Publicado
Dashboard for assessing patient flow management in hospital institutions
Tablero de control para evaluar la gestión de los flujos de pacientes en instituciones hospitalarias
DOI:
https://doi.org/10.15446/dyna.v91n232.111259Palabras clave:
management control; patient flow; hospital management; indicators; dashboard (en)control de gestión; flujo de pacientes; gestión hospitalaria; indicadores; tablero de control (es)
Descargas
Proactive control of hospital processes has a significant influence on patient performance and satisfaction. The objective of the research is to develop a dashboard for the evaluation of patient flow management in hospital institutions. Based on a descriptive quantitative study, a procedure is proposed for the development of a dashboard for the evaluation of patient flow management in hospital institutions, structured in five stages and nine steps, including procedures for the identification of key variables and aggregation of indicators. A dashboard was developed for the General Surgery service of a Clinical Surgical Teaching Hospital, which is composed of 18 indicators, six synthetic indexes and one comprehensive indicator. Among the positive implications for healthcare managers is the possibility of monitoring and comparing strategies with a process vision between different departments in support of proactive and strategic decision making in order to improve hospital performance.
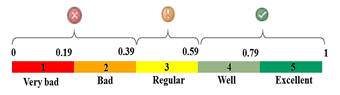
El control proactivo de los procesos hospitalarios influye de forma significativa en el rendimiento y satisfacción de los pacientes. El objetivo de la investigación es desarrollar un tablero de control para la evaluación de la gestión del flujo de pacientes en instituciones hospitalarias. Se desarrolló un estudio cuantitativo descriptivo y se analizaron metodologías precedentes. Se elaboró un proceder para la confección de un tablero de control para la evaluación de la gestión de los flujos de pacientes en instituciones hospitalarias, estructurado en cinco etapas y nueve pasos, incluye procedimientos para la identificación de variables clave y agregación de indicadores. Se confeccionó un tablero de control para el servicio de Cirugía General de un hospital Clínico Quirúrgico Docente, que está compuesto por 18 indicadores, 6 índices sintéticos y un indicador integral. El indicador integral obtuvo un valor de 0,79 (4), lo que es muestra de la eficacia de las acciones implementadas durante el despliegue del modelo de mejora. Entre las implicaciones positivas para los gestores sanitarios está la posibilidad de monitorear las estrategias con una visión de proceso.
Referencias
Jabalera, M., Pons, M., Gómez, E., and del Castillo, M., Hacia la excelencia en gestión hospitalaria. Un modelo de gestión estratégica, Journal of Healthcare Quality Research, 34(3), pp. 148-153, 2019. DOI: https://doi.org/10.1016/j.jhqr.2019.02.005 DOI: https://doi.org/10.1016/j.jhqr.2019.02.005
Adriana-Roussel, P., Impacto de un modelo de gestión de la calidad de un servicio de inmunización del Hospital de Alta Complejidad. El Cruce, Salud, Ciencia y Tecnología, 2(44), pp. 1-14, 2022. DOI: https://doi.org/10.56294/saludcyt202244 DOI: https://doi.org/10.56294/saludcyt202244
Sánchez-Suárez, Y., Instrumento metodológico para la gestión de flujos de pacientes de instituciones hospitalaria, PhD Thesis, Facultad de Ciencias Técnicas, Universidad de Matanzas, Matanzas, Cuba, 2023.
Bouckaert, N., Van den Heede, K., and Van de Voorde, C., Improving the forecasting of hospital services: a comparison between projections and actual utilization of hospital services, Health Policy, 122(7), pp. 728-736, 2018. DOI: https://doi.org/10.1016/j.healthpol.2018.05.010 DOI: https://doi.org/10.1016/j.healthpol.2018.05.010
Herlina, Madjid, M., Rusman, A.D.P., Sari, R.W., Noer, N.B., and Rivai, F., The application of the fast method needed in improving hospital services, Enfermería Clínica, 30, pp. 240-243, 2020. DOI: https://doi.org/10.1016/j.enfcli.2020.06.055 DOI: https://doi.org/10.1016/j.enfcli.2020.06.055
Aluvalu, R., Mudrakola, S., Maheswari, U., Kaladevi, A.C., Sandhya, M.V.S., and Rohith-Bhat, C., The novel emergency hospital services for patients using digital twins, Microprocessors and Microsystems, 98, art. 104794, 2023. DOI: https://doi.org/10.1016/j.micpro.2023.104794 DOI: https://doi.org/10.1016/j.micpro.2023.104794
Bahalkeh, E., Chiam, T.C., and Yih, Y., An interpretable clustering classification approach for assessing and adjusting hospital service lines, Healthcare Analytics, 4, art. 100255, 2023. DOI: https://doi.org/10.1016/j.health.2023.100255 DOI: https://doi.org/10.1016/j.health.2023.100255
Georgescu, I., Management control literature and French public hospitals, Health Policy, 111(3), pp. 324-327, 2013. DOI: https://doi.org/10.1016/j.healthpol.2013.06.014 DOI: https://doi.org/10.1016/j.healthpol.2013.06.014
Acero-Moreno, A.M., Ordoñez-Paredes, B.A., Toloza-Guardias, H.P., and Vega-Palmera, B., Análisis estratégico para la empresa Imbocar, seccional Valledupar – Colombia. Región Científica, 2(1), art. 202395, 2023. DOI: https://doi.org/10.58763/rc202395 DOI: https://doi.org/10.58763/rc202395
Fatima, T., and Elbanna, S., Advancing sustainable performance management in the hospitality industry: a novel framework based on a health-inclusive balanced scorecard, Tourism Management Perspectives, 48, art. 101141, 2023. DOI: https://doi.org/10.1016/j.tmp.2023.101141 DOI: https://doi.org/10.1016/j.tmp.2023.101141
Franklin, A., Gantela, S., Shifarraw, S., Johnson, T.R., Robinson, D.J., King, B.R., Mehta, A.M., Maddow, C.L., Hoot, N.R., Nguyen, V., Rubio, A., Zhang, J., and Okafor, N.G., Dashboard visualizations: supporting real-time throughput decision-making, Journal of Biomedical Informatics, 71, pp. 211-221, 2017. DOI: https://doi.org/10.1016/j.jbi.2017.05.024 DOI: https://doi.org/10.1016/j.jbi.2017.05.024
Peralta-Llivipuma, M.R., Erazo-Álvarez, J.C., and Narváez-Zurita, C.I., Cuadro de mando integral, enfoque estratégico al proceso administrativo y educativo, Visionario Digital, 3(2.2), pp. 120-144, 2019. DOI: https://doi.org/10.33262/visionariodigital.v3i2.2.627 DOI: https://doi.org/10.33262/visionariodigital.v3i2.2.627
Sakly, H., and Ben-Jeddou, K., Development and implementation of dashboard in the Pharmacy Department at University Hospital, Le Pharmacien Clinicien, 57(1), pp. 6-15, 2022. DOI: https://doi.org/10.1016/j.phclin.2021.09.002 DOI: https://doi.org/10.1016/j.phclin.2021.09.002
Sánchez-Suárez, Y., Marqués-León, M., Hernández-Nariño, A., y Suárez-Pérez, M.M., Metodología para el diagnóstico de la gestión de trayectorias de pacientes en hospitales, Región Científica, 2(2), art. 2023115, 2023. DOI: https://doi.org/10.58763/rc2023115. DOI: https://doi.org/10.58763/rc2023115
Torres-Moreno, G.C., y Velasco-Peñaloza, J.C., Aplicación de la metodología BMP e instrumentos Lean para evaluación del flujo de pacientes en el área de servicios quirúrgicos. Estudio de caso: hospitales de alta complejidad, Tesis de grado, Ingeniería Industrial, Universidad Santo Tomás, Colombia, 2020.
Manning, L., and Islam, S., A systematic review to identify the challenges to achieving effective patient flow in public hospitals, Int J Health Plann Mgmt, 38(3), pp. 805-828, 2023. DOI: https://doi.org/10.1002/hpm.3626 DOI: https://doi.org/10.1002/hpm.3626
Castillo, C.Y., Patient’s perception of the quality of care in the Ambulatory Surgery Unit of the Polyclinic Hospital of the western area of the Metropolitan Area of Buenos Aires, Salud, Ciencia y Tecnología, 3, art. 504, 2023. DOI: https://doi.org/10.56294/saludcyt2023504. DOI: https://doi.org/10.56294/saludcyt2023504
Lees-Deutsch, L., and Robinson, J., A systematic review of criteria-led patient discharge, J Nurs Care Qual, 34(2), pp. 121-126, 2019. DOI: https://doi.org/10.1097/NCQ0000000000000356 DOI: https://doi.org/10.1097/NCQ.0000000000000356
Alhaider, A., Lau, N., Davenport, P., and Morris, M., Distributed situation awareness: a health-system approach to assessing and designing patient flow management, Ergonomics, 63(6), pp. 682-709, 2020. DOI: https://doi.org/10.1080/00140139.2020.1755061 DOI: https://doi.org/10.1080/00140139.2020.1755061
Duarte-Forero, E.L., y Camacho-Oliveros, M.Á., Planeación de la capacidad hospitalaria: un enfoque desde el flujo de pacientes con Dinámica de Sistemas, INGE CUC, 16(1), pp. 217-233, 2020. DOI: https://doi.org/10.17981/ingecuc.16.1.2020.16 DOI: https://doi.org/10.17981/ingecuc.16.1.2020.16
Broggi, L., Kemmerer, J., Bandriwskyj, C., Fernández, A., Gangoni, C., and Laura, V.H., Characterization of patients and measures implemented during the pandemic in a high complexity hospital in Argentina: an analysis from a nursing perspective, Salud, Ciencia Y Tecnología, 3, art. 513, 2023. DOI: https://doi.org/10.56294/saludcyt2023513 DOI: https://doi.org/10.56294/saludcyt2023513
Tamburis, O., and Esposito, C., Process mining as support to simulation modeling: a hospital-based case study, Simulation Modelling Practice and Theory, 104, art. 102149, 2020. DOI: https://doi.org/10.1016/j.simpat.2020.102149 DOI: https://doi.org/10.1016/j.simpat.2020.102149
Homavazir, Z., Nagappan, B., and Singh, A., Exploring the contribution of engineering in enhancing workflow and efficiency in nursing. Salud, Ciencia y Tecnología, 3(459), pp. 1-9, 2023. DOI: https://doi.org/10.56294/saludcyt2023459 DOI: https://doi.org/10.56294/saludcyt2023459
Sánchez-Suárez, Y., Sánchez-Castillo, V., y Gómez-Cano, C.A., Modelo para la gestión de flujos de pacientes, validado en un servicio de cirugía general. Revista Cubana de Medicina Militar [Online]. 53(1), art. 024022338, 2024. [date of reference March 4th of 2024]. Available at: https://revmedmilitar.sld.cu/index.php/mil/article/download/22338/2477
Keshtkar, L., Rashwan, W., Abo-Hamad, W., and Arisha, A., A hybrid system dynamics, discrete event simulation and data envelopment analysis to investigate boarding patients in acute hospitals, Operations Research for Health Care, 26, art. 100266, 2020. DOI: https://doi.org/10.1016/j.orhc.2020.100266 DOI: https://doi.org/10.1016/j.orhc.2020.100266
Saeedian, M., Sepehri, M.M., Jalalimanesh, A., and Shadpour, P., Operating room orchestration by using agent-based simulation, Perioperative Care and Operating Room Management, 15, art. 100074, 2019. DOI: https://doi.org/10.1016/j.pcorm.2019.100074 DOI: https://doi.org/10.1016/j.pcorm.2019.100074
Tyagi, M., Tyagi, P.K., Singh, S., Sathpathy, S., Kant, S., Gupta, S.K., and Singh, R., Impact of application of queuing theory on operational efficiency of patient registration, Medical Journal Armed Forces India, 79(3), pp. 300-308, 2023. DOI: https://doi.org/10.1016/j.mjafi.2021.06.028 DOI: https://doi.org/10.1016/j.mjafi.2021.06.028
Ludbrook, G.L., and Leaman, E., Cost-Effectiveness in perioperative care: application of Markov modeling to pathways of perioperative care, Value in Health, 25(2), pp. 215-221, 2022. DOI: https://doi.org/10.1016/j.jval.2021.07.018 DOI: https://doi.org/10.1016/j.jval.2021.07.018
Belciug, S., and Gorunescu, F., A hybrid genetic algorithm-queuing multi-compartment model for optimizing inpatient bed occupancy and associated costs, Artificial Intelligence in Medicine, 68, pp. 59-69, 2016. DOI: https://doi.org/10.1016/j.artmed.2016.03.001 DOI: https://doi.org/10.1016/j.artmed.2016.03.001
Dauncey, S.J., Kelly, P.A., Baykov, D., Skeldon, A.C., and Whyte, M.B., Rhythmicity of patient flow in an acute medical unit: relationship to hospital occupancy, 7-day working and the effect of COVID-19. QJM: monthly journal of the Association of Physicians, 114(11), pp. 773-779, 2022. DOI: https://doi.org/10.1093/qjmed/hcaa334 DOI: https://doi.org/10.1093/qjmed/hcaa334
Berg, E., Weightman, A.T., and Druga, D.A., Emergency department operations II: patient flow. Emergency Medicine Clinics of North America, 38(2), pp. 323-337, 2020. DOI: https://doi.org/10.1016/j.emc.2020.01.002 DOI: https://doi.org/10.1016/j.emc.2020.01.002
Medina-León, S.V., Medina-Palomera, A., y González-Ángeles, Á., Reducir tiempos de espera de pacientes en el departamento de emergencias de un hospital utilizando simulación. Industrial Data [Online]. 13(1), pp. 67-76, 2010. [date of reference September 15th of 2023]. Available at: http://www.redalyc.org/articulo.oa?id=81619989010 DOI: https://doi.org/10.15381/idata.v13i1.6170
Gartner, D., and Kolisch, R., Scheduling the hospital-wide flow of elective patients, European Journal of Operational Research, 233(3), pp. 689-699, 2014. DOI: https://doi.org/10.1016/j.ejor.2013.08.026 DOI: https://doi.org/10.1016/j.ejor.2013.08.026
Pellizarri, M., La mejora del flujo de pacientes a través del hospital. Revista ITAES [Online]. 17(1), pp. 11-18, 2015. [date of reference September 15th of 2023]. Available at: https://studylib.es/doc/7753042/la-mejora-del-flujo-de-pacientes-a-trav%C3%A9s-del-hospital
Armony, M., Israelit, S., Mandelbaum, A., Marmor, Y.N., Tseytlin, Y., and Yom-Tov, G.B., On patient flow in hospitals: a data-based queueingscience perspective. Stochastic Systems, 5(1), pp. 146-194, 2015. DOI: https://doi.org/10.1287/14-SSY153 DOI: https://doi.org/10.1287/14-SSY153
Mathews, K.S., and Long, E.F., A conceptual framework for improving critical care patient flow and bed use. Ann Am Thorac Soc, 12(6), pp. 886-894, 2015. DOI: https://doi.org/10.1513/AnnalsATS.201409-419OC DOI: https://doi.org/10.1513/AnnalsATS.201409-419OC
Chen, X., Wang, L., Dingand, J., and Thomas, N., Patient flow scheduling and capacity planning in a smart hospital environment, IEEE Access, 4, pp. 135-148, 2016. DOI: https://doi.org/10.1109/ACCESS.2015.2509013 DOI: https://doi.org/10.1109/ACCESS.2015.2509013
Andersen, A.R., Nielsen, B.F., Reinhardt, L.B., and Stidsen, T.R., Staff optimization for time-dependent acute patient flow, European Journal of Operational Research, 272(1), pp. 94-105, 2019. DOI: https://doi.org/10.1016/j.ejor.2018.06.015. DOI: https://doi.org/10.1016/j.ejor.2018.06.015
Blouin Delisle, C.H., Drolet, R., Hains, M., Tailleur, L., Allaire, N., Coulombe, M., and Vézo, A., Improving interprofessional approach using a collaborative lean methodology in two geriatric care units for a better patient flow, Journal of Interprofessional Education and Practice, 19, pp., 2020. DOI: https://doi.org/10.1016/j.xjep.2020.100332 DOI: https://doi.org/10.1016/j.xjep.2020.100332
Vali, M., Salimifard, K., Gandomi, A.H., and Chaussalet, T.J., Application of job shop scheduling approach in green patient flow optimization using a hybrid swarm intelligence, Computers & Industrial Engineering, 172, art. e108603, 2022. DOI: https://doi.org/10.1016/j.cie.2022.108603 DOI: https://doi.org/10.1016/j.cie.2022.108603
Suárez-Gargallo, C., and Zaragoza-Sáez, P., A comprehensive bibliometric study of the balanced scorecard, Evaluation and Program Planning, 97, art. 102256, 2023. DOI: https://doi.org/10.1016/j.evalprogplan.2023.102256 DOI: https://doi.org/10.1016/j.evalprogplan.2023.102256
Sánchez-Suárez, Y., Trujillo-García, L., Marqués-León, M., y Santos-Pérez, O., Los indicadores de gestión hospitalarias en tiempos de Covid 19. Visionario Digital, 5(4), pp. 58-77, 2021. https://doi.org/10.33262/visionariodigital.v5i4.1901 DOI: https://doi.org/10.33262/visionariodigital.v5i4.1901
Sexton, P., Whiteman, K., George, E.L., Fanning, M., and Stephens, K., Improving PACU throughput using an electronic dashboard: a quality improvement initiative. Journal of PeriAnesthesia Nursing, 37(5), pp. 613-619, 2022. DOI: https://doi.org/10.1016/j.jopan.2021.11.005 DOI: https://doi.org/10.1016/j.jopan.2021.11.005
Alhabib, D., Alumarn, A., and Alrayes, S., Emergency room visualization dashboard user satisfaction in Saudi Arabia, Informatics in Medicine Unlocked, 21, art. 100493, 2020. DOI: https://doi.org/10.1016/j.imu.2020.100493 DOI: https://doi.org/10.1016/j.imu.2020.100493
Kenigsberg, T.Y.A., Hause, A.M., McNeil, M.M., Nelson, J.C., Ann Shoup, J., Goddard, K., Lou, Y., Hanson, K.E., Glenn, S.C., and Weintraub, E.S., Dashboard development for near real-time visualization of COVID-19 vaccine safety surveillance data in the Vaccine Safety Datalink, Vaccine, 40(22), pp. 3064-3071, 2022. DOI: https://doi.org/10.1016/j.vaccine.2022.04.010 DOI: https://doi.org/10.1016/j.vaccine.2022.04.010
Cinelli, C., Somsen, D., Quinn, A., Horn, N., and Murray, R., Implementation of an electronic dashboard for reporting and tracking of health care professional requirements, Journal of the American College of Radiology, 18(1 Part A), pp. 75-78, 2021. DOI: https://doi.org/10.1016/j.jacr.2020.09.021 DOI: https://doi.org/10.1016/j.jacr.2020.09.021
Castillo, V.S., Cano, C.A.G., and Gonzalez-Argote, J., Telemedicine and health applications for health monitoring in rural communities in Colombia: a systematic review. EAI Endorsed Transactions on Pervasive Health and Technology, 9(1), pp. 1-17, 2023. DOI: https://doi.org/10.4108/eetpht.9.3400 DOI: https://doi.org/10.4108/eetpht.9.3400
Hernández-Nariño, A., y Marqués-León, M., Procedimiento de determinación de indicadores. Aplicación a un proceso del Hospital “Mario Muñoz Monroy, Jornada Científica del Hospital “Mario Muñoz Monroy”, Matanzas, Cuba, 2006.
Hernández-Nariño, A., Contribución a la gestión y mejora de procesos en instalaciones hospitalarias del territorio matancero, PhD Thesis, Departamento de Ingeniería Industrial, Universidad de Matanzas “Camilo Cienfuegos”, Matanzas, Cuba, 2010.
Ramos-Castro, G., Gestión del desempeño del Sistema de Ciencia e Innovación enfocado a los procesos académicos en Salud, PhD Thesis, Departamento de Ingeniería Industrial, Universidad de Matanzas, Matanzas, Cuba, 2022.
Afanador-Cubillos, N., Historia de la producción y sus retos en la era actual, Región Científica, 2(1), art. 202315, 2023. DOI: https://doi.org/10.58763/rc202315 DOI: https://doi.org/10.58763/rc202315
Machuca-Contreras, F., Canova-Barrios, C., y Fabián-Castro, M., Una aproximación a los conceptos de innovación radical, incremental y disruptiva en las organizaciones, Región Científica, 2(1), art. 202324, 2023. DOI: https://doi.org/10.58763/rc202324 DOI: https://doi.org/10.58763/rc202324
Cano, C.A.G., Castillo, V.S., Losada, Y.B., and Monje, M.A.B., Analysis of the risks associated with the provision of services in respiratory diseases ward during the COVID 19 pandemic at the Hospital Maria Inmaculada, Salud, Ciencia y Tecnologia, 2, art. 123, 2022. DOI: https://doi.org/10.56294/saludcyt2022123 DOI: https://doi.org/10.56294/saludcyt2022123
Gonzales-Centon, J.M., Chávez-Cubas, W., Berrio-Huillcacuri, J., and Santos-Maldonado, A.B., El crecimiento empresarial y su relación en la rentabilidad de una MYPE del rubro comercial en Arequipa, Perú, Región Científica, 2(1), art. 202387, 2023. DOI: https://doi.org/10.58763/rc202387 DOI: https://doi.org/10.58763/rc202387
García-Peña, M., López-Ocmin, L.S., y Romero-Carazas, R., Control interno de inventario y la gestión de resultados de un emporio comercial de la región de San Martín - Perú. Región Científica, 2(1), art. 202392, 2023. DOI: https://doi.org/10.58763/rc202392 DOI: https://doi.org/10.58763/rc202392
González-López-Valcárcel, B., and Ortún, V., Reconstrucción del sistema sanitario: gobernanza, organización y digitalización. Informe SESPAS 2022, Gaceta Sanitaria, 36, pp. S44-S50, 2022. DOI: https://doi.org/10.1016/j.gaceta.2022.02.010 DOI: https://doi.org/10.1016/j.gaceta.2022.02.010
Chen, H.-F., Hou, Y.-H., and Chang, R.-E., Application of the balanced scorecard to an academic medical center in Taiwan: the effect of warning systems on improvement of hospital performance, Journal of the Chinese Medical Association, 75(10), pp. 530-535, 2012. DOI: https://doi.org/10.1016/j.jcma.2012.07.007 DOI: https://doi.org/10.1016/j.jcma.2012.07.007
Mejías, M., Guarate-Coronado, Y.C., and Jiménez-Peralta, A.L., Inteligencia artificial en el campo de la enfermería: implicaciones en la asistencia, administración y educación, Salud, Ciencia y Tecnología, 2(88), pp. 1-7, 2022. DOI: https://doi.org/10.56294/saludcyt202288 DOI: https://doi.org/10.56294/saludcyt202288
Esquer-Rochin, M.A., Gutierrez-Garcia, J.O., Rosales, J.-H., and Rodriguez, L.-F., Design and evaluation of a dashboard to support the comprehension of the progression of patients with dementia in day centers. International Journal of Medical Informatics, 156, art. 104617, 2021 DOI: https://doi.org/10.1016/j.ijmedinf.2021.104617 DOI: https://doi.org/10.1016/j.ijmedinf.2021.104617
Cómo citar
IEEE
ACM
ACS
APA
ABNT
Chicago
Harvard
MLA
Turabian
Vancouver
Descargar cita
CrossRef Cited-by
1. Ana Maria Chaves Cano, Alfredo Javier Pérez Gamboa. (2024). Artificial intelligence in strengthening health services: a critical analysis of the literatura. Health Leadership and Quality of Life, 3 https://doi.org/10.56294/hl2024.422.
2. Verenice Sánchez Castillo , Carlos Alberto Gómez Cano. (2024). Health education and technological innovation: an unpostponable relationship. Health Leadership and Quality of Life, 3 https://doi.org/10.56294/hl2024.436.
Dimensions
PlumX
Visitas a la página del resumen del artículo
Descargas
Licencia
Derechos de autor 2024 DYNA

Esta obra está bajo una licencia internacional Creative Commons Atribución-NoComercial-SinDerivadas 4.0.
El autor o autores de un artículo aceptado para publicación en cualquiera de las revistas editadas por la facultad de Minas cederán la totalidad de los derechos patrimoniales a la Universidad Nacional de Colombia de manera gratuita, dentro de los cuáles se incluyen: el derecho a editar, publicar, reproducir y distribuir tanto en medios impresos como digitales, además de incluir en artículo en índices internacionales y/o bases de datos, de igual manera, se faculta a la editorial para utilizar las imágenes, tablas y/o cualquier material gráfico presentado en el artículo para el diseño de carátulas o posters de la misma revista.

















