LipStaT® Surgery, A Novel Technique for the Treatment of Gummy Smile: Case Report
LipStaT®, Una novedosa técnica quirúrgica para el tratamiento de la sonrisa gingival, reporte de casos
DOI:
https://doi.org/10.15446/aoc.v10n2.84452Palabras clave:
Gingival overgrowth, Gingival diseases, Stomatognathic diseases, Maxillofacial abnormalities, Esthetics dental (en)sobrecrecimiento gingival, enfermedades gingivales, enfermedades estomatognáticas, anormalidades maxilofaciales, estética dental (es)
Descargas
Introduction: The lip stabilization technique (LipStaT®) is a novel surgical approach for the management of gummy smile. It is an outpatient technique, minimally invasive, with low risk of morbidity and low incidence of complications. The goal of the technique is to reduce the excessive gingival display during smile. Objective: to describe the LipStaT® technique including its indications, preoperative evaluation, surgical approach and patient post procedure care instructions. Clinical Cases: the authors present two female patients, aged 20 and 31 years, with excessive gingival display (over 3mm) and with experiences of failures with other procedures. The LipStaT® technique allowed to achieve aesthetic, harmonic and functional results. Conclusion: The LipStaT® technique is a safe outpatient procedure that allows to obtain predictable results, which are well accepted by patients.
Introducción: La técnica de estabilización labial (LipStaT®), es un novedoso abordaje quirúrgico para el manejo de la sonrisa gingival. Es una técnica ambulatoria, mínimamente invasiva, con baja morbilidad e incidencia de complicaciones. La meta de la técnica es reducir la excesiva cantidad de encía que se visualiza durante la sonrisa. Objetivo: Describir la técnica LipStaT® incluyendo sus indicaciones, evaluación preoperatoria, abordaje quirúrgico y las indicaciones posteriores a la intervención. Presentación del caso: Los autores presentan dos pacientes, mujeres, entre 20 y 31 años, con visualización excesiva de la encía de más de 3mm al sonreír y con experiencias de fracasos con otros procedimientos. La técnica LipStaT® permitió lograr un resultado estético, armónico y funcional. Conclusión: Este es un procedimiento seguro, ambulatorio, que permite obtener resultados predecibles y bien aceptados por los pacientes.
LipStaT® Surgery, A Novel Technique for the Treatment of Gummy Smile: Case Report
LipStaT®, Una novedosa técnica quirúrgica para el tratamiento de la sonrisa gingival, reporte de casos
Gummy Smile and LipStat® Technique
Isabella Manzur Villalobos, Eilien Gisek Tovío Martínez, Eliana Marcela Guzmán Menco, Adel Martínez Martínez
|
Recibido |
Aprobado |
Publicado |
|
05/01/2020 |
19/05/2020 |
15/07/2020 |
Citación sugerida: Manzur-Villalobos I, Tovío-Martínez EG, Guzmán Menco EM, Martínez-Martínez A. LipStaT® Surgery A Novel Technique for the Treatment of Gummy Smile: Case Report. Acta Odonto Col. 2020; 10(2): xx-xx. Available in: https://revistas.unal.edu.co/index.php/actaodontocol/article/view/84452
Abstract
Introduction: The lip stabilization technique (LipStaT®) is a novel surgical approach for the management of gummy smile. It is an outpatient technique, minimally invasive, with low risk of morbidity and low incidence of complications. The goal of the technique is to reduce the excessive gingival display during smile. Objective: to describe the LipStaT® technique including its indications, preoperative evaluation, surgical approach and patient post procedure care instructions. Clinical Cases: the authors present two female patients, aged 20 and 31 years, with excessive gingival display (over 3mm) and with experiences of failures with other procedures. The LipStaT® technique allowed to achieve aesthetic, harmonic and functional results. Conclusion: The LipStaT® technique is a safe outpatient procedure that allows to obtain predictable results, which are well accepted by patients.
Key words: Gingival overgrowth; Gingival diseases; Stomatognathic diseases; Maxillofacial abnormalities; Esthetics dental.
Resumen
Introducción: La técnica de estabilización labial (LipStaT®), es un novedoso abordaje quirúrgico para el manejo de la sonrisa gingival. Es una técnica ambulatoria, mínimamente invasiva, con baja morbilidad e incidencia de complicaciones. La meta de la técnica es reducir la excesiva cantidad de encía que se visualiza durante la sonrisa. Objetivo: Describir la técnica LipStaT® incluyendo sus indicaciones, evaluación preoperatoria, abordaje quirúrgico y las indicaciones posteriores a la intervención. Presentación del caso: Los autores presentan dos pacientes, mujeres, entre 20 y 31 años, con visualización excesiva de la encía de más de 3mm al sonreír y con experiencias de fracasos con otros procedimientos. La técnica LipStaT® permitió lograr un resultado estético, armónico y funcional. Conclusión: Este es un procedimiento seguro, ambulatorio, que permite obtener resultados predecibles y bien aceptados por los pacientes.
Palabras clave: sobrecrecimiento gingival; enfermedades gingivales; enfermedades estomatognáticas; anormalidades maxilofaciales; estética dental.
Introduction
The smile has always been considered an important factor in the physical beauty of a person. Most patients think a good smile is important to making a good first impression. Due to this, the smile plays a decisive role in aesthetics and beauty (1). Authors say a good smile depends on several factors such as: upper lip, number of teeth and gums shown, shape and teeth position, among others (2). There must be harmony and balance between the teeth, the gums and the lips. An acceptable smile is shown when the lower edge of the upper lip and the gingival margin of the central incisor screen are 1-2 mm; in contrast to an excessive gingival display or also known as a “rubbery smile” where the distance is 4 mm or more, which is considered unattractive (3).
The possible etiologies of excessive gingival visualization or excessive gingival display (EGD) would be: 1) a delay in the eruption, which means that the gum cannot complete the apical migration on the maxillary teeth at 1 mm coronal to the cement-enamel junction, 2) vertical excess of the maxilla where there is a dimension enlarged vertical, 3) hypermobile upper lip or a short upper lip, when smiling the lips move in a superior apical direction which exposes the teeth and excessive gingiva, 4) proportion of the teeth size and 5) gingival health (4). To determine other factors that are not related to hyperfunction of the levator superior lip muscle, certain characteristics must be taken into account, where the facial proportions must be symmetrical in the three-thirds horizontal, without identifying a greater proportion of the lower third, which could characterize excessive vertical maxillary growth (5).
The approach taken to treat gummy smile would depend on the problem’s etiology. Various treatments and techniques are applied depending on the case. In some cases, it can be resolved by cutting the excess gum and the crown cosmetic lengthening with a gingivectomy or gingivoplasty with an electrosurgical unit, laser surgery or with a manual scalpel (6). In other cases, the problem is due to the maxillary bone, therefore orthognathic surgery must be performed, and in some others, such as when the lip moves in an apical direction and the teeth keep a good length and shape of the crown, then an injection of botulinum toxin type A can be applied to the upper lip or the replacement of the upper lip (7).
The lip stabilization technique or LipStaT® is performed by limiting the retractions of the smile muscles, such as zygomaticus, orbicularis labia, elevator of the angle or elevation of the lip (8). This is achieved by decreasing the vestibule by removing a mucous band, which allows the lip to descend and stabilize it in that position with sutures, preventing the elevator muscle from stretching in an apical direction and, therefore, the patient shows less gum during a dynamic smile (9).
The lip repositioning procedure was first described by Rubinstein and Kostianovsky in 1973 during a plastic medical surgery. The first time this procedure was used in dentistry was in 2006 after being modified by Rosenblatt and Simon (10,11). Furthermore, in 2015, Bhola introduced the LipStaT® technique, this author reported a new classification for the excessive gingival display (EGD) and provides guidelines and indications of when to use the surgical technique according to the etiology and clinical findings of the EGD. The new classification indicates the LipStaT® technique when there is an EGD for bony maxillary excess, and the gingival excess is between 2 mm to 8 mm, if it is > 8 mm, orthognathic surgery should be recommended. Another indication is when an excessive mobility of the maxillary lip is described, it was classified by Bhola as EGD(E) and subclassified according to the amount of gingival display as 1(1-3mm), 2 (8-12mm) and 3 (10-15mm) (12).
Therefore, this technique it is a minimally invasive and novel procedure that seeks to improve the appearance of the smile by repositioning the upper lip and decreasing the amount of gum showed during dynamic smile. This surgical procedure does not generate sensory or motor alterations, can be performed in a very short time, with local anesthesia in which immediate results are obtained.
The aim of this article is to describe two clinical cases of gummy smile patients treated with LipStaT® technique, exploring the indications, diagnosis, surgical approach and postoperative management.
Cases Report
Case 1
A 20-year-old female patient attended the School of Dentistry, University of Cartagena, Colombia, for presenting aesthetic dissatisfaction in her smile because of the amount of gum displayed every time she smiled (figure 1A). The patient did not report a previous history of orthodontic or cosmetic dental treatment. No relevant family and personal medical history for the case (ASA I according to American Society of Anesthesiologists), she denied tobacco use. An extraoral and intraoral clinical examination was performed to evaluate the degree of gingival excess that the patient presented and to classify the smile. First, the facial height is evaluated measuring the three-thirds facials to determine bony maxillary excess when the lower third is longer to other two thirds. In this patient, the facial height was normal (figure 1B). The upper lip was measured from the subnasale to the inferior border of it, when it measures 20 mm it is considered within the normal limit, in the patient there was no deficiency in the length of the maxillary lip (figure 1C). It was not necessary to take radiographs or previous tomography scans of patients since the protocol requires them when the patient has excessive maxillary growth and, therefore, to determine if there is a need for orthognathic surgery.
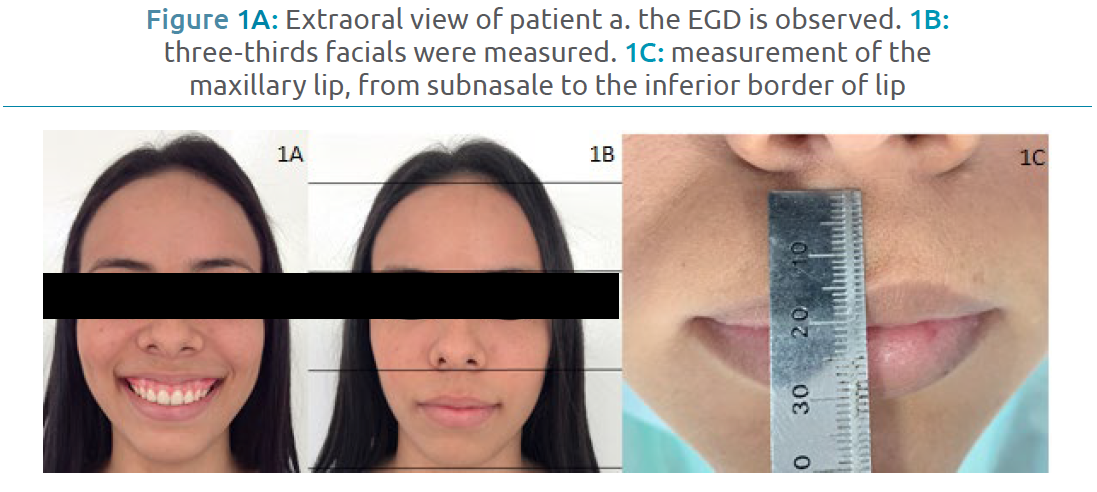
Figure 1A: Extraoral view of patient a. the EGD is observed. 1B: three-thirds facials were measured. 1C: measurement of the maxillary lip, from subnasale to the inferior border of lip
The intraoral examination revealed that there was a high smile with 3 mm to 4 mm of gingival exposure measured with a periodontal probe, with extension of the smile showing up to the first upper molars and normal occlusion, the crowns of the dental organs had an adequate proportion in height and width (figure 2A). According to the clinical examination findings the excessive gingival display was classified with EGD (E) subclass 2. The treatment option presented was the lip stabilization technique or LipStaT®.
The procedure was explained to the patient who authorized the treatment and signed the informed consent. Surgical intervention was performed under local anesthesia using the anterior superior alveolar technique with 4% articaine with 1:100,000 epinephrine. The mucosal band was marked, the lateral extension was determined by the horizontal extension during the dynamic smile and the width depended on the EGD measurement (3 to 4 mm), the height of the incision is twice this measurement (6 to 8 mm) (figure 2B). Partial thickness incisions was raised up to the first premolars and the mucous band is removed (figure 2C).

Figure 2A: Intraoral view of patient 2 with maxillary gingival excess of 4mm resulting in a gummy smile. 2B: The mucosal band width was of 6 to 8 mm. 2C: The mucosal band was removed by debridement without compromising the underlying periosteum
Suturing was initiated at the midline, interrupted sutures with PTF 5-0 are taken that confront the edges of the incisions, allowing a correct alignment and avoiding inadequate healing. Immediate extraoral postoperative showed promising results. Antibiotics and anti-inflammatories were prescribed, accompanied by Fitoestimoline® (Triticum vulgare oral gel) 3 times a day. The patient was advised to apply ice in the postoperative period and to minimize lip movement for 7 days. Controls were performed at 8, 15 and 30 days. The results were satisfactory, evidencing reduction in gingival exposure during a dynamic smile, after which the patient expressed satisfaction with the treatment and her smile (figure 3). The level of satisfaction was assessed by a direct question with an answer of yes or no in all postsurgical sessions (9-15-30 days).
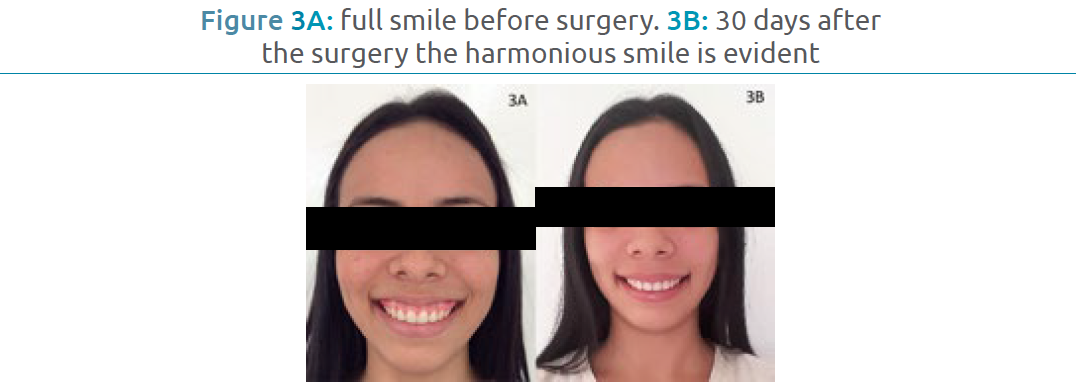
Figure 3A: full smile before surgery. 3B: 30 days after the surgery the harmonious smile is evident
Case 2
A 31-year-old female patient attended to the School of Dentistry, University of Cartagena, Colombia, for a consultation regarding cosmetic nonconformity due to a gummy smile. The patient reports a previous history of orthodontic treatment, gingival plastic surgery and cosmetic dental treatment. Without relevant family and personal medical history (ASA I according to American Society of Anesthesiologists), no smoker. An extraoral and intraoral clinical examination was performed, the facial height was normal. The upper lip no show deficiency in the length of the maxillary lip. The intraoral examination revealed there is a high smile with 4 mm of gingival exposure (figure 4A). According to the clinical examination the gummy smile was classified as EGD (E) subclass 2.
A treatment plan involving LipStaT® technique was proposed because the patient reported previous gingivectomy that eventually, after several months, grew again showing excessive gingiva during her smile. Using an anesthesia technique of the anterosuperior alveolar branches in the area of bilateral maxillary canines with 2% Lidocaine with 1:80,000 epinephrine, we proceeded to demarcate the mucosal band that will be removed, from the mucogingival line to the base of sulcus of the first premolar through contralateral first premolar. An oval-shaped mucosal incision was performed following the above-described mark, the mucosal band was removed by debridement without compromising the underlying periosteum (figure 4B).
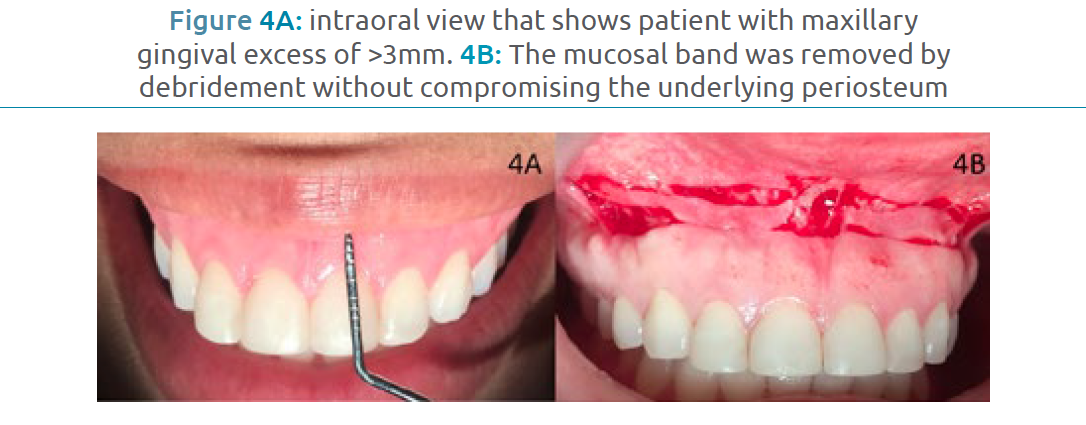
Figure 4A: intraoral view that shows patient with maxillary gingival excess of >3mm. 4B: The mucosal band was removed by debridement without compromising the underlying periosteum
The mucosal flap was advanced and sutured to the edge of the mucogingival line by a continuous suture with polyglycolic acid 4.0 (figure 5A). Postoperative indications included not brushing the area and rinsing with 0.12% chlorhexidine with 0.05% CPC for 10 days, amoxicillin 500 mg, nimesulide 100 mg and Fitoestimoline® (Triticum vulgare oral gel) 3 times a day. Post-surgical controls are performed at 8, 15 and 30 days. The patient presented satisfactory esthetic results with evident reduction of her gingival smile to less than 3 mm (figure 5B).

Figure 5A: Immediate intraoral postoperative of patient with lip reposition, using continued suture with polyglycolic acid. 5B: Smile 30 days after the lip reposition surgery
Ethical Aspects
The authors considered the ethical aspects of resolution 8430 of 1993. The clinical interventions respected the bioethics principles of autonomy, beneficence, non-maleficence and justice in patients. The informed consent was explained by the authors and after being read by the patients it was signed. The publication of the case is made respecting the identity of the patients or any data that allows the identification of the subjects.
Discussion
Beauty is a continuous search in man, since it is considered an attribute that can open doors in society in all fields, which is because patients go to the dentist to achieve a harmonious appearance on their face (13). For this reason, it is imperative to consider the psychosocial impact the smile generates for each individual, since it can work as a rule to make a good first impression. The amount of gingival display is among the aspects that comprise the aesthetics of the smile, playing an important role in being attractive to others (14). In 1973 Rubenstein and Kostianovsky were the first to introduce such a technique, also in 2015 Bhola described the lip stabilization technique (LipStaT®) allowing it to be a surgical technique, very used in last decade which allows reducing the force generated by the lifting muscles of the upper lip, thus showing the patient a smile with a more pleasant aesthetic (12).
There are recent epidemiological studies that show that the rubbery smile affects approximately 10% of the population between 20 and 30 years old, and also affirm that the average length of the maxillary lip is 20-22 mm in young adult women and 22-24 mm in young adult men (10). Being more common among women (10); which goes accordingly to the proposed cases that belong to an age range of 20 and 31 years old, female sex and maxillary lip length of 22mm. Some authors comment it is very useful to keep the upper lip frenulum and two strips are removed from the mucosa, one on each side of the frenulum, since it allows them to preserve the position of the lip midline, preserves the lips symmetry and it decreases the morbidity associated with the procedure, they also state that when a person smiles, the entire crown of the upper central incisors and 1 mm of the attached gum will be noticed, however when there is a greater amount of exposed gum (2-3 mm) it may be cosmetically acceptable as long as the gum is not too visible (10). In the reported cases, despite the fact the patients did not retain the upper lip frenulum, lip symmetry and midline were maintained, on the other hand, an acceptable gingival smile was observed when exposing more than one inch of gum.
Foudah in 2019 reported a case of lip repositioning on 25-year-old female patient with a follow up of 4 years that evidence the results have been stable during time too with satisfactory results (10), which is similar to our case not only in the age range or gender but also with the technique done. Therefore, this shows that the lip repositioning technique could maintain a good gingival display of the smile through time, which differs from some techniques such as gingivectomy that could grow back again and show excessive gingival display some months later.
Among the advantages of the LipStaT® technique are: it was designed to be shorter, less aggressive and have fewer postoperative complications when compared to other surgical methods, it still gives satisfactory results, as some authors show such as Rosenblatt, Bhola and Humayun et al (11,12,15). However, those patients who present excessive gingival smile due to presenting excessive maxillary prominence are contraindicated for this type of procedure, especially the ones having an EGD more than 8mm (12). Therefore, a correct diagnosis is necessary prior to the selection of the indicated technique (16). In this case, the patients treated for the development of this article were ideal candidates for present excessive gums and short lips, which caused aesthetic disagreements, with an EGD of 4mm and previous surgical procedures trying to solve this problem with no satisfactory results.
Proper diagnosis of etiologic factors is the first step in selecting the appropriate treatment protocol. Currently, several treatment alternatives have been proposed, among which the following stand out: orthognathic surgery and esthetic crown lengthening with lip repositioning, sometimes it must be complemented from gingivectomies, gingivoplasties, frenillectomies, corticotomies in the maxillary bone, subcutaneous lip dissection to myotomies of the upper lip elevator muscle. Depending on the diagnosis of the patient, each case can be treated with a single technique or combination of those already mentioned (2,16). For the cases presented in this article, the removal of the mucous bands that ran from the mucogingival line to the end of the vestibule was performed, accompanied by frenillectomy, such as Bhola et al (12) and Foudah et al (10) performed on their cases.
When comparing the LipStaT® technique with other surgical treatments such as orthognathic surgery, the advantages include that it allows to have precision in predicting the results, minimizes the treatment time, is a minimally invasive surgery, less traumatic, and presents a faster postoperative, with fewer complications and is comfortable for the patient. In spite of everything, like any other surgical technique, it can have complications and risks that include a small portion of attached gingiva, which can cause problems in flap design, stabilization and suturing, on the other hand, due to surgical stress, canker sores may appear, presence of suture dehiscence, infections, hemorrhages, keloid or hypertrophic scarring. After following this technique, it can be determined the results obtained are stable during time, allowing it to be an excellent alternative (15). In the reported cases, both aesthetic and functional parameters were reached, which was what the patients wanted, in this way the patients were pleased and satisfied with the treatment and the results.
In conclusion the LipStaT® technique is good surgical approach that should be used in cases of several gingival smile, especially in the ones that cannot be solved with a simple gingivectomy. After reading this article, the reader should be able to understand the characteristics and usefulness of the LipStaT® technique in patients with gingival smile; understand how the surgical procedure is performed.
Acknowledgments
We thank each of the participants in this clinical case who allowed us to get a correct diagnosis and treatment of the case presented.
Contribution of the authors
Adel Martínez Martínez: preparation of the manuscript; Isabella Manzur Villalobos, Eilien Gisek Tovío Martínez, Eliana Marcela Guzmán Menco, Adel Martínez Martínez: preparation of the manuscript and writing; Isabella Manzur Villalobos: preparation of the manuscript translation; Eilien Gisek Tovío Martínez, Adel Martínez Martínez: field work and writing.
Conflicts of interest
The authors declare no conflict of interest.
References
1. Diaspro A, Cavallini M, Piersini P, Sito G. Gummy smile treatment: proposal for a novel corrective technique and a review of the literature. Aesthetic Surgery Journal. 2018; 38(12): 1330–1338. https://doi.org/10.1093/asj/sjy174
2. Sánchez I, Gaud-Quintana S, Stern J. Modified Lip Repositioning with Esthetic Crown Lengthening: A Combined Approach to Treating Excessive Gingival Display. The International Journal of Periodontics & Restorative Dentistry. 2017; 37(1): e130–e134. https://doi.org/10.11607/prd.3124
3. Longo E, Frosecchi M, Marradi L, Signore A, de Angelis N. Guided periodontal surgery: a novel approach for the treatment of gummy smile. A case report. The International Journal of Esthetic Dentistry. 2019; 14(4): 384–392. https://pubmed.ncbi.nlm.nih.gov/31549104/
4. Gibson MP, Tatakis DN. Treatment of Gummy Smile of Multifactorial Etiology: A Case Report. Clinical Advances in Periodontics. 2017; 7(4): 167–173. https://doi.org/10.1902/cap.2017.160074
5. Sriphadungporn C, Chamnannidiadha N. Perception of smile esthetics by laypeople of different ages. Progress in Orthodontics. 2017; 18(1): 1–8. https://doi.org/10.1186/s40510-017-0162-4
6. Mantovani M, Souza E, Marson F, Corrêa G, Progiante P, Silva C. Use of modified lip repositioning technique associated with esthetic crown lengthening for treatment of excessive gingival display: A case report of multiple etiologies. Journal of Indian Society of Periodontology. 2016; 20(1): 82–87. https://doi.org/10.4103/0972-124X.164746
7. Ramesh A, Vellayappan R, Ravi S, Gurumoorthy K. Esthetic lip repositioning: A cosmetic approach for correction of gummy smile–A case series. Journal of Indian Society of Periodontology. 2019; 23(3): 290–294. https://doi.org/10.4103/jisp.jisp_548_18
8. Verardi, S, Ghassemian M, Bazzucchi A, Pavone AF. Gummy Smile and Short Tooth Syndrome-Part 2: Periodontal Surgical Approaches in Interdisciplinary Treatment. Compendium of Continuing Education in Dentistry. 2016; 37(4): 247–251. https://pubmed.ncbi.nlm.nih.gov/27136119/
9. Obero G, Chaudhry S, Yadav S, Talwar S, Verma M. Correction of gummy smile using digital smile designing in conjugation with crown lengthening by soft-tissue diode laser. Journal of Dental Lasers. 2017; 11(1): 14–18. https://doi.org/10.4103/2321-1385.208947
10. Foudah M. Lip repositioning: An alternative to invasive surgery a 4 year follow up case report. The Saudi Dental Journal. 2019; 31(Suppl): S78–S84. https://doi.org/10.1016/j.sdentj.2019.02.030
11. Rosenblatt A, Simon Z. Lip repositioning for reduction of excessive gingival display: a clinical report. International Journal Periodontics Restorative Dent. 2006; 26: 433–437. https://pubmed.ncbi.nlm.nih.gov/17073353/
12. Bhola M, Fairbairn PJ, Kolhatkar S, Chu SJ, Morris T, de Campos M. LipStaT: The lip stabilization technique—indications and guidelines for case selection and classification of excessive gingival display. International Journal Periodontics Restorative Dent. 2015; 35: 549–559. https://doi.org/10.11607/prd.2059
13. Carbajal N. Reposicionamiento labial para el tratamiento de la sonrisa gingival. Revisión de la literatura. Revista Científica Odontológica. 2019; 7(2): 97–107. https://doi.org/10.21142/2523-2754-0702-2019-97-107
14. Faus-Matoses V, Faus-Matoses I, Jorques-Zafrilla A, Faus-Llácer V. Lip repositioning technique. A simple surgical procedure to improve the smile harmony. Journal of Clinical and Experimental Dentistry. 2018; 10(4): e408– e412. https://doi.org/10.4317/jced.54721
15. Humayun N, Kolhatkar S, Souiyas J, Bhola M. Mucosal coronally positioned flap for the management of excessive gingival display in the presence of hypermobility of the upper lip and vertical maxillary excess: A case report. Journal of Periodontology. 2010; 81(12): 1858–1863. https://doi.org/10.1902/jop.2010.100292
16. Bhimani R, Sofia N. Lip repositioning, aesthetic crown lengthening, and gingival depigmentation: A combined approach for a gummy smile makeover. Journal of Cutaneous and Aesthetic Surgery. 2019; 12(4): 240–243. https://doi.org/10.4103/JCAS.JCAS_25_19
Referencias
Diaspro A, Cavallini M, Piersini P, Sito G. Gummy smile treatment: proposal for a novel corrective technique and a review of the literature. Aesthetic Surgery Journal. 2018; 38(12): 1330–1338. https://doi.org/10.1093/asj/sjy174
Sánchez I, Gaud-Quintana S, Stern J. Modified Lip Repositioning with Esthetic Crown Lengthening: A Combined Approach to Treating Excessive Gingival Display. The International Journal of Periodontics & Restorative Dentistry. 2017; 37(1): e130–e134. https://doi.org/10.11607/prd.3124
Longo E, Frosecchi M, Marradi L, Signore A, de Angelis N. Guided periodontal surgery: a novel approach for the treatment of gummy smile. A case report. The International Journal of Esthetic Dentistry. 2019; 14(4): 384–392. https://pubmed.ncbi.nlm.nih.gov/31549104/
Gibson MP, Tatakis DN. Treatment of Gummy Smile of Multifactorial Etiology: A Case Report. Clinical Advances in Periodontics. 2017; 7(4): 167–173. https://doi.org/10.1902/cap.2017.160074
Sriphadungporn C, Chamnannidiadha N. Perception of smile esthetics by laypeople of different ages. Progress in Orthodontics. 2017; 18(1): 1–8. https://doi.org/10.1186/s40510-017-0162-4
Mantovani M, Souza E, Marson F, Corrêa G, Progiante P, Silva C. Use of modified lip repositioning technique associated with esthetic crown lengthening for treatment of excessive gingival display: A case report of multiple etiologies. Journal of Indian Society of Periodontology. 2016; 20(1): 82–87. https://doi.org/10.4103/0972-124X.164746
Ramesh A, Vellayappan R, Ravi S, Gurumoorthy K. Esthetic lip repositioning: A cosmetic approach for correction of gummy smile–A case series. Journal of Indian Society of Periodontology. 2019; 23(3): 290–294. https://doi.org/10.4103/jisp.jisp_548_18
Verardi, S, Ghassemian M, Bazzucchi A, Pavone AF. Gummy Smile and Short Tooth Syndrome-Part 2: Periodontal Surgical Approaches in Interdisciplinary Treatment. Compendium of Continuing Education in Dentistry. 2016; 37(4): 247–251. https://pubmed.ncbi.nlm.nih.gov/27136119/
Obero G, Chaudhry S, Yadav S, Talwar S, Verma M. Correction of gummy smile using digital smile designing in conjugation with crown lengthening by soft-tissue diode laser. Journal of Dental Lasers. 2017; 11(1): 14–18. https://doi.org/10.4103/2321-1385.208947
Foudah M. Lip repositioning: An alternative to invasive surgery a 4 year follow up case report. The Saudi Dental Journal. 2019; 31(Suppl): S78–S84. https://doi.org/10.1016/j.sdentj.2019.02.030
Rosenblatt A, Simon Z. Lip repositioning for reduction of excessive gingival display: a clinical report. International Journal Periodontics Restorative Dent. 2006; 26: 433–437. https://pubmed.ncbi.nlm.nih.gov/17073353/
Bhola M, Fairbairn PJ, Kolhatkar S, Chu SJ, Morris T, de Campos M. LipStaT: The lip stabilization technique—indications and guidelines for case selection and classification of excessive gingival display. International Journal Periodontics Restorative Dent. 2015; 35: 549–559. https://doi.org/10.11607/prd.2059
Carbajal N. Reposicionamiento labial para el tratamiento de la sonrisa gingival. Revisión de la literatura. Revista Científica Odontológica. 2019; 7(2): 97–107. https://doi.org/10.21142/2523-2754-0702-2019-97-107
Faus-Matoses V, Faus-Matoses I, Jorques-Zafrilla A, Faus-Llácer V. Lip repositioning technique. A simple surgical procedure to improve the smile harmony. Journal of Clinical and Experimental Dentistry. 2018; 10(4): e408– e412. https://doi.org/10.4317/jced.54721
Humayun N, Kolhatkar S, Souiyas J, Bhola M. Mucosal coronally positioned flap for the management of excessive gingival display in the presence of hypermobility of the upper lip and vertical maxillary excess: A case report. Journal of Periodontology. 2010; 81(12): 1858–1863. https://doi.org/10.1902/jop.2010.100292
Bhimani R, Sofia N. Lip repositioning, aesthetic crown lengthening, and gingival depigmentation: A combined approach for a gummy smile makeover. Journal of Cutaneous and Aesthetic Surgery. 2019; 12(4): 240–243. https://doi.org/10.4103/JCAS.JCAS_25_19
Cómo citar
APA
ACM
ACS
ABNT
Chicago
Harvard
IEEE
MLA
Turabian
Vancouver
Descargar cita
Licencia
Derechos de autor 2020 EILIEN TOVIO MARTINEZ, ADEL MARTINEZ MARTINEZ, ISABELLA MANZUR VILLALOBOS, ELIANA GUZMAN

Esta obra está bajo una licencia internacional Creative Commons Atribución-NoComercial-SinDerivadas 4.0.
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
- Los autores/as conservarán sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la licencia Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación esta revista.
- Los autores/as podrán adoptar otros acuerdos de licencia no exclusiva de distribución de la versión de la obra publicada (p. ej.: depositarla en un archivo telemático institucional o publicarla en un volumen monográfico) siempre que se indique la publicación inicial en esta revista.
- Se permite y recomienda a los autores/as difundir su obra a través de Internet (p. ej.: en archivos telemáticos institucionales o en su página web) antes y durante el proceso de envío, lo cual puede producir intercambios interesantes y aumentar las citas de la obra publicada. (Véase El efecto del acceso abierto).
- Una vez sometido el artículo no se aceptaran cambios respecto a la incorporación o retiro de autores.