Description of oral-motor development from birth to six years of age
Descripción del desarrollo de los patrones oromotores desde el nacimiento hasta los seis años de edad
DOI:
https://doi.org/10.15446/revfacmed.v62n4.45211Palabras clave:
Feeding, Speech Language and Hearing Sciences, Sucking Behavior, Deglutition, Mastication (en)alimentación, fonoaudiología, conducta en la Lactancia, deglución, masticación. (es)
Descargas
El presente documento expone una investigación bibliométrica referente al desarrollo de las funciones estomatognáticas de respiración, succión, deglución, masticación y habla desde el nacimiento hasta los seis años. La investigación se planteó a través de la recopilación de información dispuesta en la literatura científica en torno al desarrollo de patrones oromotores y su interrelación con factores ambientales y posturales. Se trata de los patrones de sensibilidad, tono y resistencia muscular, uso de instrumentos de alimentación y, finalmente, la anatomía, fisiología y neurología propias de las estructuras del sistema estomatognático. Lo anterior se analizó con el fin de caracterizar cada una de las funciones estomatognáticas. Como resultado, se describen los principales hitos del desarrollo oromotor de cero a seis años de edad. Se concluye que los patrones oromotores surgen de acuerdo con la maduración de las diferentes estructuras y funciones del sistema estomatognático y se destaca la importancia de conocer el proceso normal de desarrollo oromotor dentro del rol fonoaudiológico, a fin de garantizar una adecuada práctica profesional.
DOI: https://doi.org/10.15446/revfacmed.v62n4.45211
REVIEW ARTICLE
Description of oral-motor development from birth to six years of age
Descripción del desarrollo de los patrones oromotores desde el nacimiento hasta los seis años de edad
Rosa Mercedes Sampallo-Pedroza1, Luisa Fernanda Cardona-López1, Karen Eliana Ramírez-Gómez1
1 Departamento de la Comunicación Humana, Facultad de Medicina, Universidad Nacional de Colombia. Bogotá, Colombia.
Correspondence: Rosa Mercedes Sampallo-Pedroza. Departamento de Comunicación Humana. Facultad de Medicina. Universidad Nacional de Colombia. Ciudad Universitaria. Bogotá, Colombia. Telephone: (57 1) 3165000. Extension: 15191. E-mail: rmsampallop@unal.edu.co.
Received: 26/08/2014 Accepted: 15/09/2014
Summary
This document seeks to present bibliometric research into characterizing the behaviors of each of the stomatognathic functions of a child based on developmental age and expected development until the age of six. The investigation collected the information provided in scientific literature regarding the development of oral-motor postural patterns, environmental influences, sensitivity, tone, muscle strength, use of feeding tools, anatomy, physiology, and the neurology of the anatomical structures of the stomatognathic system. As a result, the major milestones of oromotor development from birth to the age of six are described in this document. Also, a more detailed manual was written to be used by Speech-Language Pathologists. The research concludes that oral motor patterns emerge according to the maturation and function of the different stomatognathic structures. It is of prime importance for Speech-Language Pathologists to be experts in normal oromotor development in order to provide the best professional services when treating children in need of feeding, sucking and dysphagia therapy.
Keywords: Feeding; Speech, Language and Hearing Sciences; Sucking Behavior; Deglutition; Mastication (MeSH).
Sampallo-Pedroza RM, Cardona-López LF, Ramírez-Gómez KE. Description of oral motor development from birth to six years of age. Rev Fac Med. 2014;62(4):593-604. https://doi.org/10.15446/revfacmed.v62n4.45211.
Resumen
El presente documento expone una investigación bibliométrica referente al desarrollo de las funciones estomatognáticas de respiración, succión, deglución, masticación y habla desde el nacimiento hasta los seis años. La investigación se planteó a través de la recopilación de información dispuesta en la literatura científica en torno al desarrollo de patrones oromotores y su interrelación con factores ambientales y posturales. Se trata de los patrones de sensibilidad, tono y resistencia muscular, uso de instrumentos de alimentación y, finalmente, la anatomía, fisiología y neurología propias de las estructuras del sistema estomatognático. Lo anterior se analizó con el fin de caracterizar cada una de las funciones estomatognáticas. Como resultado, se describen los principales hitos del desarrollo oromotor de cero a seis años de edad. Se concluye que los patrones oromotores surgen de acuerdo con la maduración de las diferentes estructuras y funciones del sistema estomatognático y se destaca la importancia de conocer el proceso normal de desarrollo oromotor dentro del rol fonoaudiológico, a fin de garantizar una adecuada práctica profesional.
Palabras clave: Alimentación; Fonoaudiología; Conducta en la Lactancia; Deglución; Masticación (DeCS).
Sampallo-Pedroza RM, Cardona-López LF, Ramírez-Gómez KE. Descripción del desarrollo de los patrones oromotores desde el nacimiento hasta los seis años de edad. Rev Fac Med. 2014;62(4):593-604. https://doi.org/10.15446/revfacmed.v62n4.45211.
Introduction
The stomatognathic system is a functional unit made up of a collection of structures, including: the maxillae and mandible bones; the temporomandibular joint and the atloidooccipital articulation; the teeth; the head and neck muscles, the ligaments, the tongue and the lips; organic spaces; the vascular, nervous, and lymphatic systems; and the mucous membrane and the glands. These elements correlate intimately between each other and with the rest of the organism (1), while acting under the control of the nervous system and performing the different functions of the stomatognathic system, of which oromotor patterns stand out, including: respiration, sucking, deglutition (swallowing), mastication (chewing), and speech (2).
The study of the stomatognathic system and of the development processes of oromotor patterns during infancy are, for phonoaudiology, an area of great research interest. The present bibliometric study can be counted in this area. Its general objective is to characterize structural and oral behavior of each of the stomatognathic functions described at different childhood developmental ages and in their normal development up to the age of six. Also, in terms of specific objects, this study aims to recompile the information available in the scientific literature related to the development of oral-motor patterns and of the feeding process, including instruments used in this process. It also aims to create an anatomo-functional description of the anatomical structures of the stomatognathic system and, finally, to develop a manual that brings together the highlights of oromotor development up to the age of six years.
Research background
During the development process of this study, a bibliographical review of the different graduate projects produced in Colombia on the area of phonoaudiology was performed. This was done in order to go over the background in terms of studies whose central concern was the development of oral-motor patterns in children. A total of thirteen documents were reviewed, including undergraduate and postgraduate theses from the Universidad del Valle (3,4), the Corporación Universitaria Iberoamericana (5), Universidad Manuela Beltrán (6-8), Universidad del Rosario (9,10), Escuela Colombiana de Rehabilitación (11,12), and the Universidad Nacional de Colombia (13-16).
Oromotor skills
Oromotor skills involve the functioning of the lips, cheeks, jaw, and tongue, which all play a large role in the child development and are essential in speech and feeding processes. Difficulties in the development of these oral functions can lead to malnutrition and interference in the physical and social development of the child (17). Although this system is ahead compared to other motor systems (it responds to touch stimulation from the seventh week of gestation) the complete refinement of its actions are not reached until the age of six or seven years. (18).
In this process, motor control participates as a central factor. Motor control is described based on a model of the development of neural function from the point of view of the development of the nervous system and the hierarchical control available in it (19). This involves a series of processes of organization and coordination of functional movement (20), some of which are characteristic of physiological mechanisms and others of psychological mechanisms.
Motor learning refers to the way that different motor skills are acquired. This is a process that requires that the subject perform an action in the right moment, precisely when the subject decides that it is convenient, through the recognition of errors in the movement performed followed by its correction (13). Many of the actions necessary for early oral refinement occur during the first years of life (18), given that sensorimotor and cognitive experiences from this age are considered to be the basis for more advanced sensorimotor functions. Physiological ability in the orofacial region involves touch, taste, temperature, and movement.
One of the fundamental principles of the oral sensorimotor system (13) is the motor development process, which consists of development in the first year of life. It includes, at the level of gross motor function, the stabilization of the head and trunk in sitting position with or without help and the initiation of actions with hand-eye coordination (21). Meanwhile, at the oral level, processes are initiated relating to articulation, normalization of the response of the vagus nerve, and the development different planes of tongue movements. In these two planes, a relationship is built from the refinement of movements and the distal-proximal relationship that provides patterns of stabilization and sensitivity that will favor the development of find movements like those performed by the speech organs (22). The relationship also brings together the other orofacial postures, including the surrounding hard and soft tissues.
Furthermore, there are the perceptual abilities, which refer to sensation and proprioception. Also contemplated is neuromusculature, defined by strength, tone, and endurance. The stabilization of the neck, head, jaw, and tongue are also analyzed. Finally, it covers oromotor differentiation, the process of refinement of movement. In the acquisition of oromotor abilities, also included is the selection of appropriate and efficient actions from among a great variety of possible coordination patterns (20). This process of movement refinement is known as motor differentiation (13).
The development of this motor differentiation is a process of movement refinement. It occurs with time and repeated experience; with the diverse physiological abilities that continually, sequentially, and accumulatively progress (13, 18) and are defined by the following criteria: continual —continual development process—, sequential —the development occurs in steps and, although there are similarities, the steps appear uniquely for each individual—, accumulative —the development steps accumulate to create more advanced abilities and more complex movement patterns—.
This process of maturing initiates with vocal play and babbling. Interestingly, repeated babbling (ba/ba/ba) coincides with rhythmic movements produced in other parts of the body and, in addition, it is related with the development of phonological processes, which are indicators of oromotor coordination.
Breathing
From a functional point of view, the structures of the respiratory system can be divided according the flow of air in two zones: the conducting zone and the respiratory zone. Also, it consists of two stages: inspiration and expiration (23).
Inspiration (the entry of air into the lungs) is performed through alpha motor neurons, which stimulate the contraction of the diaphragm and the external intercostal muscles. When the diaphragm contracts, it descends, increasing the cephalocaudal diameter of the thorax and the contraction of the external intercostal muscles that move the ribs outwards and upwards, which increases the anteroposterior size of the rib cage.
Expiration, under normal conditions, is done passively due to the elastic properties of the thoracic cavity. Expiratory movement begins with the relaxation of the inspiratory muscles, which reduces the diameter of the thorax and increases intra-alveolar pressure, favoring, in this way, the exit of air from the lungs. Other components directly associated with respiration include overall body, head and jaw position (18,24).
Swallowing
Swallowing (or deglutition) has been defined as the sequence of coordinated muscle contractions that carries the alimentary bolus or liquids from the oral cavity to the stomach (25,26). It is a complex and integrated neuromuscular activity (2, 27). The maturation of this oral-motor process consists in the refinement of the function of the pharynx and larynx, which depends directly on stability, sensorimotor abilities, and coordination with respiration (13).
During the control of deglutition, three types of variation of positive and negative pressure that impact the bolus have been described. They include: a) positive and negative pressure associated with the muscles of the mouth, pharynx, and esophagus; b) filling and emptying of the bolus into the tract; and c) pressure related to respiration, including variations in subglottic pressure (28).
Normal swallowing includes primitive and mature patterns (2), which obey an ontogenetic classification. In the primitive pattern, the person is capable of completing only one swallowing/sucking sequence per breath. Meanwhile, in the mature model, the person can complete two or more swallows per breath (consecutive swallowing). In this sense, five phases of swallowing can be distinguished (29): the anticipatory stage (placing the food in the mouth)(26), the preparatory stage (manipulating the food in the mouth with the teeth) (25), the oral or lingual stage (25), the pharyngeal stage (25), and the esophageal stage (25).
Change in the development of swallowing patterns are described in terms of alimentary consistency, including liquids, semisolids, and solids (soft and hard) (22).
Sucking
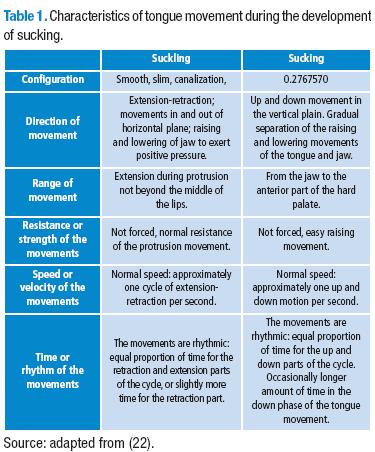
Sucking is known to be the first phase of the ingestion of liquids or soft solids. In can also be a part of the oral phase of swallowing (22). As such, it implies a rhythmic process that originates in utero and is considered to be a reflex after birth (2), one that must be initiated easily and with rhythm, support, strength, and frequency. This process starts with contact of the infant’s mouth with the breasts, a bottle nipple, the fingers, or even a toy. The last two processes are related to non-nutritional sucking, which can calm the infant and leads to body organization (22). In the infantile development of the sucking pattern, two phases are identified (22,30): suckling (29,31) and sucking (13,29,31) (Table 1).
Biting and mastication
Biting is defined as a protective reflex that can be provoked by a series of stimuli, including: olfactory and visual stimuli; touching the posterior third of the palate, the palatal or lingual face of the gums, the pharynx; stimulation of the vagal nerve in the intestinal tract, or the stimulation of the semicircular canals in the inner ear from the rapid movement of the head or body. Biting is necessary for protecting the body from unfamiliar or negative stimuli. Two types of biting are described: the phasic biting and the biting with vertical movements (28). The action of biting, grinding, and chewing the food is a complex physiological act that involves neuromuscular and digestive activities. Like the preparatory phase of deglutition, in which swallowing can take place adequately and without compensatory pressures due to an efficient mastication processes (28), masticatory function has a gradual development that depends of the patterns of growth, development and maturation of the craniofacial complex, the central nervous system, and occlusal guides from the firm and rhythmic approximation of the osteo-dental arcs. In this process, movements in three planes of space are executed: opening, closing, protrusion, retraction, and rotational movements that are unique to mastication.
Mastication is carried out starting with a jaw opening accompanied by an apprehension of the food through a vertical over bit in which the incisors cut a piece of this food. The central nervous system and its proprioceptive functions automatically program, according to previous sensorial information taken by the subject, the opening of the jaw and the strength of the incisors necessary to ingest each food (28).
This stomatognathic function is also a learned act, in which, if the subject is not exposed to food that require clear masticatory action, due to modifications in growth and maxillary development, the mechanics of mastication will not develop efficiently. Mastication also requires the physiological acquirement of rhythmicity in the movements of the jaw, tongue, and facial musculature. This coordination is shown by the possibility of developing the masticatory act and cycle (28).
During this developmental process, two masticatory processes can be differentiated: a) the immature mastication pattern and b) the mature mastication pattern (13). The jaw movements seen during mastication (22) are described in Table 2.
Speech
Understood as a skill of a high level of complexity, requiring several years to be acquired, it continues to be perfected at an adult age. It is also the functional skill in which physiological and phonological skills and the structures of the tongue and oral motor system come together with semantic intent to produce a message (13).
The development of speech is influenced by cognitive and perceptual factors (32). This appreciation, together with the prolonged amount of time necessary for dominating speech, suggests that babies are not doted with the neuromuscular control necessary to produce the gamut of sounds available in their mother tongues and, as a consequence, require strategies that are characteristic of their development for approximating the speech of an adult. These first adaptations provide a window for the state of development of the neuromotor system and cognitive/perceptual processes in infants.
In the acquisition of this process, it is very important to be aware of the development and evolution of the basic postures necessary for speech. These provide an adequate formation of muscle tone and body stability for the respiratory-resonant-articulatory complex (29). Four basic postures are recognized: back postures (0-3 months), elbow patterns (3-6 months), sitting patterns (6-9 months), and standing patterns (9-27 months).
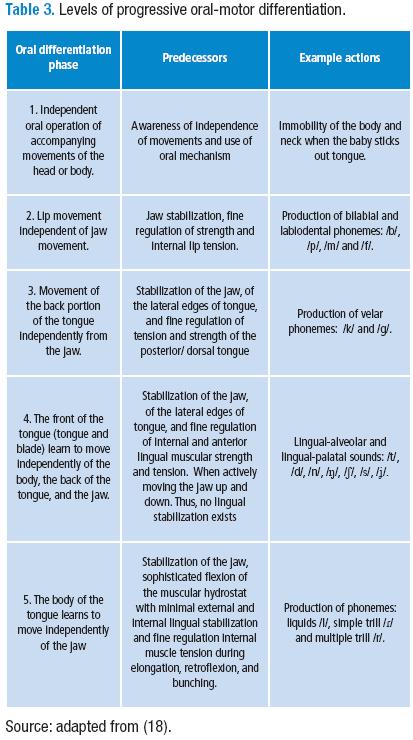
Progressive levels of oral-motor differentiation
In the motor differentiation process, 5 phases (18) can be differentiated. They are described in Table 3.
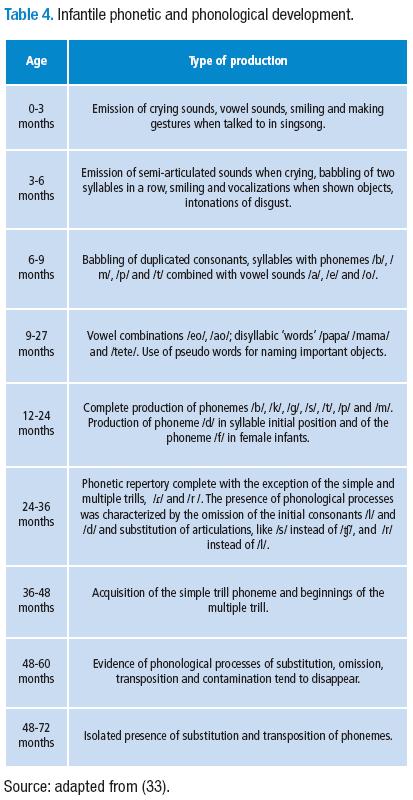
Infantile phonetic and phonological development
The phonetic development and the characterization of sequentiality of the appearance of the phonemes in the lexicon of infantile Spanish has been described from a linguistic point of view (33), presented in Table 4. From an oral-motor development standpoint (18), it starts with movements of the tongue and jaw —low, medium, back, etc; bilabial consonants; and /n/—
The production of the phoneme /s/ requires the front of the tongue to be moved vertically, slightly downwards, approaching the edge between the alveolus and the palate. Furthermore, the tongue is sustained for a moment while the column of air flows forced through the narrow space. In this development process, a relationship can be seen between oral-motor development and the processes of speech (34). This is further explained in Figure 1.
Ambient and postural factors affecting feeding
When speaking about the development of eating processes, an important relationship between the child and their caretaker, who is the one who provides food and ambient stimuli for the child’s development, has been described. Thus, feeding is a unique and complex process. For maturation, it requires processes of: a) the acceptance of a wide variety of food in terms of stage of development, their texture, and types; and b) safe and successful sucking, chewing, and swallowing (35). Defining stages in the normal development of feeding include: homeostasis, attachment-transition and separation-individualization (22,35,36). In these stages, depending on infantile development and the interaction with the adult, the infant engages in communicative acts that include visual contact, smiling, gests, gurgling, the establishment of eating routines, and taking turns (35).
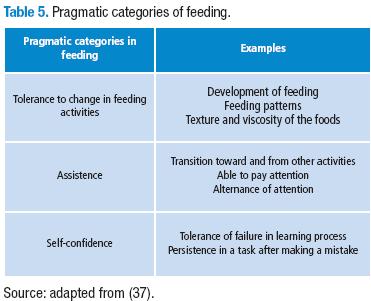
As such, here we describe a series of pragmatic categories involved in the process of ingestion and deglutition that are determined by the psychosocial interaction between the child and their caretaker (37). They are shown in Table 5.
Another pragmatic component involved in the feeding process is represented by feeding postures. These depend directly on the infant’s age, the stage of feeding development of their motor development, the type of utensils used, and the types of food provided for feeding (22).
The identification of this and other experiential information associated with the ingestion of food and swallowing are inherent to the process of the development of oromotor skills. Some of the sensations involved include the sensation of contact with the food or utensil, the pressure, the temperature, and the taste. Sensations that are distantly related with the process are the sense of smell, sight, and hearing. The relevant proprioceptive information is related to the positioning and movement of the joints and muscles, of the body in space, breathing, the sensations of hunger and thirst, and the digestive condition (38). This sensorial impulse is also seen in the development of the five phases of deglutition (39).
Kinesthesia plays an important role in the proprioceptive process since it is the sense of movement and position of the parts of the body like the tongue and the jaw (13). Some of the receptors responsible for providing kinesthetic information include: muscle and joint receptors, and mechanoreceptors in the skin and mucous membranes. Meanwhile, proprioception generates an awareness of spatial relationships, of the internal form and configuration of movement, and of the quantity and regulation of internal muscular effort.
The tongue has a leading role in the recognition of proprioception because of its ability to detect the sense of taste (13). This involves taste receptors, tastes and personal preferences, taste detection thresholds and adaptations to different tastes. All of these factors influence the development of the sense of taste. Motor processing together with sensorial processing makes up a work network that promotes phonological development by using feedback given to the child from the environment in which they are developing (18). In this process, the brain interprets received stimuli, and, later, a response is made. This response will be translated emotionally and will be determined as positive (pleasant) or negative (aversive). This mix of sensation and movement will give specificity in oromotor development, leading movements to become reduced and refined. Thanks to movement (muscular contraction), proprioception and muscle tone are generated, followed by stabilization and the dissociation of the movement of the joints.
This process, denominated oral exploration, is characterized as the earliest and most basic sensorimotor activity. It allows for the organization of oral patterns. This activity will promote the reduction of aversive experiences related to the food textures to which the children are exposed, given that it refers to a process of neuromuscular training with a physiological basis.
The muscular capacity needed for the specificity of normal movements is based on precision, dexterity, and the ability of the tongue to act with speed and without problems in making contact and movements during speech without tiring. This dexterity related to speech organs can be divided into three categories: strength (18), tone (14,18), and resistance (18).
Instruments involved in feeding processes
Baby’s bottle
Artificial feeding consists of taking food from a bottle and can be provided by a mother or a substitute (27,29). Artificial sucking demands that the lips completely attach to the nipple, permitting a total anterior seal, which favors the creation of negative intra-oral pressures. The back of the tongue canalizes to receive the nipple and the jaw ascends and descends freely, compressing the liquid. The sucking should be easily started, rhythmic, strong, sustained, and efficient, just like is done with the sucking pattern in the mother’s breast (30).
Spoon
Ingestion from a spoon is initially a passive process in which movements identical to those in sucking can be observed, including: half-open lips, protruding tongue, and a free up and down movement of the lower jaw (22). When the spoon approaches the infant’s body, it leans forward. The tongue also leans forward slightly when pieces of food fall from the spoon. From the combined work of experiences and visual stimuli, the mouth opens enough so that the spoon and the food can enter the oral cavity. While the jaw is stabilized in the open position, the tongue descends to the floor of the mouth until the spoon is inside the mouth (30). In this moment, there is a simultaneous movement of the lips and the jaw to take the food from the spoon and hold it in the mouth.
The jaw closes gradually and slowly, the upper lip moves forward and down to clean the spoon while the tongue begins to move to distribute the food in the oral cavity, mixing it with saliva so that the papillae can execute the action of their taste receptors and, later, prepare the food for swallowing or chewing.
Cup
The specific movement that takes place so that ingestion can happen using a cup as an instrument depends on the form that it has and how full it is. A narrow cup generally requires tipping the head backward when there is little liquid left in the bottom. However, if the cup has a large opening or is full of liquid, it is only necessary to move it toward the chin and tip it backward (29). This process requires complete and efficient cervical control, since cephalic hyperextension and possible bronco-aspiration should be avoided. The cup touches the lower lip without going beyond the teeth or gums to avoid the presence of the phasic bite, the tongue remains flat in the oral cavity (although occasionally vertical movements can be seen), the cheeks contract a bit to help create adequate intra-oral pressures, the jaw makes up and down movements similar to those in the sucking pattern (this helps to move the liquid to the back part of the oral cavity to facilitate swallowing), the lips close after ingestion to avoid the spilling of the liquid from the oral cavity, and the action of the muscles of the cheeks becomes important to avoid later spilling.
Generally, ingestion from a cup is introduced between the ages of four and six months, once the child has developed a mature suction pattern, and voluntary lip attachment occurs (29). Initially, the infant takes single sips in which sputtering and choking is frequent. As coordination between sucking and swallowing is developed, these difficulties will disappear and the sips will increase in speed and frequency. Also, less liquid will be spilled than before.
Straw
To drink with a straw, a good intra-oral pressure is important, since this is the only feeding activity that is done against gravity (29). It is for that reason that it is useful for effectively toning the orofacial musculature.
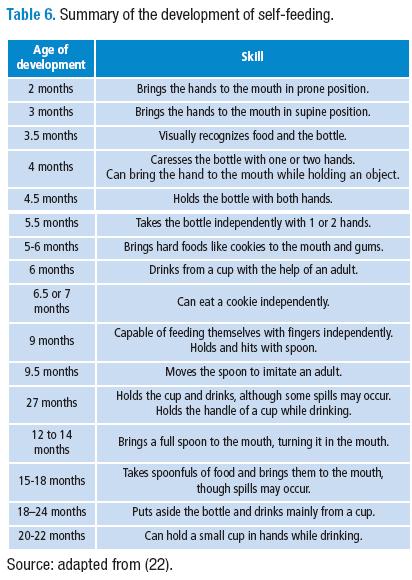
The process starts with the lips pressed against the straw and the jaw in descent. Later, the lips move forward to protrude. The tongue canalizes so as to allow for the introduction of the straw and begins forward and backward movements. The lower jaw moves freely up and down while the cheeks contract, increasing the pressure in the oral cavity. Drinking through the straw especially favors the development of the coordination of sucking/swallowing/respiration (S:S:R:), reducing sputtering due to the rhythmic movements of the lips, tongue, jaw, and cheeks. The initial use of the straw may vary; it is possible to find it from seven to eight months, when the tongue begins to make forward-backward movements with greater control, capable of a rhythmic movement for approximately 5 minutes (22). After the use of the different instruments described above, independent feeding skills are developed (22). These skills are presented below in Table 6.
Anatomy of the stomatognathic system.
The stomatognathic system is made up of a heterogeneous group of tissues and organs that include structures of bone, muscles, joints, and glands, as well as associated vascular, lymphatic, and nervous components (40). From the functional point of view, passive and active structures can be distinguished: the passive structures are represented by the upper and lower jaw (1), which are related by the temporomandibular joint (14), the hyoid bone, and other cranial bones like the temporal bones. Static structures refer to the collection of structures that cannot move of their own accord. The dynamic structures are the neuromuscular components that represent the true motors of the system. Finally, the annex structures include salivary glands, and associated vascular and lymphatic components. Below, some of these will be described.
Development of hard tissues
Normal facial growth includes a downward and forward movement, in which the mandible and the maxillae develop to become wider, longer, and taller (22). The width is the first process to be completed. It includes the growth of the dental arches and finalizes before adolescence. The growth of the nasopharynx, however, is completed at two years of age. Lengthening occurs until puberty, up until 14 or 15 years of age in females and until 18 years of age in males. In terms of height/verticality, the growth of this proportion of the branches of the jaws and the face in general continues in girls until 17 or 18 years of age and to 20 years of age in boys.
While facial development is genetically determined, there are other elements, like the action of surrounding soft tissue or an abnormal mandible descent, that can alter it (22). The anatomical relationships of the face begin to change around four to six months when the mandible descends and the intraoral space increases. At this moment, the tongue begins up and down movements. With neurological maturation, in these months the cortical control of different motor patterns begins. These physical and neurological changes are responsible for the change in the sucking pattern seen at this age.
Thus, in the development of the different stomatognathic functions, the action of the following cranial nerves is included. They are listed here together with their functions (22,35): the olfactory nerve (I), sense of smell; the trigeminal nerve (V), sensory fibers —the anterior two thirds of the tongue, the soft palate, the nasopharynx, the mouth, taste— and motor fibers —mastication muscles—; the facial nerve (VII), sensory fibers —taste, two anterior thirds of the tongue, feeling in the lips, submandibular and sublingual salivary glands—; glossopharyngeal nerve (IX), sensory fibers —mucous membrane of the pharynx, posterior third of the tongue, feeling in the tonsils, hard and soft palate— and motor fibers —superior pharyngeal muscles—; vagus nerve (X), sensory fibers —viscera, thorax, abdomen, pharynx, larynx, and esophagus—, motor fibers —middle pharyngeal muscles, muscles of the larynx, and the root of the tongue—, and autonomic fibers —the heart, soft muscles and glands or gastric motility, and respiratory pressure—; accessory nerve (XI), motor fibers —neck muscles and the sternocleidomastoid muscle—; hypoglossal nerve (XII), motor fibers —intrinsic and extrinsic muscles of the tongue—.
Method
For the compilation of literature surrounding the topic of the normal development of oral-motor patterns up to the age of six years, a bibliometric review of the scientific articles available in journals indexed in the databases of the Universidad Nacional de Colombia coming from Colombia, Latin America, North America, Europe, and Asia. Also, digital and physical books and other academic documents that discuss this topic were used.
Procedure
The present study, which originated as an undergraduate thesis, was executed in two parts. The first part consisted of the recompilation of the information on the development of each oral-motor pattern found in the articles and books consulted, including: respiration, swallowing, sucking, biting, mastication and speech, as well as the use of feeding utensils (spoon, cup, straw), ambient and postural factors affecting feeding, sensitivity, muscle tone and resistance, the description of the anatomical structures of the stomatognathic system (development of hard tissues, osteology, oral cavity, pharynx, and larynx), functional description of orofacial structures, and neurology of feeding.
In the second part, the manual of oral-motor skills was created. This work compiled the main characteristics of the development of each oral-motor pattern with respect to age, according to the information found in the first phase of the study. This manual will facilitate the consultation by phonoaudiology professionals of the normal development of these skills in their professional practice. The development can be consulted generally by months or by a certain pattern, depending on the immediate needs of the professional. Finally, the present article, that brings together the main findings of the study and the book (where they are presented in depth), was written.
Results
As a result, with regard to the articles, 12 undergraduate theses available in the databases of different Colombian universities were reviewed. They had the following distribution: two theses from the Universidad del Valle (3,4), one from the Corporación Universitaria Iberoamericana (5), three in the Universidad Manuela Beltrán (6-8), two from the Escuela Colombiana de Rehabilitación (11,12), two at the Universidad del Rosario (9,10), and two from the Universidad Nacional de Colombia (13,16). In this review, two postgraduate theses were also explored (14,15). Furthermore, 18 books were found (1,2,18,19,29,30,35,38,41- 57), as well as 31 articles from indexed journals (20-24,26,27,31–34,36,39,40,58-71), and one webpage (28). These accounted for the information on the development of oromotor patterns and on the items put forward above in the method section. After finalizing the first phase of the research (literature review), high evidence of studies referring to the stomatognathic system was found, in which it is possible to delimit the most significant processes involved in child development of the oral-motor patterns. These patterns include sucking patterns —sucking in the first four months—, the respiration pattern —characterized by expiration-swallowing-expiration, followed by inspiration-expiration-expiration, and, finally, expiration-swallowing-inspiration—, the immature and mature swallowing pattern, types of biting —phasic, unconscious, graded, stereotyped and non-stereotype vertical, with diagonal and circular rotation—.
In mastication, the action of a series of reflexes can be seen. Among these are the phasic jaw-opening reflex, the jaw-jerk reflex, the stretch reflex, the Golgi tendon reflex, and the inhibitory reflex of the levator muscles.
A anatomo-functional description was also provided of the bone and muscle structures, and of the structures of the stomatognathic system that participate in the execution of these and all oromotor patterns, including the temporomandibular joint and its relationship with the processes of biting and chewing.
Phases of motor-oral differentiation that describe the relationship of this process of motor dissociation with the production of the sounds of speech (18, 20).
Neurological activity during each of the oromotor patterns.
Neural control of respiration determined by the brain stem.
Neural control of swallowing, which involves the following cranial nerves: the trigeminal (V), facial (VII), glossopharyngeal (IX), vagus (X), accessory (XI) and hypoglossal (XII) nerves.
Neural control of sucking: involves the cranial nerves connected to the brain stem, which have sensory fibers.
Eruption of the teeth starting towards six months of age, ending around 30 months of age.
In this phase of the research, the book entitled Descripción del desarrollo de los patrones oromotores desde el nacimiento hasta los seis años de edad (Description of the development of oral-motor patterns from birth to 6 years of age) was consolidated. This book explores the sections touched upon in this article in greater depth. A manual for practical use with the same title was also produced.
Conclusions
Based on the collection of information available in the scientific literature regarding the development of oromotor patterns and feeding processes, it can be concluded that, in child development, these patterns reveal processes of change and maturation that are related to the neurological, socio-affective and motor development that each child has. Thus, initially they are reflexes, later turning into voluntary actions and, finally, are perfected within the processes of eating and speech. This, added to factors such as the introduction of new food textures; the use of instruments like the cup, spoon, and straw; the tooth eruption processes; and oral sensory experiences will foster an optimal oral-motor development of feeding functions around three years old and speech at the end of six years old.
Furthermore, we conclude that the knowledge of the characterization by phonoaudiologists interested in the topic of the structural behavior and functionality of the stomatognathic system with regard to child developmental age and normal development is essential. From this knowledge, different clinical trials are proposed (72) since understanding the processes of eating, sucking, and swallowing is their responsibility. Therefore, it is important to continue doing research that allows us to create new, valid, and reliable strategies for their inclusion in professional activities.
Finally, to ensure the resolution of concerns, to complement the information provided in the article, to deepen the understanding the concepts discussed here, and to make good use of them, it is necessary to read the manual entitled Descripción del desarrollo de los patrones oromotores desde el nacimiento hasta los seis años de edad (Description of the development of oral-motor patterns from birth to 6 years of age).
Conflict of interest
None declared by the authors.
Financing
None declared by the authors.
Acknowledgements
None declared by the authors.
References
1. Echeverri E, Sencherman G. Neurología de la oclusión. Bogotá: Editorial Monserrate LTDA; 1984.
2. Queiroz I. Fundamentos de Fonoaudiología: aspectos clínicos de la motricidad oral. Panamericana. 2002.
3. Bonilla C, Paredes D, Loaiza M. Influencia de las alteraciones en el tono muscular en niños con insuficiencia motriz de origen cerebral en el proceso del habla. [Undergraduate thesis]. Bogotá: Universidad del Valle; 1997.
4. Giraldo V, Paula M, Patiño C. Prevención y detección de desórdenes miofuncionales orales en niños y niñas entre 5 y 10 años de la escuela Rufino José Cuervo. [Undergraduate thesis]. Bogotá: Universidad del Valle; 2001.
5. Inocencio M, Prada P, Rojas S. Estudio exploratorio de las actividades pre fónicas de succión, deglución, mordida y mascado en niños con parálisis cerebral espástica de 12-247 meses de edad. [Undergraduate thesis]. Bogotá: Universidad Iberoamericana; 1997.
6. Cendirini R, Granada J. Caracterización de los trastornos deglutorios en pacientes pediátricos pos intubación orotraqueal. [Undergraduate thesis]. Bogotá: Universidad Manuela Beltrán; 2012.
7. Figueroa S, Hernández N, Sánchez S. Protocolo de evaluación de la deglución pediátrica en niños entre 3 y 6 años. [Undergraduate thesis]. Bogotá: Universidad Manuela Beltrán; 2008.
8. Godoy L, Zamora E. Cartilla sobre abordaje miofuncional en niños de edad escolar de 3 años a 7 años. [Undergraduate thesis]. Bogotá: Universidad Manuela Beltrán; 2011.
9. Chaparro N, Marín A. Influencia de los hábitos orofaciales en las funciones del aparato estomatognático. [Undergraduate thesis]. Bogotá: Universidad del Rosario; 2003.
10. Guerrero D, Pérez A, Sáenz M. Descripción de los procesos deglutorios en niños con lph de 0 a 6 meses que utilizan placa obturadora. [Undergraduate thesis]. Bogotá: Universidad del Rosario; 2002.
11. Cardozo M, González M, Madero O. Habilidades de los órganos fonoarticuladores y su correlación con el proceso alimentario en niños de 12-24 meses. [Undergraduate thesis]. Bogotá: Escuela Colombiana de rehabilitación; 1994.
12. González M, Otero D, Severino P. Habilidades de los órganos fonoarticuladores y su correlación con el proceso alimentario. [Undergraduate thesis]. Bogotá: Escuela Colombiana de rehabilitación; 1993.
13. Castañeda B, Porras C. Aplicación de un programa para el desarrollo de las habilidades motrices orales en niños con enfermedad motriz cerebral. [Undergraduate thesis]. Bogotá: Universidad Nacional de Colombia; 1999.
14. Rivera H. Desarrollo motor y desarrollo del habla: ampliando las perspectivas. [Undergraduate thesis]. Bogotá: Universidad Nacional de Colombia; 2006.
15. La Torre C. Relación entre las funciones orales y articulación temporomandibular. [Postgraduate thesis]. Bogotá: Universidad Nacional de Colombia; 2006.
16. Cuervo D, Rodríguez J. Estado del sistema estomatognático en reposo y su influencia en los procesos alimenticio y de habla. [Undergraduate thesis]. Bogotá: Universidad Nacional de Colombia; 2002.
17. Camargo C, Pinzon G. La promoción de la salud en la primera infancia: evolución del concepto y su aplicación en el contexto internacional y nacional. Rev. Fac. Med. 2012;60: S62-74.
18. Boshart C. Oral-Motor analysis and remediation techniques. Temecula, USA: Speech Dynamics Incorporated; 1998.
19. Boshart C. Treatise in the tongue analysis and treatment of tongue abnormalities. Temecula, USA: Speech dynamics incorporated; 1999.
20. Connolly K, Dalgleish M. The emergence of a tool-using in infancy. Dev Psychol. 1989;25:894-912. http://doi.org/fhwkhj.
21. Department of agriculture policy. A guide for use in the child nutrition programs. Washington: Department of agriculture; 2001.
22. Morris S, Dunn M. Pre feeding skills. 2a edición. San Antonio, Estados Unidos: Therapy Skill Builders; 2000.
23. Fieramosca F, Lezama E, Manrique R, Quiros O, Farias M, Rondón S, et al. La función respiratoria y su repercusión a nivel del sistema estomatognático. Ortodoncia Ws [Internet]. 2007:1-13 [cited 2014 April 26]. Available from: http://goo.gl/XiUaVm.
24. Feldman J, Mitchell G, Nattie E. Breathing: Rhythmicity, Plasticity, Chemosensitivity. Annu Rev Neurosci. 2003;26:239-66. http://doi.org/bsws8h.
25. Álvarez W, Jara B, Lagos M, Silva S, Veloso A. Patrones de deglución en un grupo de niños chilenos de 2, 3 y 4 años. [Undergraduate thesis]. Santiago, Chile: Universidad De Chile, Facultad de Medicina, Escuela de Fonoaudiología; 2007.
26. Ertekin C, Aydogdu I. Neurophysiology of swallowing. Clin Neurophysiol. 2003;114:2226-44. http://doi.org/fgc6kz.
27. Hurst N, Lau C. Oral feeding in infants. Curr Probl Pediatr. 1999:105-24.
28. Beckman oral motor Search for Knowledge[Internet]. Maitland, Florida. Oral Motor Patterns. [cited 2014 April 9]. Available from: http://goo.gl/EN3er9.
29. Reyes R, Rivera H. Evaluación fonoaudiológica de estructuras y funciones del sistema estomatognático. Place unknown: publisher unknown;2000.
30. Morris S, Dunn M. Pre feeding skill. Place unknown: Therapy Skill Builders; 1987.
31. Eishima M, Iwayama K. Neonatal sucking behaviour and its development until 14 months. Early Hum Dev. 1996;47:1-9.
32. Green J, Moore C, Reilly K. The Sequential Development of Jaw and Lip Control for Speech. J Speech Lang Hear Res. 2002;45:66-79. http://doi.org/db2jrc.
33. Camargo M. Desarrollo fonético-fonológico del español en niños. Umbral científico. 2006;9:5-9.
34. Reyes M, Rivera H. Desarrollo normal de las funciones alimenticias. Revista Odontos. 2002;16:12-7.
35. Arvedson J, Brodsky L. Pediatric swallowing and feeding. 2nd Edition. Canada: Thompson Learning; 2002.
36. Arvedson J, Roger B. Assessment of infant oral sensorimotor and swallowing function. Ment Phys Disabil Law Rep. 2005;11:74-82.
37. Sheppard J. Using motor learning approaches for treating swallowing and feeding disorders: A review. Lang Speech Hear Serv Sch. 2008;39:227-36. http://doi.org/dpz58f.
38. Sheppard J. Eating-related behaviors and swallowing and feeding skills in children. En: Handbook of behaivor food and nutritioncap motor learning approaches for iproving negative. New York: Springer; 2011. pp. 3271-84.
39. Miller A, Steele C. Sensory input pathways and mechanisms in swallowing: A review. Dysphagia. 2010;25:323-33. http://doi.org/fbmbvd.
40. Beszkin M, Losviz E, Zielinsky L. El sistema estomatognático: un sistema complejo. RAAO. 2005;XLIV:27-32.
41. Catalán J. Examen físico del recién nacido. En: Nazer J, Ramírez R. Neonatología. Santiago de Chile, Chile: Editorial Universitaria; 2003. pp. 23-33.
42. Department of agriculture policy. Infant nutrición and feeding: A guide for Use in the WIC and CSF programs. Washington: Department of agriculture policy; 2009.
43. Fondo de las Naciones Unidas para la Infancia. UNICEF. Por una niñez bien nutrida. Área de políticas básicas. Colombia: UNICEF; 2004.
44. François R. Tratado de osteopatía craneal. Madrid: Editorial Panamericana; 2005.
45. Garliner D. Myofunctional theraphy in dental practice. Abnormal swallowing habits: diagnosis-treatment. Coral Gables, Florida: Bartel Dental Book Co; 1974.
46. Gilroy A, Mac Pherson B, Ross L. Atlas de anatomía Prometheus. Madrid: Editorial Médica Panamericana; 2009.
47. González T, Zambrana N. Logopedia y ortopedia maxilar en la rehabilitación orofacial tratamiento precoz y preventivo terapia miofuncional. Barcelona: Masson; 1998.
48. Hamdy S, Mistry S. Neural control of feeding and swallowing. Phys Med Rehabil Clin N Am. 2008;19:709-28. http://doi.org/b8x267.
49. Manns A, Díaz G. Sistema estomatognático. Santiago: Universidad de Chile, Facultad de Odontología; 1988.
50. McCarthy J. Feedding infants & toddlers, strategies for safe, stress-free meal times [Internet]. 2006 [cited 2014 May 8]. Available from: http://goo.gl/1VA9NM.
51. Ministerio de la protección social. Guías alimentarias paras niños y niñas colombianos. Menores de 2 años. Bases técnicas. Bogotá: Ministerio de la protección social; 2004.
52. Ministerio de salud, Instituto Colombiano de Bienestar Familiar. Guías alimentarias para la población colombiana mayor de dos años. Bases técnicas. Bogotá: Ministerio de Salud; 1999.
53. Posel P, Schulte E. Mini Sobotta: Esquemas de Anatomía, histología y embriología. España: Marban; 2005.
54. Ricard F. Tratado de osteopatía craneal. Articulación temporomandibular. Analisis y tratamiento ortodóntico. 2nd Edition. Madrid: Editorial Médica Panamericana; 2013.
55. Toledo N, Dalva L. Logopedia y ortopedia maxilar en la rehabilitación orofacial. Barcelona: Masson; 2002.
56. Velayos J, Díaz H. Anatomía de la cabeza con enfoque odontoestomatológico. Madrid: Editorial Médica Panamericana; 1998.
57. Watson C. Supporting sucking skills in breastfeeding infants. New York: Woodhaven, New York Jones & Bartlett learning; 2013.
58. Aguilar F. Alimentación y deglución. Aspectos relacionados con el desarrollo normal. Plasticidad y restauración nuerológica. 2005;4:49-57.
59. Alcazas V, Martínez R. La fonología de las primeras palabras del español de la ciudad de México: una relectura a lo propuesto por Roman Jackobson. Función. 1998;18:21-34.
60. Arvedson J, Delaney A. Development of swallowing and feeding: prenatal through first year of life. Dev Disabil Res Rev. 2008;14:105-17. http://doi.org/ftt46m.
61. Baterson V, Gribble P, Ostry D. An examination of the degrees of freedom of human jaw motion in speech and mastication. J Speech Lang Hear Res. 1997;40:134-5.
62. Beckman D, Neal C, Phrirsichbaum J, Stratton L, Taylor V, Ratusnik D. Range of movement and strenght in oral motor therapy: A retrospective study. J Commun Disord. 2004;21:7-14.
63. Bronwen K, Huckabee M, Jones R, Frampton C. The first year of human life: Coordinating respiration and nutritive swallowing. Dysphagia. 2007;22:37-43. http://doi.org/bnkfcr.
64. Coloma C, Maggiolo M, Pavez M, Peñaloza C. Desarrollo fonológico en niños de 3 a 6 años: incidencia de la edad, el género y el nivel socioeconómico. Revista Signos. 2010;43:31-48. http://doi.org/cvfm5x.
65. Davenport P, Zhang W. Neural control of breathing. Perspectives on voice and voice disorders. 2005;15:20-4. http://doi.org/c6mtff.
66. Gewolb I, Vice F. Maturational changes in the rhythms, patterning, and coordination of respiration and swallow during feeding in preterm and term infants. Dev Med Child Neurol. 2006;48:589-94. http://doi.org/cbnzpc.
67. León H, Vivar P. Desarrollo fonológico-fonético en un grupo de niños entre 3 y 5, 11 años. CEFAC. 2009;11:190-8. http://doi.org/bdbwxv.
68. Lowell S, Poletto C, Knorr-Chung B, Reynolds R, Simonyan K, Ludlow C. Sensory stimulation activates both motor and sensory components of the swallowing system. Neuroimage. 2008;42:285-95. http://doi.org/fc5gwf.
69. Mandelbau E, Montagneri L. Caracterização da função mastigatória em crianças com dentição decídua e dentição mista Cefac Brasil. CEFAC. 2009;11:324-33.
70. Morquette P, Lavoie R, Fhima M, Lamoureux X, Verdier D, Arlette K. Generation of the masticatory central pattern and its modulation by sensory feedback. Prog Neurobiol. 2012;96:340-55. http://doi.org/zf7.
71. Steel C, Miller A. Sensory input pathways and mechanisms in swallowing: A review. Dysphagia. 2010;25:323-33. http://doi.org/fbmbvd.
72. American Speech-Language-Hearing association. Preferred practice patterns for the profession of Speech-Language Pathology [Internet]. 2004 [cited 2014 May 8]. Available from: http://goo.gl/yzZQ2K.
Referencias
Echeverri E, Sencherman G. Neurología de la oclusión. Bogotá: Editorial Monserrate LTDA; 1984.
Queiroz I. Fundamentos de Fonoaudiología: aspectos clínicos de la motricidad oral. Panamericana. 2002.
Bonilla C, Paredes D, Loaiza M. Influencia de las alteraciones en el tono muscular en niños con insuficiencia motriz de origen cerebral en el proceso del habla. [Undergraduate thesis]. Bogotá: Universidad del Valle; 1997.
Giraldo V, Paula M, Patiño C. Prevención y detección de desórdenes miofuncionales orales en niños y niñas entre 5 y 10 años de la escuela Rufino José Cuervo. [Undergraduate thesis]. Bogotá: Universidad del Valle; 2001.
Inocencio M, Prada P, Rojas S. Estudio exploratorio de las actividades pre fónicas de succión, deglución, mordida y mascado en niños con parálisis cerebral espástica de 12-247 meses de edad. [Undergraduate thesis]. Bogotá: Universidad Iberoamericana; 1997.
Cendirini R, Granada J. Caracterización de los trastornos deglutorios en pacientes pediátricos pos intubación orotraqueal. [Undergraduate thesis]. Bogotá: Universidad Manuela Beltrán; 2012.
Figueroa S, Hernández N, Sánchez S. Protocolo de evaluación de la deglución pediátrica en niños entre 3 y 6 años. [Undergraduate thesis]. Bogotá: Universidad Manuela Beltrán; 2008.
Godoy L, Zamora E. Cartilla sobre abordaje miofuncional en niños de edad escolar de 3 años a 7 años. [Undergraduate thesis]. Bogotá: Universidad Manuela Beltrán; 2011.
Chaparro N, Marín A. Influencia de los hábitos orofaciales en las funciones del aparato estomatognático. [Undergraduate thesis]. Bogotá: Universidad del Rosario; 2003.
Guerrero D, Pérez A, Sáenz M. Descripción de los procesos deglutorios en niños con lph de 0 a 6 meses que utilizan placa obturadora. [Undergraduate thesis]. Bogotá: Universidad del Rosario; 2002.
Cardozo M, González M, Madero O. Habilidades de los órganos fonoarticuladores y su correlación con el proceso alimentario en niños de 12-24 meses. [Undergraduate thesis]. Bogotá: Escuela Colombiana de rehabilitación; 1994.
González M, Otero D, Severino P. Habilidades de los órganos fonoarticuladores y su correlación con el proceso alimentario. [Undergraduate thesis]. Bogotá: Escuela Colombiana de rehabilitación; 1993.
Castañeda B, Porras C. Aplicación de un programa para el desarrollo de las habilidades motrices orales en niños con enfermedad motriz cerebral. [Undergraduate thesis]. Bogotá: Universidad Nacional de Colombia; 1999.
Rivera H. Desarrollo motor y desarrollo del habla: ampliando las perspectivas. [Undergraduate thesis]. Bogotá: Universidad Nacional de Colombia; 2006.
La Torre C. Relación entre las funciones orales y articulación temporomandibular. [Postgraduate thesis]. Bogotá: Universidad Nacional de Colombia; 2006.
Cuervo D, Rodríguez J. Estado del sistema estomatognático en reposo y su influencia en los procesos alimenticio y de habla. [Undergraduate thesis]. Bogotá: Universidad Nacional de Colombia; 2002.
Camargo C, Pinzon G. La promoción de la salud en la primera infancia: evolución del concepto y su aplicación en el contexto internacional y nacional. Rev. Fac. Med. 2012;60: S62-74.
Boshart C. Oral-Motor analysis and remediation techniques. Temecula, USA: Speech Dynamics Incorporated; 1998.
Boshart C. Treatise in the tongue analysis and treatment of tongue abnormalities. Temecula, USA: Speech dynamics incorporated; 1999.
Connolly K, Dalgleish M. The emergence of a tool-using in infancy. Dev Psychol. 1989;25:894-912. http://doi.org/fhwkhj.
Department of agriculture policy. A guide for use in the child nutrition programs. Washington: Department of agriculture; 2001.
Morris S, Dunn M. Pre feeding skills. 2a edición. San Antonio, Estados Unidos: Therapy Skill Builders; 2000.
Fieramosca F, Lezama E, Manrique R, Quiros O, Farias M, Rondón S, et al. La función respiratoria y su repercusión a nivel del sistema estomatognático. Ortodoncia Ws [Internet]. 2007:1-13 [cited 2014 April 26]. Available from: http://goo.gl/XiUaVm.
Feldman J, Mitchell G, Nattie E. Breathing: Rhythmicity, Plasticity, Chemosensitivity. Annu Rev Neurosci. 2003;26:239-66. http://doi.org/bsws8h.
Álvarez W, Jara B, Lagos M, Silva S, Veloso A. Patrones de deglución en un grupo de niños chilenos de 2, 3 y 4 años. [Undergraduate thesis]. Santiago, Chile: Universidad De Chile, Facultad de Medicina, Escuela de Fonoaudiología; 2007.
Ertekin C, Aydogdu I. Neurophysiology of swallowing. Clin Neurophysiol. 2003;114:2226-44. http://doi.org/fgc6kz.
Hurst N, Lau C. Oral feeding in infants. Curr Probl Pediatr. 1999:105-24.
Beckman oral motor Search for Knowledge[Internet]. Maitland, Florida. Oral Motor Patterns. [cited 2014 April 9]. Available from: http://goo.gl/EN3er9.
Reyes R, Rivera H. Evaluación fonoaudiológica de estructuras y funciones del sistema estomatognático. Place unknown: publisher unknown;2000.
Morris S, Dunn M. Pre feeding skill. Place unknown: Therapy Skill Builders; 1987.
Eishima M, Iwayama K. Neonatal sucking behaviour and its development until 14 months. Early Hum Dev. 1996;47:1-9.
Green J, Moore C, Reilly K. The Sequential Development of Jaw and Lip Control for Speech. J Speech Lang Hear Res. 2002;45:66-79. http://doi.org/db2jrc.
Camargo M. Desarrollo fonético-fonológico del español en niños. Umbral científico. 2006;9:5-9.
Reyes M, Rivera H. Desarrollo normal de las funciones alimenticias. Revista Odontos. 2002;16:12-7.
Arvedson J, Brodsky L. Pediatric swallowing and feeding. 2nd Edition. Canada: Thompson Learning; 2002.
Arvedson J, Roger B. Assessment of infant oral sensorimotor and swallowing function. Ment Phys Disabil Law Rep. 2005;11:74-82.
Sheppard J. Using motor learning approaches for treating swallowing and feeding disorders: A review. Lang Speech Hear Serv Sch. 2008;39:227-36. http://doi.org/dpz58f.
Sheppard J. Eating-related behaviors and swallowing and feeding skills in children. En: Handbook of behaivor food and nutritioncap motor learning approaches for iproving negative. New York: Springer; 2011. pp. 3271-84.
Miller A, Steele C. Sensory input pathways and mechanisms in swallowing: A review. Dysphagia. 2010;25:323-33. http://doi.org/fbmbvd.
Beszkin M, Losviz E, Zielinsky L. El sistema estomatognático: un sistema complejo. RAAO. 2005;XLIV:27-32.
Catalán J. Examen físico del recién nacido. En: Nazer J, Ramírez R. Neonatología. Santiago de Chile, Chile: Editorial Universitaria; 2003. pp. 23-33.
Department of agriculture policy. Infant nutrición and feeding: A guide for Use in the WIC and CSF programs. Washington: Department of agriculture policy; 2009.
Fondo de las Naciones Unidas para la Infancia. UNICEF. Por una niñez bien nutrida. Área de políticas básicas. Colombia: UNICEF; 2004.
François R. Tratado de osteopatía craneal. Madrid: Editorial Panamericana; 2005.
Garliner D. Myofunctional theraphy in dental practice. Abnormal swallowing habits: diagnosis-treatment. Coral Gables, Florida: Bartel Dental Book Co; 1974.
Gilroy A, Mac Pherson B, Ross L. Atlas de anatomía Prometheus. Madrid: Editorial Médica Panamericana; 2009.
González T, Zambrana N. Logopedia y ortopedia maxilar en la rehabilitación orofacial tratamiento precoz y preventivo terapia miofuncional. Barcelona: Masson; 1998.
Hamdy S, Mistry S. Neural control of feeding and swallowing. Phys Med Rehabil Clin N Am. 2008;19:709-28. http://doi.org/b8x267.
Manns A, Díaz G. Sistema estomatognático. Santiago: Universidad de Chile, Facultad de Odontología; 1988.
McCarthy J. Feedding infants & toddlers, strategies for safe, stress-free meal times [Internet]. 2006 [cited 2014 May 8]. Available from: http://goo.gl/1VA9NM.
Ministerio de la protección social. Guías alimentarias paras niños y niñas colombianos. Menores de 2 años. Bases técnicas. Bogotá: Ministerio de la protección social; 2004.
Ministerio de salud, Instituto Colombiano de Bienestar Familiar. Guías alimentarias para la población colombiana mayor de dos años. Bases técnicas. Bogotá: Ministerio de Salud; 1999.
Posel P, Schulte E. Mini Sobotta: Esquemas de Anatomía, histología y embriología. España: Marban; 2005.
Ricard F. Tratado de osteopatía craneal. Articulación temporomandibular. Analisis y tratamiento ortodóntico. 2nd Edition. Madrid: Editorial Médica Panamericana; 2013.
Toledo N, Dalva L. Logopedia y ortopedia maxilar en la rehabilitación orofacial. Barcelona: Masson; 2002.
Velayos J, Díaz H. Anatomía de la cabeza con enfoque odontoestomatológico. Madrid: Editorial Médica Panamericana; 1998.
Watson C. Supporting sucking skills in breastfeeding infants. New York: Woodhaven, New York Jones & Bartlett learning; 2013.
Aguilar F. Alimentación y deglución. Aspectos relacionados con el desarrollo normal. Plasticidad y restauración nuerológica. 2005;4:49-57.
Alcazas V, Martínez R. La fonología de las primeras palabras del español de la ciudad de México: una relectura a lo propuesto por Roman Jackobson. Función. 1998;18:21-34.
Arvedson J, Delaney A. Development of swallowing and feeding: prenatal through first year of life. Dev Disabil Res Rev. 2008;14:105-17. http://doi.org/ftt46m.
Baterson V, Gribble P, Ostry D. An examination of the degrees of freedom of human jaw motion in speech and mastication. J Speech Lang Hear Res. 1997;40:134-5.
Beckman D, Neal C, Phrirsichbaum J, Stratton L, Taylor V, Ratusnik D. Range of movement and strenght in oral motor therapy: A retrospective study. J Commun Disord. 2004;21:7-14.
Bronwen K, Huckabee M, Jones R, Frampton C. The first year of human life: Coordinating respiration and nutritive swallowing. Dysphagia. 2007;22:37-43. http://doi.org/bnkfcr.
Coloma C, Maggiolo M, Pavez M, Peñaloza C. Desarrollo fonológico en niños de 3 a 6 años: incidencia de la edad, el género y el nivel socioeconómico. Revista Signos. 2010;43:31-48. http://doi.org/cvfm5x.
Davenport P, Zhang W. Neural control of breathing. Perspectives on voice and voice disorders. 2005;15:20-4. http://doi.org/c6mtff.
Gewolb I, Vice F. Maturational changes in the rhythms, patterning, and coordination of respiration and swallow during feeding in preterm and term infants. Dev Med Child Neurol. 2006;48:589-94. http://doi.org/cbnzpc.
León H, Vivar P. Desarrollo fonológico-fonético en un grupo de niños entre 3 y 5, 11 años. CEFAC. 2009;11:190-8. http://doi.org/bdbwxv.
Lowell S, Poletto C, Knorr-Chung B, Reynolds R, Simonyan K, Ludlow C. Sensory stimulation activates both motor and sensory components of the swallowing system. Neuroimage. 2008;42:285-95. http://doi.org/fc5gwf.
Mandelbau E, Montagneri L. Caracterização da função mastigatória em crianças com dentição decídua e dentição mista Cefac Brasil. CEFAC. 2009;11:324-33.
Morquette P, Lavoie R, Fhima M, Lamoureux X, Verdier D, Arlette K. Generation of the masticatory central pattern and its modulation by sensory feedback. Prog Neurobiol. 2012;96:340-55. http://doi.org/zf7.
Steel C, Miller A. Sensory input pathways and mechanisms in swallowing: A review. Dysphagia. 2010;25:323-33. http://doi.org/fbmbvd.
American Speech-Language-Hearing association. Preferred practice patterns for the profession of Speech-Language Pathology [Internet]. 2004 [cited 2014 May 8]. Available from: http://goo.gl/yzZQ2K.
Cómo citar
APA
ACM
ACS
ABNT
Chicago
Harvard
IEEE
MLA
Turabian
Vancouver
Descargar cita
CrossRef Cited-by
1. Sacide Yildizeli Topcu, Melahat Akgun Kostak, Remziye Semerci, Ozlem Guray. (2020). Effect of Gum Chewing on Pain and Anxiety in Turkish Children During Intravenous Cannulation: A Randomized Controlled Study. Journal of Pediatric Nursing, 52, p.e26. https://doi.org/10.1016/j.pedn.2019.12.007.
2. S Nivetha, Arya Geetha, Navitha Ulaghanathan. (2023). Development and Validation of Oro-Motor Sensory Training Module for Feeding Problems in Children with Autism Spectrum Disorder. Journal of Indian Association for Child and Adolescent Mental Health, 19(2), p.178. https://doi.org/10.1177/09731342231191949.
3. Alaina Martens, Jessica Davidson, Katharine Radville, Natalie Peterman, Hayden Kamiya, Kristen Allison, Emily Zimmerman. (2026). Developmental progression of bottle-feeding in the first year of life. Early Human Development, 216, p.106507. https://doi.org/10.1016/j.earlhumdev.2026.106507.
4. James Makame, Henriette De Kock, M. Naushad Emmambux. (2023). Nutrient density and oral processing properties of common commercial complementary porridge samples used in southern Africa: Effect on energy and protein intakes among children aged 6–24 months. Journal of Texture Studies, 54(4), p.481. https://doi.org/10.1111/jtxs.12753.
5. Sheen A John, Reshmi Janardhanan, Anandaraj Soman, Ashok Sukumaran. (2021). Evaluation of the Association of Oral Stereognosis with Malocclusion in Children. International Journal of Clinical Pediatric Dentistry, 14(S1), p.S18. https://doi.org/10.5005/jp-journals-10005-2050.
6. Justyna Pilip-Malec, Magdalena Knapek. (2025). Wiedza i doświadczenia własne rodziców związane z rozszerzaniem diety dzieci. Logopaedica Lodziensia, (11), p.155. https://doi.org/10.18778/2544-7238.11.10.
7. Kai Jia Tey, Sarah Walker, Amanda Seidl, Camila Scaff, Loann Peurey, Bridgette L. Kelleher, William Havard, Lisa Hamrick, Pauline Grosjean, Margaret Cychosz, Heidi Colleran, Marisa Casillas, Elika Bergelson, Kasia Hitczenko, Alejandrina Cristia. (2026). The Development of Canonical Proportion as a Function of Community, Multilingualism, and Target Language’s Syllable Complexity. Journal of Child Language, , p.1. https://doi.org/10.1017/S0305000926100476.
8. Karen Eliana Ramírez-Gómez, Rosa Mercedes Sampallo-Pedroza. (2017). Fonoaudiología y lactancia humana. Revista de la Facultad de Medicina, 65(2), p.297. https://doi.org/10.15446/revfacmed.v65n2.56269.
9. Daiana Debucean, Judit Mihaiu, Adrian Marius Maghiar, Florin Marcu, Olivia Andreea Marcu. (2023). A Multidisciplinary Approach to Swallowing Rehabilitation in Patients with Forward Head Posture. Medicina, 59(9), p.1580. https://doi.org/10.3390/medicina59091580.
10. Tom Van Boxel-Woolf, Kathleen M. McCarthy. (2026). Speech and language skills in a case of Watson syndrome. Clinical Linguistics & Phonetics, 40(1), p.1. https://doi.org/10.1080/02699206.2025.2472051.
11. Kelly Guedes de Oliveira Scudine, Paula Midori Castelo, João Paulo Maires Hoppe, André Krumel Portella, Patricia Pelufo Silveira. (2024). Early Influences on Development of Sensory Perception and Eating Habits. Advances in Nutrition, 15(12), p.100325. https://doi.org/10.1016/j.advnut.2024.100325.
12. Selen Serel Arslan, Cansu Özşin Özler, Numan Demir, Şeyma Öztürk, Meryem Uzamış Tekçiçek, Aynur Ayşe Karaduman. (2021). Pediatric dentists can determine chewing performance level in children. Clinical Oral Investigations, 25(8), p.5043. https://doi.org/10.1007/s00784-021-03815-w.
13. Swapna Narayanan, Kavya Vijayan, Mekhala Vastare Guruprasad, Prashanth Prabhu P, Animesh Barman. (2022). Oral and Verbal Praxis in Impaired Language Learners. Perceptual and Motor Skills, 129(1), p.33. https://doi.org/10.1177/00315125211056421.
14. Nicole Hübl, Saakje P. da Costa, Nicole Kaufmann, Jun Oh, Klaus Willmes. (2020). Sucking patterns are not predictive of further feeding development in healthy preterm infants. Infant Behavior and Development, 58, p.101412. https://doi.org/10.1016/j.infbeh.2019.101412.
15. Denise Fernandes Barbosa, Laura Fernandes Bana, Maria Cristina Buta Michel, Miguel Meira e Cruz, Edilson Zancanella, Almiro José Machado Júnior. (2023). Rapid maxillary expansion in pediatric patients with obstructive sleep apnea: an umbrella review. Brazilian Journal of Otorhinolaryngology, 89(3), p.494. https://doi.org/10.1016/j.bjorl.2023.02.004.
16. Ghasem Mahmoodabadi, Ahmad Bavali‐Gazik, Fateme Mouhebati, Morteza Arab‐Zozani, Meysamreza Boghrati. (2024). The effectiveness of oral motor interventions on the weight gain, independent oral feeding, and length of hospital stay in hospitalized preterm infants: A systematic review and meta‐analysis. Health Science Reports, 7(9) https://doi.org/10.1002/hsr2.70015.
17. Fabio Savastano. (2023). Neuromuscular Orthodontics. , p.41. https://doi.org/10.1007/978-3-031-41295-0_4.
18. Dolapo A. Oladiran, Naushad M. Emmambux. (2022). Locally Available African Complementary Foods: Nutritional Limitations and Processing Technologies to Improve Nutritional Quality—A Review. Food Reviews International, 38(5), p.1033. https://doi.org/10.1080/87559129.2020.1762640.
19. Bilge Meral Koc, Tugce Ozlu Karahan, Ezgi Arslan Yuksel, Gokcen Garipoglu. (2025). Complementary feeding practices and nutritional status in infants living in Turkey: Iowa infant feeding attitude scale and complementary feeding index. Maternal & Child Nutrition, 21(1) https://doi.org/10.1111/mcn.13746.
20. Eunike Sianturi, Risti Saptarini Primarti, Arlette Suzy Setiawan. (2023). A self-reported cross-sectional study on the oral function and the quality of life in children with stunted growth. Frontiers in Pediatrics, 10 https://doi.org/10.3389/fped.2022.1019143.
21. Daniel Steven Cruz Romero, Rosa Mercedes Sampallo Pedroza, Paula Astrid Maldonado Barbosa. (2024). Prevalencia de lactancia materna exclusiva en los primeros 2 meses de edad posnatal en población pretérmino. Areté, 24(2), p.51. https://doi.org/10.33881/1657-2513.art24206.
Dimensions
PlumX
Visitas a la página del resumen del artículo
Descargas
Licencia
Derechos de autor 2015 Revista de la Facultad de Medicina

Esta obra está bajo una licencia Creative Commons Reconocimiento 3.0 Unported.
-