Use of botulinum toxin as a preoperative adjuvant in incisional hernia repair performed using the Rives-Stoppa technique in a pediatric patient: a case report
Uso de toxina botulínica como adyuvante prequirúrgico en reparación de hernia incisional realizada con técnica de Rives-Stoppa en un paciente pediátrico: reporte de caso
Paula Andrea Quintero-Garzón1 Jose Ricardo Torres-Pulido2
Jose Ricardo Torres-Pulido2 Fernando Augusto Escobar2
Fernando Augusto Escobar2
1 Universidad Nacional de Colombia - Bogotá Campus - Faculty of Medicine - Bogotá D.C. - Colombia.
2 Empresa Social del Estado Hospital Universitario San Rafael de Tunja - Pediatric Surgery Service - Tunja - Colombia.
Open access
Received: 06/03/2023
Accepted: 11/10/2023
Corresponding author: Paula Andrea Quintero-Garzón. Facultad de Medicina, Universidad Nacional de Colombia. Bogotá D.C. Colombia. Email: pquinterog@unal.edu.co.
Keywords: Incisional Hernia; Surgical Procedures, Operative; Botulinum Toxins, Type A; Pediatrics (MeSH).
Palabras clave: Hernia incisional; Procedimientos quirúrgicos operativos; Toxinas botulínicas Tipo A; Pediatría (DeCS).
How to cite: Quintero-Garzón PA, Torres-Pulido JR, Escobar AF. Use of botulinum toxin as a preoperative adjuvant in incisional hernia repair performed using the Rives-Stoppa technique in a pediatric patient: a case report. Rev. Fac. Med. 2024;72(1):e107644. English. doi: https://doi.org/10.15446/revfacmed.v72n1.107644.
Cómo citar: Quintero-Garzón PA, Torres-Pulido JR, Escobar FA. [Uso de toxina botulínica como adyuvante prequirúrgico en reparación de hernia incisional realizada con técnica de Rives-Stoppa en un paciente pediátrico: reporte de caso]. Rev. Fac. Med. 2024;72(1):e107644. English. doi: https://doi.org/10.15446/revfacmed.v72n1.107644.
Copyright: Copyright: ©2024 Universidad Nacional de Colombia. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, as long as the original author and source are credited.
Abstract
Introduction. Although incisional hernia is a rare condition in pediatric patients, it is relevant because of its possible complications and esthetic and functional impact.
Case presentation. A 14-year-old boy with a history of acute appendicitis with generalized peritonitis required multiple surgical interventions in July 2020 and was readmitted to the emergency department of a secondary care hospital located in the department of Boyacá (Colombia) two months later due to intestinal obstruction. Despite receiving conservative management, no improvement was observed, so he was referred to a university hospital located in Boyacá, where he underwent an exploratory laparoscopy after 7 days of treatment, during which lysis of abdominal adhesions and the resection of a segment of the intestine were performed. In October 2020, the patient was taken again to the emergency department due to intestinal obstruction, requiring surgical treatment (lysis of multiple peritoneal adhesions and abdominal adhesions in the proximal ileum). Six months later, during the second postoperative follow-up, an incisional hernia of 10cm in diameter was evidenced. Given the large size of the hernia and its characteristics, it was decided to repair it surgically using the Rives-Stoppa technique including the administration of botulinum toxin type A as a preoperative adjuvant, achieving the recovery of the abdominal wall anatomy without any complications.
Conclusion. While currently there is no treatment of choice for the repair of incisional hernias in pediatric patients, the Rives-Stoppa technique is an effective and safe therapeutic option. Likewise, botulinum toxin type A has proven to be an effective preoperative adjuvant for reducing the risk of complications.
Resumen
Introducción. Si bien la hernia incisional es una condición poco frecuente en pacientes pediátricos, es relevante por sus posibles complicaciones e impacto estético y funcional.
Presentación del caso. Niño de 14 años con antecedente de apendicitis aguda con peritonitis generalizada que en julio de 2020 requirió múltiples intervenciones quirúrgicas y quien dos meses después fue reingresado al servicio de urgencias de un hospital de segundo nivel del departamento de Boyacá (Colombia) por obstrucción intestinal, donde, a pesar de recibir manejo conservador, no se observó mejoría, por lo cual fue remitido a un hospital universitario de Boyacá, donde, luego de 7 días de manejo médico, fue llevado a laparoscopia exploratoria en la que se realizó lisis de adherencias abdominales y resección de un segmento del intestino. En octubre de 2020 fue llevado nuevamente al servicio de urgencias por obstrucción intestinal, requiriendo de nuevo manejo quirúrgico (lisis de múltiples adherencias peritoneales y adherencias abdominales en el íleon proximal). Durante el segundo control postoperatorio, 6 meses después, se evidenció hernia incisional de 10cm de diámetro. Dado el gran tamaño de la hernia y sus características, se decidió reparar quirúrgicamente con técnica de Rives-Stoppa con aplicación de toxina botulínica de tipo A como adyuvante prequirúrgico, logrando recuperación de la anatomía de la pared abdominal sin complicaciones.
Conclusión. Si bien actualmente no hay un tratamiento de elección para la reparación de hernias incisionales en pacientes pediátricos, la técnica de Rives-Stoppa representa una opción terapéutica eficaz y segura. Igualmente, la toxina botulínica de tipo A demostró ser un adyuvante prequirúrgico efectivo para la reducción del riesgo de complicaciones.
Introduction
Incisional hernias (IH) are a rare postsurgical complication in pediatric patients, with an incidence of 2.1% to 5.2%, which is very low as compared to adults (up to 50-54%).1-3 IHs involve a loss of the normal anatomy and functionality of the abdominal wall, causing an aesthetic and functional impact, and may also induce pain or discomfort over the area where they are located, visible or palpable swelling, skin problems, or symptoms of bowel obstruction or strangulation.1 Consequently, they should be identified and corrected early in order to avoid major complications such as hernia incarceration and bowel strangulation.3
At present, given the low incidence rates of IHs in children, there are few studies that allow establishing the method of choice for their repair in the pediatric population.1,2
In view of the above, the following is a case report of a pediatric patient who underwent IH repair using the Rives-Stoppa technique and in whom botulinum toxin was used as a preoperative adjuvant.
Case presentation
A 14-year-old boy underwent an open appendectomy in July 2020 due to acute perforated appendicitis with generalized peritonitis that required two peritoneal lavages and a stay in the pediatric intensive care unit for 11 days. In September 2020, the patient was admitted to the emergency department of the Hospital Regional de Chiquinquirá Empresa Social del Estado, a secondary care institution located in Chiquinquirá (Boyacá, Colombia), due to intestinal obstruction, and received non-surgical management with fluid therapy, bowel rest, and indication to walk for as long as possible. However, since no satisfactory response to this treatment was observed and due to the occurrence of several episodes of bile vomiting, the patient was referred to a tertiary care university hospital in Tunja, Boyacá. On admission physical examination, normal vital signs and pain in the abdomen without signs of peritonitis were reported; in addition, no abnormal findings were reported in the admission laboratory tests (complete blood count, renal function tests, serum electrolyte panel, and amylase test).
Given his medical history, clinical manifestations and the foregoing findings, the patient was diagnosed with partial intestinal obstruction that did not require surgery. Accordingly, the patient was treated with a nasogastric tube on free drainage; infusion of lactated Ringer’s + 5mL potassium at 90mL/hour; intravenous ondansetron 5mg every 8 hours, omeprazole 20mg every 12 hours, and dipyrone 1.5mg every 6 hours; and chewing gum to stimulate bowel function. After 7 days, and since his clinical condition did not improve, he was taken to an exploratory laparotomy in which lysis of abdominal adhesions was performed; in addition, in the presence of proximal ileum stenosis caused by abdominal adhesions, the affected intestinal segment was resected and end-to-end anastomosis was performed. The patient had no perioperative complications and was discharged on the fifth postoperative day.
In October 2020, the patient was taken again to the emergency department of the same hospital in Tunja due to a new intestinal obstruction. On that occasion, non-surgical management was once again initiated, but since no satisfactory response was obtained, four days later he was admitted to the hospitalization service. On the following day, an exploratory laparotomy was performed, during which multiple peritoneal adhesions and abdominal adhesions in the proximal ileum that caused 90% obstruction of the intestinal lumen were lysed. Ten days after surgery and upon adequate progress, he was discharged from the hospital.
At the follow-up appointment held 8 days after discharge, the patient was in good general condition and showed adequate healing of the surgical wound, so a second follow-up appointment was scheduled to be held after 6 months. The physical examination of this second follow-up showed an IH with circular borders and approximately 10cm in diameter (Figure 1), so surgery was indicated. Furthermore, in order to have a better characterization of the hernia, a computed axial tomography (CAT) scan was performed, which showed a 7cm eventration with diastasis recti. It should be noted that, due to administrative issues, this imaging test was performed 4 months after the last follow-up.
Figure 1. Incisional hernia in pediatric patient. A) patient in dorsal decubitus; B) lateral view.
Two months after performing the CAT scan and given the size of the hernia and the presence of diastasis recti, botulinum toxin administration was indicated in a new follow-up appointment, as recommended by Palmisano.4 First, the infiltration points were marked (Figure 2) and then the toxin was reconstituted by diluting 100 units in 2-4mL of sterile saline, obtaining a concentration of 25-50 units/mL. Afterwards, using ultrasound as a guide, the subcutaneous cellular tissue, three abdominal muscle planes (external oblique, internal oblique, and transversus abdominus) and a deeper plane including peritoneum and bowel loops were delimited. Finally, under ultrasound guidance, in each muscle plane (external oblique, internal oblique, and transversus), the previously marked points were infiltrated, administering 50 units/mL of the reconstituted toxin on the left and right sides of the abdomen, for a total of 100 units/mL.
Figure 2. Points of botulinum toxin administration.
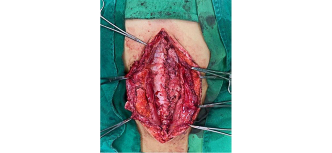
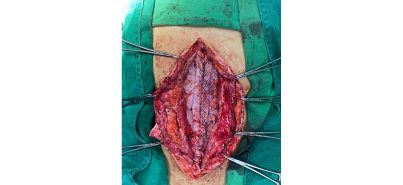
Thirty-five days later, surgical repair was performed with the Rives-Stoppa technique using the following approach: first, the scar from one of the previous laparotomies was resected, and then a dissection by planes was performed down to the abdominal cavity and the adhesions of the abdominal wall were released. At this point, we proceeded as follows: dissection of the posterior sheath of the right and left sides of the rectus abdominis muscle was performed (Figure 3), the posterior sheath was closed with PDS 0 suture (Figure 4), the ULTRAPRO® mesh was placed and fixed with PDS 2-0 suture (Figure 5), and the anterior sheath was closed with approximation of both sides of the rectus abdominis muscle to the midline using PDS 0 suture. Finally, the abdominal cavity was closed by layers.
Figure 3. Dissection of the posterior sheath of the rectus abdominis muscle.
Figure 4. Closure of the posterior sheath of the rectus abdominis muscle.
There were no complications during the procedure, and the patient progressed satisfactorily in the postoperative period, with tolerance to oral intake of liquids and food and adequate pain control with non-steroidal anti-inflammatory drugs. As a result, the patient was discharged two days after the procedure.
In the first postoperative follow-up appointment, 8 days after discharge, the patient was found to be in good general condition and did not have abdominal pain. On physical examination, a hypertrophic laparotomy scar was detected with no abdominal flaccidity or protrusion of abdominal contents; no other relevant findings were reported.
Figure 5. ULTRAPRO® mesh placement.
Discussion
IH is defined as an abdominal wall defect at the site of a surgical incision that is diagnosed mainly on physical examination (89%-100% of cases), but can also be detected by ultrasound.1,3 This is consistent with the present case, in which the patient was diagnosed during a physical examination.
Although the literature on this complication in the pediatric population is limited, it has been reported that the incidence of IH in children is very low (2.1-5.2%).1-3 Similarly, Mullassery et al.1 found that the risk of developing IH is much lower after laparoscopic surgery compared to laparotomy. This supports what happened in the case of our patient, who developed IH after three laparotomies.
IHs usually present as a lump in the surgical incision area. In this regard, Eeftinck-Schattenkerk et al.,3 in a study of 2 055 children under 3 years of age undergoing abdominal surgery at the medical centers of the University of Amsterdam (the Netherlands) between 1998 and 2018, found that of the 107 participants who presented with IH, 68% had an asymptomatic swelling as their only symptom. This is consistent with what happened in our case since the patient’s only symptom was the protrusion. Likewise, patients with IH may present with intermittent pain on exertional activities or, in cases of large hernias diagnosed late, develop intestinal obstruction due to the incarceration of hernial contents.1,3 In our case, despite dealing with a large hernia, early diagnosis prevented the occurrence of serious complications.
In the adult population, there are well known risk factors for the presentation of IH, including increasing age, obesity, preoperative chemotherapy, and smoking.1 In the pediatric population, surgical site infection, preterm birth and a history of stomas are the main risk factors, with surgical site infection being the factor with the highest association.3 Moreover, Mullassery et al.1 reported that an age below 6 months is a possible risk factor. On the other hand, although no data were found on the relationship between open appendectomy and IH, we consider that the main factor influencing the appearance of IH in our patient was the multiple surgical procedures he had undergone.
In 2021, Roca-Domínguez et al.4 published a guideline for the management of ventral and midline incisional hernias in which they state that, regardless of size, all hernias should be treated surgically since the risk-benefit ratio of surgery is more favorable compared to watchful waiting. This, together with the large size of the hernia observed in our patient, supports the decision to perform a surgical repair.
To deal with this condition, especially large hernias, it may be necessary to perform an imaging test that allows an adequate characterization of the abdominal wall defect, with CT being the method of choice as it provides a dimension of the size of the defect, identifies its content, evaluates the abdominal muscles and the rest of the cavity, and predicts the need for pre- or transoperative adjuvant techniques.5 Based on these facts, a CAT scan of the abdomen was requested for our patient, showing diastasis recti, which, added to the contracture of the abdominal muscles detected in the physical examination, allowed an adequate preoperative planning, taking advantage of the available adjuvant techniques.
Currently, the surgical technique of choice for the management of abdominal hernias in the adult population is the Rives-Stoppa technique because it allows recovering the anatomy of the abdominal wall by reconstructing the midline with the least possible tension, which has been shown to reduce relapses or complications.2 On the other hand, as mentioned above, the literature in the pediatric population is limited; in this sense, a PubMed search yielded 23 studies related to the topic, but only one of them contained all the search terms (“incisional”, “hernia”, “pediatric”, “patient”) and was relevant to this report.6
Even though IH repair has been little explored in pediatric surgery, primary closure2 has long been preferred in order to avoid invasive procedures or the placement of foreign material. However, since large defects or situations in which primary closure becomes difficult may be encountered, there is a need to study new techniques with different surgical approaches (open, laparoscopic) and using prosthetic material.
One of these treatment options is laparoscopic repair with intraperitoneal mesh placement,6 a procedure that has the advantage of being minimally invasive, avoids extensive dissection of the abdominal wall, and allows maintaining the integrity and functionality of the abdominal wall. However, some complications have been described in the adult population related to the location of the prosthetic material, as it can cause visceral adhesions or fistulization, and even cases of iatrogenic enterotomy have been reported due to the need for extensive adhesiolysis,7 but there are still no studies that follow up pediatric patients who undergo this procedure in the long term. This technique was not considered in our patient because the surgical incision in question was a midline laparotomy which allowed us to use the approach and remove the skin flap with hypertrophic scarring and give the patient a more esthetic result.
The Rives-Stoppa technique has already been reported as an option for the treatment of IHs in the pediatric population,2 and its advantages are similar to those described in the adult population. Furthermore, muscle dissection allows medialization of the rectus abdominis muscles up to 2cm,2 which is a great advantage when treating a large defect, as in the case of our patient, since this favors tension-free closure of the abdominal cavity, thus reducing the possibility of complications.
In a study reviewing the records of adult patients undergoing the Rives-Stoppa technique in a hospital in Iran between 1993 and 2003 (n=86), Yaghoobi-Notash et al.8 concluded that this is the most promising technique for IH repair, with a low recurrence rate (5.8%). Similarly, in a study of 176 patients who underwent IH repair using the Rives-Stoppa technique between 1998 and 2003, Mehrabi et al.9 reported a recurrence rate of 1.1%, which confirms that this is an effective and safe technique. Based on the foregoing and taking into account the patient’s surgical history and the great involvement of the abdominal wall, it was decided to use the Rives-Stoppa technique.
In order to reduce complications such as intra-abdominal hypertension, respiratory failure, or early recurrence of the defect derived from the surgical repair of large hernias (>10cm), adjuvant techniques have been proposed such as the use of botulinum toxin A, which has been tested in the repair of these hernias in adults. It consists of the infiltration of this substance into the abdominal muscles to cause a flaccid and reversible muscle paralysis that leads to a lengthening of the muscle by 2.5cm on each side and a decrease in its thickness of approximately 1cm, thus modifying the size of the defect.4,10 These effects are at their maximum expression between days 30 to 45 after toxin administration,4 at which time surgical repair should ideally be performed.
In a case report of a 7-year-old patient with giant ventral hernia repaired by progressive preoperative pneumoperitoneum technique and use of botulinum toxin, Rombaldi et al.11 reported that the only side effect noted was abdominal wall flaccidity, which was observed at the 3-month follow-up appointment and disappeared at the 6-month follow-up examination, but otherwise it was a successful treatment that allowed tension-free closure. These results allow us to conclude that botulinum toxin therapy is safe in pediatric patients despite the fact that there is still not much literature reporting its use.
It has also been demonstrated that the use of botulinum toxin as a preoperative adjuvant has a favorable impact on surgical outcomes and long-term treatment effectiveness.4 In the case reported here, the large hernia and muscle contracture were major risk factors for a possible tension closure of the abdominal cavity, so it was decided to use botulinum toxin. Although we do not have exact measurements of the thickness reduction and lengthening of the muscle, the improvement of the contracture after the administration of the toxin was evident in the physical examination, thus achieving the positive effects expected at the time of the surgery.
Conclusions
The Rives-Stoppa technique for IH repair is an effective and safe therapeutic option in pediatric patients, as it achieves the main objective when repairing these defects and restores the anatomy of the abdominal wall. In addition, the administration of botulinum toxin type A was found to be an effective preoperative adjuvant that reduces complications associated with tension closures of the abdominal wall. However, studies are needed to evaluate the long-term effectiveness and safety of this procedure in this population.
Ethical considerations
For the preparation of this case report, the patient’s legal guardian signed the informed consent form authorizing the use of the patient’s data.
Conflicts of interest
None stated by the authors.
Funding
None stated by the authors.
Acknowledgments
None stated by the authors.
References
1.Mullassery D, Pedersen A, Robb A, Smith N. Incisional hernia in pediatric surgery - experience at a single UK tertiary centre. J Pediatr Surg. 2016;51(11):1791-4. https://doi.org/f8933p.
2.Molina-Caballero AY, Pérez-Martínez A, Goñi-Orayen C. Abdominal hernia repair using the Rives-stoppa technique: An abdominal reconstruction. Cir Pediatr. 2021;34(3):164-7.
3.Eeftinck-Schattenkerk LD, Musters GD, Coultre SEL, de Jonge WJ, van Heurn LE, Derikx JPM. Incisional hernia after abdominal surgery in infants: A retrospective analysis of incidence and risk factors. J Pediatr Surg. 2021;56(11):2107-12. https://doi.org/mqkk.
4.Roca-Domínguez MB, Gutiérrez-Ferreras AI, Mayagoitia González JC. Guía para el manejo de la hernia ventral y hernia incisional medial. Rev Hispanoam Hernia. 2021;9(2):80-7. https://doi.org/mq3m.
5.Inoue M, Aoi S, Taniguchi A, Sakai K, Higashi M, Fumino S, et al. Laparoscopic intraperitoneal onlay mesh for pediatric incisional hernia—a case report. Surg Case Rep. 2017;3(1):122. https://doi.org/mq3z.
6.Soare AM, Cârţu D, Nechita SL, Andronic O, Șurlin V. Complications of Intraperitoneal Mesh Techniques for Incisional Hernia - A Systematic Review. Chirurgia (Bucur). 2021;116(Suppl 6):S36-S42.
7.Yaghoobi-Notash A, Yaghoobi-Notash A, Seied-Farshi J, Ahmadi-Amoli H, Salimi J, Mamarabadi M. Outcomes of the rives-stoppa technique in incisional hernia repair: Ten years of experience. Hernia. 2006;11(1):25-9. https://doi.org/bsb96h
8.Mehrabi M, Jangjoo A, Tavoosi H, Kahrom M, Kahrom H. Long-term outcome of Rives-stoppa technique in complex ventral incisional hernia repair. World J Surg. 2010;34(7):1696-701. https://doi.org/bjxx2v.
9.Grove TN, Kontovounisios C, Montgomery A, Heniford BT, Windsor AC, Warren OJ, et al. Perioperative optimization in complex abdominal wall hernias: Delphi Consensus statement. BJS Open. 2021;5(5):zrab082. https://doi.org/grzfkw.
10.Palmisano EM. Application of Botulinum Toxin A as a Preoperative Adjuvant Technique in Large Abdominal Wall Defects. Acta Scientific Clinical Case Reports 2.3. 2021;2(3):22-4.
11.Rombaldi MC, Neto WF, Holanda FC, Cavazzola LT, Fraga JC. Ventral hernia secondary to giant omphalocele in a child: Combined approach of botulinum toxin and preoperative progressive pneumoperitoneum. Hernia. 2019;24(6):1397-400. https://doi.org/mr5w.
 Jose Ricardo Torres-Pulido2
Jose Ricardo Torres-Pulido2 Fernando Augusto Escobar2
Fernando Augusto Escobar2