literature describing that the administration of PRP is generally safe (6-8,11).
Likewise, the patient reported a reduction in pain and improvement in her overall quality of life, which is in agreement with Suthar et al. (6) and
Salazar-Álvarez et al. (7), whose studies showed that treated patients also experienced improvement in the perception of pain associated with the injury and in their quality of life. In similar studies, it was also observed that patients who received PRP as a treatment for acute ulcers and surgical wounds had a statistically significant reduction in the use of analgesics (20).
The management of the reported case was satisfactory considering that ulcer closure was achieved by administering PRP activated with ozone and fibrin membranes for the first time. The patient complied with all the scheduled interventions and did not report any serious adverse reactions; likewise, the staff in charge of administering the treatment performed adequately to ensure that the intervention was safe and caused as little discomfort as possible to the patient.
Some of the main limitations of this case report include the lack of direct quantification of the size of the ulcer during the course of the treatment, which, together with the pictures provided, would offer further evidence of the result obtained. To validate the results of the present case, more in-depth and controlled research is needed, with randomized clinical trials and a larger sample size.
Conclusions
The results of the present case showed that the combined administration of PRP activated with ozone and fibrin membranes for the treatment of phlebostatic ulcers is a useful, feasible, and safe option. Moreover, an improvement in the patient’s quality of life could be observed after the intervention.
Patient’s perspective
At first, the patient reported being worried about the injury she had been suffering for 4 months in her left lower limb, since it had affected her quality of life, considering that she was subject to a daily treatment plan that had an economic and family impact due to the cost of the medical supplies and the need to travel to a specialized center to receive the treatment, which compromised her family dynamics.
With this treatment, the patient perceived that her lesion closed in a short time and consequently her quality of life improved rapidly, enabling her to engage in other tasks that she was unable to perform due to the discomfort caused by the lesion.
Ethical considerations
The present case was prepared with the approval of the patient, who gave her written and verbal consent for the disclosure of all information obtained by the physician during her treatment in order to evaluate the efficacy and safety of the treatment and to prepare reports and publications.
Conflict of interest
None stated by the authors.
Funding
None stated by the authors.
Acknowledgments
To the patient and her relatives, and to the health care personnel involved in the study.
References
1.Greer N, Foman N, MacDonald R, Dorrian J, Fitzgerald P, Rutks I, et al. Advanced Wound Care Therapies for Non-Healing Diabetic, Venous, and Arterial Ulcers: A Systematic Review. Ann Intern Med. 2013;159(8):532-42. https://doi.org/ts5.
2.Nelzen O. Prevalence of venous leg ulcer: the importance of the data collection method.
Phlebolymphology. 2008;15(4):143-50.
3.Zolotukhin IA, Seliverstov EI, Shevtsov YN, Avakiants IP, Nikishkov AS, Tatarintsev AM, et al. Prevalence and Risk Factors for Chronic Venous Disease in the General Russian Population. Eur J Vas Endovasc Surg. 2017;54(6):752-8. https://doi.org/gcspds.
4.San Sebastian KM, Lobato I, Hernandez I. Efficacy and safety of autologous platelet rich plasma for the treatment of vascular ulcers in primary care: phase III study. BMC Fam Pract. 2014;15:211. https://doi.org/f8k8s2.
5.Bonkemeyer-Millan S, Gan R, Townsend PE. Venous Ulcers: Diagnosis and Treatment. Am Fam Physician. 2019;100(5):298-305.
6.Suthar M, Gupta S, Bukhari S, Ponemone V. Treatment of chronic non-healing ulcers using autologous platelet rich plasma: a case series. J Biomed Sci. 2017;24(1):16. https://doi.org/f9vppg.
7.Salazar-Álvarez AE, Riera-del Moral LF, García-Arranz M, Álvarez-García J, Concepción-
Rodriguez N, Riera-de-Cubas L. Uso de plasma rico en plaquetas para cicatrización de úlceras crónicas de miembros inferiores. Actas Dermosifiliogr. 2014;105(6):597-604. https://doi.org/f2rsrz.
8.Driver VR, Hanft J, Fylling CP, Beriou JM. A prospective, randomized, controlled trial of autologous platelet rich plasma for the treatment of diabetic foot ulcers. Ostomy Wound Manage. 2006;52(6):68-87.
9.Andia I, Abate M. Platelet-rich plasma: underlying biology and clinical correlates. Regen Med. 2013;8(5):645-58. https://doi.org/gqgcfx.
10.Xia Y, Zhao J, Xie J, Lv Y, Cao DS. The Efficacy of Platelet-Rich Plasma Dressing for Chronic Nonhealing Ulcers: A Meta-Analysis of 15 Randomized Controlled Trials. Plast Reconstr Surg. 2019;144(6):1463-74. https://doi.org/ghkhpk.
11.Anitua E, Aguirre JJ, Algorta J , Ayerdi E, Cabezas AI, et al. Effectiveness of autologous preparation rich in growth factors for the treatment of chronic cutaneous ulcers. J Biomed Mater Res B Appl Biomater. 2008;84(2):415-21. https://doi.org/bpzbcr.
12.Valacchi G, Bocci V. Studies on the biological effects of ozone: 10. Release of factors from ozonated human platelets. Mediators Inflamm. 1999;8(4-5):205-9. https://doi.org/fcgxs4.
13.Re L, Martínez-Sánchez G, Pérez-Davison G, Sirito M. Role of Ozone/Oxygen in Fibroblast Growth Factor Activation. Discovering the Facts. International Journal of Ozone Therapy. 2010;9:55-8.
14.Schwartz A, Martínez-Sánchez G, Re L. Factores de crecimiento derivados de plaquetas y sus aplicaciones en medicina regenerativa. Potencialidades del uso del ozono como activador. Revista Española de Ozonoterapia. 2011;1(1):54-73.
15.Xie T, Ye J, Rerkasem K, Mani R. The venous ulcer continues to be a clinical challenge: an update. Burns trauma. 2018;6:18. https://doi.org/gdr6mz.
16.Kanwar S, Agarwal N. PRP: A MIRACLE FOR CHRONIC ULCERS. International Journal of Scientific Research. 2020;9(10):41-4. https://doi.org/j5h9.
17.Chicharro-Alcántara D, Rubio-Zaragoza M, Damiá-Giménez E, Carrillo-Poveda JM, Cuervo-
Serrato B, Peláez-Gorrea P, et al. Platelet Rich Plasma: New Insights for Cutaneous Wound Healing Management. J Funct Biomater. 2018;9(1):10. https://doi.org/gp4bj4.
18.O’Meara S, Cullum N, Nelson EA, Dumville JC. Compression for venous leg ulcers. Cochrane Database Syst Rev. 2012;11(11):CD000265. https://doi.org/j5jb.
19.De Carvalho MR, Peixoto BU, Silveira IA, Oliveria BGRB. A Meta-analysis to Compare Four-layer to Short-stretch Compression Bandaging for Venous Leg Ulcer Healing. Ostomy Wound Manage. 2018;64(5):30-7.
20.Carter MJ, Fylling CP, Parnell LKS. Use of platelet rich plasma gel on wound healing: A systematic review and meta-analysis. Eplasty. 2011;11:e38.