Results of total colonoscopy in the diagnosis of polyps. Case studies in Villavicencio, Colombia
Resultados de colonoscopia total en el diagnóstico de pólipos. Análisis de casos presentados en Villavicencio, Colombia
DOI:
https://doi.org/10.15446/revfacmed.v65n3.49484Palabras clave:
Colonoscopy, Proctosigmoidoscopy, Colonic polyps, Cancer Screening. (en)Colonoscopia, Proctosigmoidoscopia, Pólipos del colon. (es)
Descargas
Introduction: Any elevation above the normal plane of the colonic mucosa is considered a polypoid projection. As age increases, polyps are more likely to be found; in addition, polyps larger than 1 cm of diameter may potentially lead to a malignant neoplasm.
Objective: To establish the frequency, size, location and age groups of colonic polyp lesions in patients who underwent colonoscopy at Hospital Departamental in Villavicencio during 2009-2014.
Materials and methods: The results of 411 diagnostic colonoscopies were analyzed. Data collection and statistical description was done using SPPSS 2011 software.
Results: 43 (11%) polyps were smaller than 1cm; 16 (4%) were between 1cm and 2cm long; no polyps larger than 2cm were found, and the remaining results did not show any abnormality. Polyps were found in all segments of the colon in the 41-50 age group, but the highest percentage (11%) was observed in the 71-80 age group. 68.7% of polyps larger than 1cm and 67% smaller than 1cm were found in the left colon.
Conclusion: In population groups under 40 years of age, the incidence of polyps is low in the left colon and very low in the right colon.
Introducción. Cualquier levantamiento por encima del plano normal de la mucosa colónica es considerada proyección polipoidea. A mayor edad es más probable encontrar pólipos; además, los >1 cm de diámetro tienen mayor potencial de desarrollar neoplasia maligna.
Objetivo. Establecer la frecuencia de lesiones polipósicas del colon, su tamaño, su localización y los grupos de edades donde están presentes en pacientes a quienes se les realizó colonoscopia en el Hospital Departamental de Villavicencio en el periodo 2009-2014.
Materiales y métodos. Se analizaron los resultados de 411 colonoscopias diagnósticas. La recolección de datos y descripción estadística se hizo con el software SPPSS 2011.
Resultados. Del total de la muestra, 43 (10.46%) pólipos fueron ≤1cm de diámetro, 16 (4% 3.89%) estuvieron entre 1cm y 2cm, no se encontraron pólipos >2cm y en el resto de resultados no se hallaron estas anomalías. En el grupo de edad de 41 a 50 años se presentaron pólipos en todos los segmentos del colon, pero el de mayor porcentaje (11%) fue el de 71 a 80 años. En el colon izquierdo se presentó el 69% de los pólipos >1cm y el 67% de los <1cm.
Conclusión. En grupos de poblaciones <40 años de edad, los hallazgos de pólipos son bajos en colon izquierdo y muy bajos en colon derecho.
Original research
DOI: https://doi.org/10.15446/revfacmed.v65n3.49484
Results of total colonoscopy in the diagnosis of polyps.
Case studies in Villavicencio, Colombia
Resultados de colonoscopia total en el diagnóstico de pólipos.
Análisis de casos presentados en Villavicencio, Colombia
Received: 04/03/2015. Accepted: 18/06/2016.
Mauricio Alberto Melo-Peñaloza1
1 Universidad Cooperativa de Colombia - Villavicencio Campus- Faculty of Medicine - GRIVI Research Group - Villavicencio - Colombia.
Corresponding author: Mauricio Alberto Melo-Peñaloza. Faculty of Medicine, Universidad Cooperativa de Colombia. Carrera 22 No 7-06, piso 3, Decanatura. Phone number: +57 8 6818850, ext.: 8607. Villavicencio. Colombia. Email: mauricio.melo@campusucc.edu.co.
| Abstract |
Introduction: Any elevation above the normal plane of the colonic mucosa is considered a polypoid projection. As age increases, polyps are more likely to be found; in addition, polyps larger than 1 cm of diameter may potentially lead to a malignant neoplasm.
Objective: To establish the frequency, size, location and age groups of colonic polyp lesions in patients who underwent colonoscopy at Hospital Departamental in Villavicencio during 2009-2014.
Materials and methods: The results of 411 diagnostic colonoscopies were analyzed. Data collection and statistical description was done using SPPSS 2011 software.
Results: 43 (11%) polyps were smaller than 1cm; 16 (4%) were between 1cm and 2cm long; no polyps larger than 2cm were found, and the remaining results did not show any abnormality. Polyps were found in all segments of the colon in the 41-50 age group, but the highest percentage (11%) was observed in the 71-80 age group. 68.7% of polyps larger than 1cm and 67% smaller than 1cm were found in the left colon.
Conclusion: In population groups under 40 years of age, the incidence of polyps is low in the left colon and very low in the right colon.
Keywords: Colonoscopy; Proctosigmoidoscopy, Colonic polyps; Cancer Screening (MeSH).
Melo-Peñaloza MA. Results of total colonoscopy in the diagnosis of polyps. Case studies in Villavicencio, Colombia. Rev. Fac. Med. 2017;65(3):433-9. English. doi: https://doi.org/10.15446/revfacmed.v65n3.49484.
| Resumen |
Introducción. Cualquier levantamiento por encima del plano normal de la mucosa colónica es considerada proyección polipoidea. A mayor edad es más probable encontrar pólipos; además, los >1 cm de diámetro tienen mayor potencial de desarrollar neoplasia maligna.
Objetivo. Establecer la frecuencia de lesiones polipósicas del colon, su tamaño, su localización y los grupos de edades donde están presentes en pacientes a quienes se les realizó colonoscopia en el Hospital Departamental de Villavicencio en el periodo 2009-2014.
Materiales y métodos. Se analizaron los resultados de 411 colonoscopias diagnósticas. La recolección de datos y descripción estadística se hizo con el software SPPSS 2011.
Resultados. Del total de la muestra, 43 (10.46%) pólipos fueron ≤1cm de diámetro, 16 (4% 3.89%) estuvieron entre 1cm y 2cm, no se encontraron pólipos >2cm y en el resto de resultados no se hallaron estas anomalías. En el grupo de edad de 41 a 50 años se presentaron pólipos en todos los segmentos del colon, pero el de mayor porcentaje (11%) fue el de 71 a 80 años. En el colon izquierdo se presentó el 69% de los pólipos >1cm y el 67% de los <1cm.
Conclusión. En grupos de poblaciones <40 años de edad, los hallazgos de pólipos son bajos en colon izquierdo y muy bajos en colon derecho.
Palabras clave: Colonoscopia; Proctosigmoidoscopia, Pólipos del colon (DeCS).
Melo-Peñaloza MA. [Resultados de colonoscopia total en el diagnóstico de pólipos. Análisis de casos presentados en Villavicencio, Colombia]. Rev. Fac. Med. 2017;65(3):433-9. English. doi: https://doi.org/10.15446/revfacmed.v65n3.49484.
Introducción
Any elevation above the normal plane of the colonic mucosa is considered a polypoid projection. Colon polyps may be non-neoplastic, such as inflammatory, hyperplastic, and cystic polyps. Neoplastic polyps (new mucosal growth) may be benign —including tubular, tubulovillous and hairy adenomas— or malignant, and are precursors of colon cancer. Therefore, removing them is important to prevent the development of malignant polyps. The malignant potential of polyps is variable (1).
The World Health Organization classifies neoplastic polyps into: 1) tubular adenomas (tubular epithelial glands) when 20% or less of their architecture is histologically villous, 2) tubulovillous adenomas when a mixed pattern is observed, and 3) hairy adenomas when papillary processes are predominant (2).
Hairy architecture is understood as digitiform or papillary processes made up of connective tissue covered by epithelial cells. They are usually bulkier than tubular and sessile adenomas in most cases. The villous adenoma, due to its histology and bigger volume, has the greatest potential for malignancy, which has been estimated at 5% (2).
The prevalence of adenomas leading to cancer ranges from 0.2% to 11% in endoscopic series of polyp resection; currently, these values are greater due to screening programs. In asymptomatic patients older than 50 years, a prevalence of 0.8% of adenocarcinoma has been estimated, of which 50% is in situ (intramucosal tumor without submucosal invasion) (3).
Adenomas have been found to be larger, more frequent and located on the left side of the colon. A study of 233 414 adenomas found in 142 686 patients showed that those on the right side were smaller (8.2mm vs. 12.4mm) and had a lower percentage of high dysplasia (OR=5.27 95%CI: 4.06-6.82) and adenocarcinomas (OR=4.89, 95% CI: 4.34-5.51) than those on the left side (4).
The size of the adenoma depends on many factors, including age, race, sex and the presence of multiple polyps. Regarding age, a linear relationship may be observed, since size seems to increase in older patients; also, bigger sizes have been found in black population in comparison with white population; regarding sex, they are larger in men than in women, and the probability of a larger size is greater in the presence of multiple polyps (5-7).
Potential malignancy is related to irregular morphology, in other words, if polyps are depressed at the center or ulcerated, if they are immotile (sessile) and if they have no stalk. Size is also influential, since polyps smaller than 1cm, known as advanced neoplasias, are more related with malignancy (8).
Most adenomas do not progress to cancer, but finding tumors larger than 1cm is an indicator of risk for the development of colorectal cancer. In these cases, endoscopic follow-up should be done at shorter intervals after diagnosis (9,10).
About 75% of colorectal cancers come from adenomatous polyps. There is an adenoma-carcinoma sequence that involves a mutation of the APC gene (inactivation) as an early event, followed by accumulation of genetic mutations that activate oncogenes and inhibit suppressor genes. Since there is a strong link between the presence of adenomas and the subsequent risk of developing colorectal cancer, the main objective of colonoscopy screening is to find and remove adenomas for further study, which may prevent the progression of premalignant lesions to malignant lesions (10).
Colonoscopy is an endoscopic study done with a flexible device that allows visualizing the surface of the colon, taking biopsies and resecting lesions found on its surface. It is indicated to study rectorrhagia/hematochezia, chronic diarrhea, changes in intestinal habits, anemia, ulcerative colitis, Crohn’s disease, positive fecal occult blood test, radiological anomalies, and to detect cancer in risk groups (11,12).
From an endoscopic perspective, polyps can be classified as benign or malignant according to the findings. The Kudo classification for colonoscopies with magnification —in which the surface of the adenoma is observed— is divided into: type I, uniform round pits; type II, stellar or papillary pits; type III, large tubular or roundish pits, but smaller than type I pits; type IV, branch-like or gyrus-like pits, and type V, non-structural pits (13).
With this classification, types I and II represent, histologically, hyperplastic or inflammatory polyps, whereas type III, IV and V are neoplastic polyps. This method has a sensitivity of around 89% (95%CI: 85.2-91.9) and specificity of 85.7% (95%CI: 81.3-89.2) (14).
Colon cancer is the third leading cause of death in the USA; in 1999, the age-adjusted incidence was 40.56 per 100 000 inhabitants, and the number of deaths was estimated at 47 900 (15). In 2001, the age-adjusted incidence for Colombia was 11.8 and the age-adjusted mortality rate was 5.87 per 100 000 inhabitants (16).
Several professional associations recommend initiating with screening colonoscopies at age 50; this recommendation is based on the fact that the incidence of colorectal cancer increases around the sixth decade and that, therefore, premalignant lesions could be detected in this age group. Additionally, a greater number of polyp lesions larger than 1cm and advanced neoplasias have also been observed in this group (17).
In the USA screening for colon cancer increased from 38% in 2000 to 53% in 2008 in the population with access to health insurance. Despite this, 53 000 people die every year as a result of colorectal cancer. There is still no agreement as to which is the best screening system because, in the 50-59 age group, only 11% use occult blood test as a screening system; actually, 49.5% use rectosigmoidoscopy for the first time and then sigmoidoscopy in the following 10 years (17). A history of pelvic irradiation or cancer in first-degree relatives are risk factors; therefore, in these cases, a total colonoscopy examination is highly recommended in younger populations (<50 years).
Follow-up of (one or two) polyps of 1cm is recommended once every 5 years, since they are considered as low risk. If 3 to 4 polyps smaller than 1cm are found at colonoscopy, and at least one is larger than 1cm, they are considered as intermediate risk and follow-up should be done every 3 years. When more than five polyps smaller than 1cm and at least 3 larger than 1cm are found, they are considered as high-risk and annual follow-up is advised (18,19).
Colonoscopy in people older than 80 years with a diagnosis of polyps and without associated risk factors has a greater number of complications, so it should be done after carefully considering the pros and cons, even if there are more adenomas smaller than 1cm and advanced adenomas, since life expectancy is clearly lower than in younger age groups (20).
In countries with limited resources such as Colombia, patients can be on long waiting lists for their colon to be examined. It should also be borne in mind that total colonoscopy studies require trained personnel and, in most cases, endoscopy rooms with sufficient capacity to sedate the patient, which increases the cost of the procedure. Therefore, selecting the patients who should undergo a total colonoscopy procedure, both by age and symptomatology, is of great importance in order to optimize the use of this resource.
The objective of this research is to determine the frequency of polyp lesions in the colon, their size, location and the age groups of patients undergoing total colonoscopy in the endoscopy unit of Hospital Departamental in Villavicencio, Colombia.
Materials and methods
This is a descriptive, retrospective, transversal and analytical study in which the reports of diagnostic or screening colonoscopies done until the caecum and performed in the Endoscopy Unit of the Hospital Departmental in Villavicencio between 2009 and 2014 were included. All endoscopies that did not allow reaching and adequately visualizing the caecum due to technical reasons, such as poor preparation, loops or irreducible endoscopic angulations were excluded. Reports in which colon surgery had been proven or in which colon cancer had already been diagnosed by some other diagnostic means were also excluded. The patient information considered for the study were age, endoscopic diagnosis and location of the colon segment, in which the alterations found were ≤1cm, >1cm and ≥2cm.
For this study, the endoscopic diagnosis of polyps in the different segments of the colon was taken into account and histopathological findings were ruled out because they could only be obtained in a few cases. Colonoscopies with diagnoses different from polyps were added to the total amount of performed colonoscopies.
The association between the patient’s symptoms leading to the completion of colonoscopy and polyp findings was not evaluated, as most were not recorded in the examination report. The Kudo endoscopic classification was not evaluated either due to the lack of endoscopes with magnification and narrow-band imaging (NBI).
Statistical analysis
All data were entered into a spreadsheet and analyzed with the statistical package SPSS. Cases with polyps were divided by age groups at 10-year intervals: 20-30, 31-40, 41-50, 51-60, 61-70, 71-80, 81-90 and 91-100. Elevated lesions that might suggest polyps were classified as ≤1cm, >1cm and ≥2cm to establish their frequency in each age group. The size of the polyp was determined by visual estimation and comparison with open colonoscopy biopsy forceps, yielding a size of 0.7cm. The findings in each group were tabulated according to the segment of the colon diagnosed, and the frequency was determined subsequently.
Ethical considerations
According to the Declaration of Helsinki (21) and the Resolution 8430 of the Ministry of Health of Colombia (22), this research does not represent any risk. During the study, respect for the dignity of the subjects and the protection of their data prevailed.
Results
A total of 411 colonoscopies that met the criteria described were analyzed. The mean age was 53 years (SD 14.88, mode 54, minimum 20 and maximum 93). The number of normal colonoscopies was 231 (56%), and 121 (29%) had abnormalities different to polyps. 43 (11%) polyp lesions <1cm, 16 (4%) polyps ≤2cm, and no polyps >2cm were found; the remaining reports did not yield
relevant results.
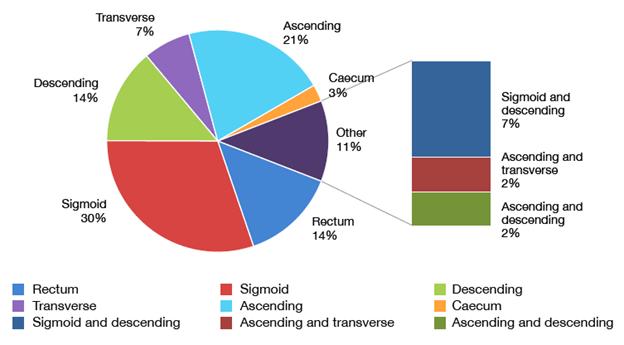
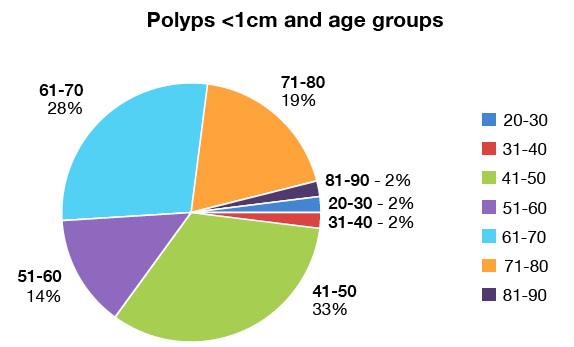
In the 41-50 age group, the mean age was 45 years, the mode 42 years and the SD 2.87; lesions in all segments of the colon, as well as the highest number of polyps <1cm (n=4; 33%) were found in this group. The colon segment with the highest number of polyps found was the sigmoid with 14 cases (33%). In the 51-60, 61-70 and 71-80 age groups, polyps were also found, and the lowest percentage was found among 81-90 (Table 1 and Figure 1 and 2). 67% of all lesions <1cm were found in the left colon (rectum 14%%, sigmoid 32%% and descending colon 19%).
In the 20-30 and 31-40 age groups, only two lesions were found in the rectum, while a significant increase was observed in the 41-50, 51-60, 61-70 and 71-80 age groups. In the 81-90 age group, lesions decreased noticeably. In relation to elevated lesions >1cm, 16 cases were found, which represent 4% of the cases (Table 2).
Only one polyp lesion >1cm was found on the right side of the colon in the 20-30 age group, and one in the 41-50 age group. In all groups >50 years, polyps >1cm were found, with the highest percentage (11%) found in the 71-80 age group. Polyps >1cm in the left colon were found in 69% of the cases.
Table 1. Elevated lesions <1cm, location and age groups.
|
Age groups |
20-30 n=27 |
31-40 n=52 |
41-50 n=95 |
51-60 n=104 |
61-70 n=73 |
71-80 n=47 |
81-90 n=13 |
Total n=411 |
|
Rectum |
1 |
1 |
1 |
1 |
1 |
1 |
0 |
6 |
|
Sigmoid |
0 |
0 |
4 |
3 |
5 |
1 |
0 |
13 |
|
Descending |
0 |
0 |
1 |
1 |
3 |
1 |
0 |
6 |
|
Transverse |
0 |
0 |
2 |
0 |
1 |
0 |
0 |
3 |
|
Ascending |
0 |
0 |
3 |
1 |
1 |
3 |
1 |
9 |
|
Caecum |
0 |
0 |
1 |
0 |
0 |
0 |
0 |
1 |
|
Sigmoid and descending (Simultaneous) |
0 |
0 |
0 |
0 |
1 |
2 |
0 |
3 |
|
Ascending and transverse (Simultaneous) |
0 |
0 |
1 |
0 |
0 |
0 |
0 |
1 |
|
Ascending and descending (Simultaneous) |
0 |
0 |
1 |
0 |
0 |
0 |
0 |
1 |
|
Total |
1 |
1 |
14 |
6 |
12 |
8 |
1 |
43 |
|
Percentage * |
3.7% |
2% |
15% |
6% |
16% |
17% |
7.% |
11% |
* This percentage was estimated based on the number of patients in each age group.
Source: Own elaboration based on the data obtained in the study.

Figure 1. Percentage of polyps <1cm in colon segments.
Source: Own elaboration based on the data obtained in the study.

Figure 2. Percentage of polyps <1cm and age groups.
Source: Own elaboration based on the data obtained in the study.
Table 2. Elevated lesions >1cm, location and age groups.
|
Age groups |
20-30 n=27 |
31-40 n=52 |
41-50 n=95 |
51-60 n=104 |
61-70 n=73 |
71-80 n=47 |
81-90 n=13 |
Total n=411 |
|
Rectum |
0 |
0 |
0 |
1 |
0 |
0 |
1 |
2 |
|
Sigmoid |
0 |
0 |
0 |
2 |
3 |
4 |
0 |
9 |
|
Descending |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
|
Transverse |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
|
Ascending |
0 |
1 |
0 |
2 |
1 |
1 |
0 |
5 |
|
Caecum |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
|
Sigmoid and descending |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
|
Total |
0 |
1 |
0 |
5 |
4 |
5 |
1 |
16 |
|
Percentage * |
0 |
2% |
0 |
5% |
6% |
11% |
8% |
4% |
* This percentage was estimated based on the number of patients in each age group.
Source: Own elaboration based on the data obtained in the study.
Discussion
Polyps <1cm were found in 11% (n=43) of all cases, which is similar to Silva et al. (23) who obtained positive results in 207 (12.54%) cases from sample of 1 650 reports. In a Chilean follow-up program, in which fecal occult blood test was performed for asymptomatic persons >50 years to decide a colonoscopy, a frequency of 40.2% of polyps <1cm was found —476 cases in a sample of 1 184 (24)— indicating that if the test is performed with the intention of finding precursor lesions for cancer, the result is optimized. Such results contrast with this research because the reason for the examination was different in all cases, and the number was not determined in screening cases.
In this series, colonoscopy proved to be an efficient examination tool for the diagnosis of colon polyps; in addition, colonoscopy results showed a significant relationship with age groups, since the 41-50 group, with 14 cases (14.73%), had the highest number of polyps smaller than 1cm, as well as 32.55 % of total polyps regardless of size.
In Ko & Youn’s study (25), with a sample of 3 114 colonoscopies, the frequency of polyps in the 40-49 age group was 42.7% (440 cases in a sample of 1 038 reports) —these authors make reference to any polyp size. The study by Bafandeh (26), done in a low prevalence area with 480 colonoscopies, reported that 12.2% of polyps were found in the 40-49 group; size was not specified either. An Iranian series of 240 reports, considered as low frequency, showed 21 cases (8.75%) of polyps <1cm in a group 4 050 samples (27).
On the other hand, the findings of this research are similar to those obtained by Rundle et al. (28), who found that 135 out of 905 colonoscopies showed elevated lesions, and that these lesions represented 14% in the 40-49 age group and in 16% the group of 50-59; in the latter group, a greater number and larger sizes were observed, as well as cancer.
Regarding localization, 67% of the polyps <1cm were on the left side of the colon (rectum, sigmoid and descending). A similar result was found in the series by Silva et al. (23) with 71.4% (n=148) and in an Iranian series with 80.4% (n=193); the latter did not establish if they were bigger or smaller than 1cm, but reported a greater proportion of high-grade dysplasia on the left side (29). An Italian series found 59 cases (53.15%) of polyps on the left side of the colon in a sample of 111 reports (30). Bafandeh et al. (26) also reported that 72% of the polyps were found on the left side of the colon (26% descending, 26% sigmoid and 20% rectal). Eshghi et al. (31) found in a retrospective study that the percentage of adenomatous polyps on the left side of the colon was 60.44%. These findings may indicate that the study of the left side of the colon remains important for follow-up of in populations at risk (32).
If OR (odds ratio) in the Ko & Youn series (25) is considered, the value for type of neoplasia in the colon, including adenoma and cancer, was 2.38 for the 40-50 age group (95%CI: 1.79-3.17), 4.73 in the 50-60 age group (95%CI: 3.55-6.30) and 5.42 in the 60-70 age group (95%CI: 3.89-7.56). The study by Giuliani et al. (30) showed that the OR in people >55 years is 5.1 (95%CI: 4.15-6.33) compared to all <55, regarding polyps. The research of Morimoto et al. (32) reported that the OR for adenomatous polyps in the 40-49 age group was 1.5 (95%CI: 0.9-2.6), whereas for the 50-59 group was 2.3 (95%CI: 1.4-3.9), and 3.8 (95%CI: 2.3-6.3) for the 60-69 group. The description in this study and the quoted series show an increased possibility of finding polyps in the age groups over 40; performing a total colonoscopy is crucial among population this age.
In all the studies reviewed, polyps >1cm were found in the age groups >50; the group with the highest percentage of polyps was 71-80 with 10.6%, and the most frequent location was the left side of the colon with 11 cases (68.7%). Only one polyp lesion >1cm was found on the right side of the colon in the 20-30 and 41-50 groups. The Ko & Youn series (25) described polyps >1cm in 4 (0.8%) of the 483 reports on the 30-40 group, 44 (3.7%) out of 1 200 reports in the 40-50 group, and 77 (7.5 %) out of 1 038 reports on the 60-70 group.
In the specific follow-up program of Castells et al. (33), 493 cases (9.74%) were found in 5 059 reports, of which 244 were observed in the left colon; the 50-59 group had 132 cases and the 60-69 group, 175. In the study by Terhaar Sive Droste et al. (34), in which the usefulness of colonoscopy in the follow-up of individuals >50 years of age was evaluated, polyps >1cm were found in 496 cases (10.72%) in a sample of 4 623 reports, 67% of them in the left colon, 13% in the 50-60 group, 17% in the 60-70 group, and 20% in the 70-80 group. In a series with seniors with a mean age of 62 years, 228 (7.3%) cases of polyposis lesions >1cm were found in a sample of 3 121 reports. These reviews showed that if colonoscopy is done in the context of an established follow-up program, the probability of finding lesions >1cm increases.
In groups <40 years, the frequency of polyps is low; this research found only two polyps in the 21-30 and 31-40 groups, which were located in the rectum. Similarly, in a Korean series, 71 (14.7%) cases were found in the 30-39 group (25); Zare-Mirzaie et al. (27) described a frequency of 1.25% in <20 years, 0.8% in the 20-29 group, and 5.41% in the 30-39 group, 76.5% of which were located on the left side of the colon. Morimoto et al. (32) found 23 cases (5.26%) <40 years in a sample of 437 reports. Eshghi et al. (31) found 5.40% in the 18-30 group and 11.90% in the 31-40 group. These numbers suggest that rectosigmoidoscopy examination would be sufficient for patients <40 in the absence of risk factors and clinical or laboratory findings (35-37).
This description has several limitations, such as sex, height, weight, body mass index, alcohol or cigarette consumption, as well as the impossibility of finding and correlating pathological studies. Another limitation relates to the population studied since it is not at risk, therefore it is not a screening sample; however, even with these restrictions, the similarity with other series is striking, especially when addressing factors such as age and limitations (38).
Conclusions
The frequency of polyps in the colon, both smaller and greater than 1cm, is similar to the international series. The age group in which these lesions begin to be reported is 41-50 years; in younger groups, findings in the left colon are less common. Adequate use of resources indicates that the rectosigmoidoscopy study is sufficient for people <40 years old, who do not present risk factors or abnormal laboratory indicators, and that colonoscopy would be indicated for the early detection of polyps in the 40-50 group.
If finding colon cancer at earlier stages of development is the goal, screening programs should be directed to persons at risk >50 years of age, just like programs for controlling hypertension or diabetes. Likewise, other studies are necessary to establish an association between the presence of polyps, their location and histopathological alterations.
Conflict of interests
None stated by the author.
Funding
None stated by the author.
Acknowledgement
I would like to thank Henry Horta Sanz, a sixth semester student of Medicine at the Universidad Cooperativa de Colombia, for registering in the database the information extracted from colonoscopy reports of 142 patients, to Giovanna Cocunubo for supporting this research, and to Dr. Norton Pérez for his reviews and suggestions.
References
1.Acheson AG, Scholefield JH. Colorectal cancer: screening and surveillance. In: Hawkey CJ, Bosch J, Richter JE, García-Tsa G, Chan FKL, editors. Textbook of Clinical Gastroenterology and hepatology. 2nd ed. Oxford: Wiley-Blackwell; 2012. p. 438-443.
2.Bosman FT, Carneiro F, Hruban RH. WHO Classification of Tumours of the Digestive System. 4th ed. Geneva: World Health Organization; 2010.
3.Bujanda L, Cosme A, Gil I, Arenas-Mirave J. Malignant colorectal polyps. World J Gastroenterol. 2010;16(25):3103-11.
4.Gupta S, Balasubramanian BA, Fu T, Genta RM, Lash R. Polyps with advanced neoplasia are smaller in the right than in the left colon: implications for colorectal cancer screening. Clin Gastroenterol Hepatol. 2012;10(12):1395-1401. http://doi.org/f2j4nn.
5.Lowenfels AB, Williams JL, Holub JL, Maisonneuve P, Lieberman DA. Determinants of polyp size in patients undergoing screening colonoscopy. BMC Gastroenterol. 2011;11:101. http://doi.org/c6wggq.
6.Ahmad A, Frank BB. Women´s issues in gastroenterology. Preface. Gastroenterology Clin North Am. 2011;40(2):xiii-xiv. http://doi.org/dd6hb6.
7.Brenner H, Hoffmeister M, Arndt V, Haug U. Gender differences in colorectal cancer: implications for age at initiation of screening. Br J Cancer. 2007;96(5):828-31. http://doi.org/cf6xss.
8.Bujanda L, Cosme A, Gil I, Arenas-Mirave JI. Malignant colorectal polips. World J Gastroenterol. 2010;16(25):3103-11. http://doi.org/cbf6pk.
9.Burnett-Hartman AN, Newcomb PA, Phipps AI, Passarelli MN, Grady WM, Upton MP, et al. Colorectal endoscopy, advanced adenomas, and sessile serrated polyps: implications for proximal colon cancer. Am J Gastroenterol. 2012;107(8):1213-9. http://doi.org/f39hc8.
10.Markowitz SD, Bertagnolli MM. Molecular origins of cancer: Molecular basis of colorectal cancer. N Engl J Med. 2009;361(25):2449-60. http://doi.org/cr398j.
11.de la Peña J, Diaz A, Moraleja I. Indicaciones de la colonoscopia, rectoscopia y anuscopia. Medicine. 2012;11(7):451-4. http://doi.org/f27qb4.
12.Waye J. Lower gastrointestinal endoscopy and biopsy. In: Hawkey CJ, Bosch J, Richter JE, García-Tsa G, Chan FKL, editors. Textbook of Clinical Gastroenterology and hepatology. 2nd edition. Oxford: Wiley-Blackwell; 2012. p. 936-942.
13.The Paris endoscopic classification of superficial neoplastic lesions: esophagus, stomach, and colon: November 30 to December 1, 2002. Gastrointest Endosc. 2003;58(Supple 6):S3-43. http://doi.org/d3wr28.
14.Li M, Ali SM, Umm-a-OmarahGilani S, Liu J, Li YQ, Zuo XL. Kudo’s pit pattern classification for colorectal neoplasms: A meta-analysis. World J Gastroenterol. 2014;20(35):12649-56. http://doi.org/f6gznk.
15.Lagares-Garcia JA, Kurek S, Collier B, Diaz F, Schilli R, Richey J, et al. Colonoscopy in octogenarians and older patients. Surg Endosc. 2001;15(3):262-5. http://doi.org/frd49r.
16.Cardona-Villamizar HJ, Otero-Regino W, Forero-Piñeros EA, Gutierrez-Ceballos O. Significado de los pólipos en colon distal, en una población de un país en vía de desarrollo: prevalencia y asociación con neoplasia proximal sincrónica. Rev Colomb Gastroenterol. 2004;19(4):253-62.
17.Overholt BF, Brooks-Belli L, Grace MG, Rankin K, Harrell R, Turyk M, et al. Evaluating Screening Age for Colonoscopy: A Quality Assurance Assessment. J Clin Gastroenterol. 2010;44(7):e147-53. http://doi.org/bszrgz.
18.Centers for Disease Control and Prevention (CDC). Vital Signs: Colorectal Cancer Screening Among Adults Aged 50-75 Years. United States, 2008. MMWR. 2010;59(26);808-12.
19.Hassan C, Repici A, Zullo A, Sharma P. New Paradigms for Colonoscopic Management of Diminutive Colorectal Polyps: Predict, Resect, and Discard or Do Not Resect? Clin Endosc. 2013;46(2):130-7. http://doi.org/f4txcg.
20.Lin OS. Performing colonoscopy in elderly and very elderly patients: Risks, costs and benefits. World J Gastrointest Endosc. 2014;16(6):220-6. http://doi.org/b6qv.
21.Asociación Médica Mundial. Declaración de Helsinki de la Asociación Médica Mundial. Principios éticos para las investigaciones médicas en seres humanos. Fortaleza: 64a Asamblea General de la AMM; 2013 [cited 2014 Dec 20]. Available from: https://goo.gl/hvf7l1.
22.Colombia. Ministerio de Salud. Resolución 8430 de 1993 (octubre 4): Por la cual se establecen las normas científicas, técnicas y administrativas para la investigación en salud. Bogotá D.C.; octubre 4 de 1993.
23.Silva SM, Rosa VF, Santos AC, RM, Oliveira PG, Susa JB. Influence of patients age and colorectal polips size on histopatholgy findings. Arq Bras Cir Dig. 2014;27(2):109-13. http://doi.org/b6pp.
24.López-Köstner F, Kronber U, Zárate AJ, Wielandt AM, Pinto E, Suazo C, et al. Programa de detección de neoplasias colorrectales en población mayor de 50 años. Rev Med Chil. 2012;140(3):281-6. http://doi.org/b6qw.
25.Ko HJ, Youn CH. Determination of the beginning age for colonoscopic screening among colonoscopy-naïve individuals. Clin Res Hepatol Gastroenterol. 2012;36(4):384-90. http://doi.org/f4bw6h.
26.Bafandeh Y, Khoshbaten M, Eftekhar Sadat AT, Farhang S. Clinical predictors of colorectal polyps and carcinoma in a low prevalence region: Results of a colonoscopy based study. World J Gastroenterol. 2008;14(10):1534-8.
27.Zare-Mirzaie A, Abolhasani M, Aryamanesh A. Left sided colorectal adenomatous polyps have more risk for high grade dysplasia. Acta Med Iran. 2013;51(3):172-7.
28.Rundle AG, Lebwohl B, Vogel R, Levine S, Neugut AI. Colonoscopic screening in average -isk individual ages 40 to 49 vs 50 to 59 years. Gastroenterology. 2008;134(5):1311-5. http://doi.org/dq6mkk.
29.Iravani S, Kashfi SM, Azimzadeh P, Lashkari MH. Prevalence and characteristics of colorectal polyps in symptomatic and asymptomatic Iranian patients undergoing colonoscopy from 2009-2013. Asian Pac J Cancer Prev. 2014;15(22):9933-7. http://doi.org/b6qx.
30.Giuliani A, Caporale A, Corona M, Ricciardulli T, Di Bari M, Demoro M, et al. Large size, villous content and distal location are associated with severe dysplasia in colorectal adenomas. Anticancer Res. 2006;26(5B):3717-22.
31.Eshghi MJ, Fatemi R, Hashemy A, Aldulaimi D, Khodadoostan M. A retrospective study of patients with colorectal polyps. Gastroenterol Hepatol Bed Bench. 2011;4(1):17-22.
32.Morimoto LM, Newcomb PA, Ulrich CM, Bostick RM, Lais CJ, Potter JD. Risk factors for hyperplastic and adenomatous polyps: evidence for malignant potential? Cancer Epidemiol Biomarkers Prev. 2002;11(10 Pt 1):1012-8.
33.Castells A, Bessa X, Quintero E, Bujanda L, Cubiella J, Salas D, et al. Risk of advanced proximal neoplasms according to distal colorectal findings: comparison of sigmoidoscopy-based strategies. J Natl Cancer Inst. 2013;105(12):878-86. http://doi.org/f43c9p.
34.Terhaar Sive Droste JS, Craanen ME, van der Hulst RWM, Bartelsman JF, Bezemer DP, Cappendijk KR, et al. Colonoscopic yield of colorectal neoplasia in dailyclinical practice. World J Gastroenterol. 2009;15(9):1085-92. http://doi.org/d8dtrk.
35.Segnan N, Armaroli P, Bonelli L, Risio M, Scioallero S, Zappa M, et al. Once-Only Sigmoidoscopy in Colorectal Cancer Screening: Follow-up Findings of the Italian Randomized Controlled Trial—SCORE. J Natl Cancer. 2011;103(17):1310-22. http://doi.org/cz9ddx.
36.Wang FW, Hsu PI, Chuang HY, Tu MS, Mar GY, King TM, et al. Prevalence and risk factors of asymptomatic colorectal polyps in taiwan. Gastroenterol Res Pract. 2014;2014:985205. http://doi.org/f58gkv.
37.Binda V, Pereira-Lima J, Nunes CA, Falkemberg LT, Azambuja DB, Cruz JV. Is there a role for sigmoidoscopy in symptomatic patients? Analysis of a study correlating distal and proximal colonic neoplasias detected by colonoscopy in a symptomatic population. Arg Gastroenterol. 2007;4(1):2-7. http://doi.org/b97t4w.
38.Marderstein EL, Church JM. Classic “outlet” rectal bleeding does not require full colonoscopy to exclude significant pathology. Dis Colon Rectum. 2008;51(2):202-6. http://doi.org/b9pmqn.
Iván “Ivanquio” Benavides
“El niño vacío” – 003
Técnica: tinta, color digital
Recibido: 4 de marzo de 2015; Aceptado: 18 de junio de 2016
Abstract
Introduction:
Any elevation above the normal plane of the colonic mucosa is considered a polypoid projection. As age increases, polyps are more likely to be found; in addition, polyps larger than 1 cm of diameter may potentially lead to a malignant neoplasm.
Objective:
To establish the frequency, size, location and age groups of colonic polyp lesions in patients who underwent colonoscopy at Hospital Departamental in Villavicencio during 2009-2014.
Materials and methods:
The results of 411 diagnostic colonoscopies were analyzed. Data collection and statistical description was done using SPPSS 2011 software.
Results:
43 (11%) polyps were smaller than 1cm; 16 (4%) were between 1cm and 2cm long; no polyps larger than 2cm were found, and the remaining results did not show any abnormality. Polyps were found in all segments of the colon in the 41-50 age group, but the highest percentage (11%) was observed in the 71-80 age group. 68.7% ofpolyps larger than 1cm and 67% smaller than 1cm were found in the left colon.
Conclusion:
In population groups under 40 years of age, the incidence of polyps is low in the left colon and very low in the right colon.
Keywords:
Colonoscopy, Proctosigmoidoscopy, Colonic polyps, Cancer Screening (MeSH).Resumen
Introducción.
Cualquier levantamiento por encima del plano normal de la mucosa colónica es considerada proyección polipoidea. A mayor edad es más probable encontrar pólipos; además, los >1 cm de diámetro tienen mayor potencial de desarrollar neoplasia maligna.
Objetivo.
Establecer la frecuencia de lesiones polipósicas del colon, su tamaño, su localización y los grupos de edades donde están presentes en pacientes a quienes se les realizó colonoscopia en el Hospital Departamental de Villavicencio en el periodo 2009-2014.
Materiales y métodos.
Se analizaron los resultados de 411 colonoscopias diagnósticas. La recolección de datos y descripción estadística se hizo con el software SPPSS 2011.
Resultados.
Del total de la muestra, 43 (10.46%) pólipos fueron <1cm de diámetro, 16 (4% 3.89%) estuvieron entre 1cm y 2cm, no se encontraron pólipos >2cm y en el resto de resultados no se hallaron estas anomalías. En el grupo de edad de 41 a 50 años se presentaron pólipos en todos los segmentos del colon, pero el de mayor porcentaje (11%) fue el de 71 a 80 años. En el colon izquierdo se presentó el 69% de los pólipos >1cm y el 67% de los <1cm.
Conclusión.
En grupos de poblaciones <40 años de edad, los hallazgos de pólipos son bajos en colon izquierdo y muy bajos en colon derecho.
Palabras clave:
Colonoscopia, Proctosigmoidoscopia, Pólipos del colon (DeCS).Introducción
Any elevation above the normal plane of the colonic mucosa is considered a polypoid projection. Colon polyps may be non-neoplastic, such as inflammatory, hyperplastic, and cystic polyps. Neoplastic polyps (new mucosal growth) may be benign -including tubular, tubulo villous and hairy adenomas- or malignant, and are precursors of colon cancer. Therefore, removing them is important to prevent the development of malignant polyps. The malignant potential of polyps is variable 1.
The World Health Organization classifies neoplastic polyps into: 1) tubular adenomas (tubular epithelial glands) when 20% or less of their architecture is histologically villous, 2) tubulovillous adenomas when a mixed pattern is observed, and 3) hairy adenomas when papillary processes are predominant 2.
Hairy architecture is understood as digitiform or papillary processes made up of connective tissue covered by epithelial cells. They are usually bulkier than tubular and sessile adenomas in most cases. The villous adenoma, due to its histology and bigger volume, has the greatest potential for malignancy, which has been estimated at 5% 2.
The prevalence of adenomas leading to cancer ranges from 0.2% to 11% in endoscopic series of polyp resection; currently, these values are greater due to screening programs. In asymptomatic patients older than 50 years, a prevalence of 0.8% of adenocarcinoma has been estimated, of which 50% is in situ (intramucosal tumor without submucosal invasion) 3.
Adenomas have been found to be larger, more frequent and located on the left side of the colon. A study of 233 414 adenomas found in 142 686 patients showed that those on the right side were smaller (8.2mm vs. 12.4mm) and had a lower percentage of high dysplasia (OR=5.27 95%CI: 4.06-6.82) and adenocarcinomas (OR=4.89, 95% CI: 4.34-5.51) than those on the left side 4.
The size of the adenoma depends on many factors, including age, race, sex and the presence of multiple polyps. Regarding age, a linear relationship may be observed, since size seems to increase in older patients; also, bigger sizes have been found in black population in comparison with white population; regarding sex, they are larger in men than in women, and the probability of a larger size is greater in the presence of multiple polyps 5-7.
Potential malignancy is related to irregular morphology, in other words, if polyps are depressed at the center or ulcerated, if they are immotile (sessile) and if they have no stalk. Size is also influential, since polyps smaller than 1cm, known as advanced neoplasias, are more related with malignancy 8.
Most adenomas do not progress to cancer, but finding tumors larger than 1cm is an indicator of risk for the development of colorectal cancer. In these cases, endoscopic follow-up should be done at shorter intervals after diagnosis 9,10.
About 75% of colorectal cancers come from adenomatous polyps. There is an adenoma-carcinoma sequence that involves a mutation of the APC gene (inactivation) as an early event, followed by accumulation of genetic mutations that activate oncogenes and inhibit suppressor genes. Since there is a strong link between the presence of adenomas and the subsequent risk of developing colorectal cancer, the main objective of colonoscopy screening is to find and remove adenomas for further study, which may prevent the progression of premalignant lesions to malignant lesions 10.
Colonoscopy is an endoscopic study done with a flexible device that allows visualizing the surface of the colon, taking biopsies and resecting lesions found on its surface. It is indicated to study rectorrhagia/hematochezia, chronic diarrhea, changes in intestinal habits, anemia, ulcerative colitis, Crohn's disease, positive fecal occult blood test, radiological anomalies, and to detect cancer in risk groups 11,12.
From an endoscopic perspective, polyps can be classified as benign or malignant according to the findings. The Kudo classification for colonoscopies with magnification -in which the surface of the adenoma is observed- is divided into: type I, uniform round pits; type II, stellar or papillary pits; type III, large tubular or roundish pits, but smaller than type I pits; type IV, branch-like or gyrus-like pits, and type V, non-structural pits 13.
With this classification, types I and II represent, histologically, hyperplastic or inflammatory polyps, whereas type III, IV and V are neoplastic polyps. This method has a sensitivity of around 89% (95%CI: 85.2-91.9) and specificity of 85.7% (95%CI: 81.3-89.2) 14.
Colon cancer is the third leading cause of death in the USA; in 1999, the age-adjusted incidence was 40.56 per 100 000 inhabitants, and the number of deaths was estimated at 47 900 15. In 2001, the age-adjusted incidence for Colombia was 11.8 and the age-adjusted mortality rate was 5.87 per 100 000 inhabitants 16.
Several professional associations recommend initiating with screening colonoscopies at age 50; this recommendation is based on the fact that the incidence of colorectal cancer increases around the sixth decade and that, therefore, premalignant lesions could be detected in this age group. Additionally, a greater number of polyp lesions larger than 1cm and advanced neoplasias have also been observed in this group 17.
In the USA screening for colon cancer increased from 3 8% in 2000 to 53% in 2008 in the population with access to health insurance. Despite this, 53 000 people die every year as a result of colorectal cancer. There is still no agreement as to which is the best screening system because, in the 50-59 age group, only 11% use occult blood test as a screening system; actually, 49.5% use rectosigmoidoscopy for the first time and then sigmoidoscopy in the following 10 years 17. A history of pelvic irradiation or cancer in first-degree relatives are risk factors; therefore, in these cases, a total colonoscopy examination is highly recommended in younger populations (<50 years).
Follow-up of (one or two) polyps of 1cm is recommended once every 5 years, since they are considered as low risk. If 3 to 4 polyps smaller than 1cm are found at colonoscopy, and at least one is larger than 1cm, they are considered as intermediate risk and follow-up should be done every 3 years. When more than five polyps smaller than 1cm and at least 3 larger than 1cm are found, they are considered as high-risk and annual follow-up is advised 18,19.
Colonoscopy in people older than 80 years with a diagnosis ofpolyps and without associated risk factors has a greater number of complications, so it should be done after carefully considering the pros and cons, even if there are more adenomas smaller than 1cm and advanced adenomas, since life expectancy is clearly lower than in younger age groups 20.
In countries with limited resources such as Colombia, patients can be on long waiting lists for their colon to be examined. It should also be borne in mind that total colonoscopy studies require trained personnel and, in most cases, endoscopy rooms with sufficient capacity to sedate the patient, which increases the cost of the procedure. Therefore, selecting the patients who should undergo a total colonoscopy procedure, both by age and symptomatology, is of great importance in order to optimize the use of this resource.
The objective of this research is to determine the frequency of polyp lesions in the colon, their size, location and the age groups of patients undergoing total colonoscopy in the endoscopy unit of Hospital Departamental in Villavicencio, Colombia.
Materials and methods
This is a descriptive, retrospective, transversal and analytical study in which the reports of diagnostic or screening colonoscopies done until the caecum and performed in the Endoscopy Unit of the Hospital Departmental in Villavicencio between 2009 and 2014 were included. All endoscopies that did not allow reaching and adequately visualizing the caecum due to technical reasons, such as poor preparation, loops or irreducible endoscopic angulations were excluded. Reports in which colon surgery had been proven or in which colon cancer had already been diagnosed by some other diagnostic means were also excluded. The patient information considered for the study were age, endoscopic diagnosis and location of the colon segment, in which the alterations found were <1cm, >1cm and >2cm.
For this study, the endoscopic diagnosis of polyps in the different segments of the colon was taken into account and histopathological findings were ruled out because they could only be obtained in a few cases. Colonoscopies with diagnoses different from polyps were added to the total amount of performed colonoscopies.
The association between the patient's symptoms leading to the completion of colonoscopy and polyp findings was not evaluated, as most were not recorded in the examination report. The Kudo endoscopic classification was not evaluated either due to the lack of endoscopes with magnification and narrow-band imaging (NBI).
Statistical analysis
All data were entered into a spreadsheet and analyzed with the statistical package SPSS. Cases with polyps were divided by age groups at 10-year intervals: 20-30, 31-40, 41-50, 51-60, 61-70, 7180, 81-90 and 91-100. Elevated lesions that might suggest polyps were classified as <1cm, >1cm and >2cm to establish their frequency in each age group. The size of the polyp was determined by visual estimation and comparison with open colonoscopy biopsy forceps, yielding a size of 0.7cm. The findings in each group were tabulated according to the segment of the colon diagnosed, and the frequency was determined subsequently.
Ethical considerations
According to the Declaration of Helsinki 21 and the Resolution 8430 of the Ministry of Health of Colombia 22, this research does not represent any risk. During the study, respect for the dignity of the subjects and the protection of their data prevailed.
Results
A total of 411 colonoscopies that met the criteria described were analyzed. The mean age was 53 years (SD 14.88, mode 54, minimum 20 and maximum 93). The number of normal colonoscopies was 231 (56%), and 121 (29%) had abnormalities different to polyps. 43 (11%) polyp lesions <1cm, 16 (4%) polyps <2cm, and no polyps >2cm were found; the remaining reports did not yield relevant results.
In the 41-50 age group, the mean age was 45 years, the mode 42 years and the SD 2.87; lesions in all segments of the colon, as well as the highest number ofpolyps <1cm (n=4; 33%) were found in this group. The colon segment with the highest number of polyps found was the sigmoid with 14 cases (33%). In the 51-60, 61-70 and 71-80 age groups, polyps were also found, and the lowest percentage was found among 81-90 (Table 1 and Figure 1 and 2). 67% of all lesions <1cm were found in the left colon (rectum 14%%, sigmoid 32%% and descending colon 19%).
* This percentage was estimated based on the number of patients in each age group. Source: Own elaboration based on the data obtained in the study.Table 1: Elevated lesions <1cm, location and age groups.

Figure 1: Percentage of polyps <1cm in colon segments.
Figure 2: Percentage of polyps <1cm and age groups.
In the 20-30 and 31-40 age groups, only two lesions were found in the rectum, while a significant increase was observed in the 41-50, 51-60, 61-70 and 71-80 age groups. In the 81-90 age group, lesions decreased noticeably. In relation to elevated lesions >1cm, 16 cases were found, which represent 4% of the cases (Table 2).
* This percentage was estimated based on the number of patients in each age group. Source: Own elaboration based on the data obtained in the study.Table 2: Elevated lesions >1cm, location and age groups.

Only one polyp lesion >1cm was found on the right side of the colon in the 20-30 age group, and one in the 41-50 age group. In all groups >50 years, polyps >1cm were found, with the highest percentage (11%) found in the 71-80 age group. Polyps >1cm in the left colon were found in 69% of the cases.
Discussion
Polyps <1cm were found in 11% (n=43) of all cases, which is similar to Silva et al. 23 who obtained positive results in 207 (12.54%) cases from sample of 1 650 reports. In a Chilean follow-up program, in which fecal occult blood test was performed for asymptomatic persons >50 years to decide a colonoscopy, a frequency of 40.2% of polyps <1cm was found -476 cases in a sample of 1 184 (24)- indicating that if the test is performed with the intention of finding precursor lesions for cancer, the result is optimized. Such results contrast with this research because the reason for the examination was different in all cases, and the number was not determined in screening cases.
In this series, colonoscopy proved to be an efficient examination tool for the diagnosis of colon polyps; in addition, colonoscopy results showed a significant relationship with age groups, since the 41-50 group, with 14 cases (14.73%), had the highest number of polyps smaller than 1cm, as well as 32.55 % of total polyps regardless of size.
In Ko & Youn's study 25, with a sample of 3 114 colonoscopies, the frequency of polyps in the 40-49 age group was 42.7% (440 cases in a sample of 1 038 reports) -these authors make reference to any polyp size. The study by Bafandeh 26, done in a low prevalence area with 480 colonoscopies, reported that 12.2% of polyps were found in the 40-49 group; size was not specified either. An Iranian series of240 reports, considered as low frequency, showed 21 cases (8.75%) of polyps <1cm in a group 4 050 samples 27.
On the other hand, the findings of this research are similar to those obtained by Rundle et al. 28, who found that 135 out of 905 colonoscopies showed elevated lesions, and that these lesions represented 14% in the 40-49 age group and in 16% the group of 50-59; in the latter group, a greater number and larger sizes were observed, as well as cancer.
Regarding localization, 67% of the polyps <1cm were on the left side of the colon (rectum, sigmoid and descending). A similar result was found in the series by Silva et al. 23 with 71.4% (n=148) and in an Iranian series with 80.4% (n=193); the latter did not establish if they were bigger or smaller than 1cm, but reported a greater proportion of high-grade dysplasia on the left side 29. An Italian series found 59 cases (53.15%) of polyps on the left side of the colon in a sample of 111 reports 30. Bafandeh et al. 26 also reported that 72% of the polyps were found on the left side of the colon (26% descending, 26% sigmoid and 20% rectal). Eshghi et al. 31 found in a retrospective study that the percentage of adenomatous polyps on the left side of the colon was 60.44%. These findings may indicate that the study of the left side of the colon remains important for follow-up of in populations at risk 32.
If OR (odds ratio) in the Ko & Youn series 25 is considered, the value for type of neoplasia in the colon, including adenoma and cancer, was 2.38 for the 40-50 age group (95%CI: 1.79-3.17), 4.73 in the 50-60 age group (95%CI: 3.55-6.30) and 5.42 in the 60-70 age group (95%CI: 3.89-7.56). The study by Giuliani et al. 30 showed that the OR in people >55 years is 5.1 (95%CI: 4.15-6.33) compared to all <55, regarding polyps. The research of Morimoto et al. 32 reported that the OR for adenomatous polyps in the 40-49 age group was 1.5 (95%CI: 0.9-2.6), whereas for the 50-59 group was 2.3 (95%CI: 1.4-3.9), and 3.8 (95%CI: 2.3-6.3) for the 60-69 group. The description in this study and the quoted series show an increased possibility of finding polyps in the age groups over 40; performing a total colonoscopy is crucial among population this age.
In all the studies reviewed, polyps >1cm were found in the age groups >50; the group with the highest percentage of polyps was 71-80 with 10.6%, and the most frequent location was the left side of the colon with 11 cases (68.7%). Only one polyp lesion >1cm was found on the right side of the colon in the 20-30 and 41-50 groups. The Ko & Youn series 25 described polyps >1cm in 4 (0.8%) of the 483 reports on the 30-40 group, 44 (3.7%) out of 1 200 reports in the 40-50 group, and 77 (7.5 %) out of 1 038 reports on the 60-70 group.
In the specific follow-up program of Castells et al. 33, 493 cases (9.74%) were found in 5 059 reports, of which 244 were observed in the left colon; the 50-59 group had 132 cases and the 60-69 group, 175. In the study by Terhaar Sive Droste et al. 34, in which the usefulness of colonoscopy in the follow-up of individuals >50 years of age was evaluated, polyps >1cm were found in 496 cases (10.72%) in a sample of4 623 reports, 67% of them in the left colon, 13% in the 50-60 group, 17% in the 60-70 group, and 20% in the 70-80 group. In a series with seniors with a mean age of 62 years, 228 (7.3%) cases of polyposis lesions >1cm were found in a sample of 3 121 reports. These reviews showed that if colonoscopy is done in the context of an established follow-up program, the probability of finding lesions >1cm increases.
In groups <40 years, the frequency of polyps is low; this research found only two polyps in the 21-30 and 31-40 groups, which were located in the rectum. Similarly, in a Korean series, 71 (14.7%) cases were found in the 30-39 group 25; Zare-Mirzaie et al. 27 described a frequency of 1.25% in <20 years, 0.8% in the 20-29 group, and 5.41% in the 30-39 group, 76.5% of which were located on the left side of the colon. Morimoto et al. 32 found 23 cases (5.26%) <40 years in a sample of 437 reports. Eshghi et al. 31 found 5.40% in the 18-30 group and 11.90% in the 31-40 group. These numbers suggest that rectosigmoidoscopy examination would be sufficient for patients <40 in the absence of risk factors and clinical or laboratory findings 35-37.
This description has several limitations, such as sex, height, weight, body mass index, alcohol or cigarette consumption, as well as the impossibility of finding and correlating pathological studies. Another limitation relates to the population studied since it is not at risk, therefore it is not a screening sample; however, even with these restrictions, the similarity with other series is striking, especially when addressing factors such as age and limitations 38.
Conclusions
The frequency of polyps in the colon, both smaller and greater than 1cm, is similar to the international series. The age group in which these lesions begin to be reported is 41-50 years; in younger groups, findings in the left colon are less common. Adequate use of resources indicates that the rectosigmoidoscopy study is sufficient for people <40 years old, who do not present risk factors or abnormal laboratory indicators, and that colonoscopy would be indicated for the early detection of polyps in the 40-50 group.
If finding colon cancer at earlier stages of development is the goal, screening programs should be directed to persons at risk >50 years of age, just like programs for controlling hypertension or diabetes. Likewise, other studies are necessary to establish an association between the presence of polyps, their location and histopathological alterations.
Acknowledgement
I would like to thank Henry Horta Sanz, a sixth semester student of Medicine at the Universidad Cooperativa de Colombia, for registering in the database the information extracted from colonoscopy reports of 142 patients, to Giovanna Cocunubo for supporting this research, and to Dr. Norton Pérez for his reviews and suggestions.
References
Referencias
Acheson AG, Scholefield JH. Colorectal cancer: screening and surveillance. In: Hawkey CJ, Bosch J, Richter JE, García-Tsa G, Chan FKL, editors. Textbook of Clinical Gastroenterology and hepatology. 2nd ed. Oxford: Wiley-Blackwell; 2012. p. 438-443.
Bosman FT, Carneiro F, Hruban RH. WHO Classification of Tumours of the Digestive System. 4th ed. Geneva: World Health Organization; 2010.
Bujanda L, Cosme A, Gil I, Arenas-Mirave J. Malignant colorectal polyps. World J Gastroenterol. 2010;16(25):3103-11.
Gupta S, Balasubramanian BA, Fu T, Genta RM, Lash R. Polyps with advanced neoplasia are smaller in the right than in the left colon: implications for colorectal cancer screening. Clin Gastroenterol Hepatol. 2012;10(12):1395-1401. http://doi.org/f2j4nn.
Lowenfels AB, Williams JL, Holub JL, Maisonneuve P, Lieberman DA. Determinants of polyp size in patients undergoing screening colonoscopy. BMC Gastroenterol. 2011;11:101. http://doi.org/c6wggq.
Ahmad A, Frank BB. Women´s issues in gastroenterology. Preface. Gastroenterology Clin North Am. 2011;40(2):xiii-xiv. http://doi.org/dd6hb6.
Brenner H, Hoffmeister M, Arndt V, Haug U. Gender differences in colorectal cancer: implications for age at initiation of screening. Br J Cancer. 2007;96(5):828-31. http://doi.org/cf6xss.
Bujanda L, Cosme A, Gil I, Arenas-Mirave JI. Malignant colorectal polips. World J Gastroenterol. 2010;16(25):3103-11. http://doi.org/cbf6pk.
Burnett-Hartman AN, Newcomb PA, Phipps AI, Passarelli MN, Grady WM, Upton MP, et al. Colorectal endoscopy, advanced adenomas, and sessile serrated polyps: implications for proximal colon cancer. Am J Gastroenterol. 2012;107(8):1213-9. http://doi.org/f39hc8.
Markowitz SD, Bertagnolli MM. Molecular origins of cancer: Molecular basis of colorectal cancer. N Engl J Med. 2009;361(25):2449-60. http://doi.org/cr398j.
de la Peña J, Diaz A, Moraleja I. Indicaciones de la colonoscopia, rectoscopia y anuscopia. Medicine. 2012;11(7):451-4. http://doi.org/f27qb4.
Waye J. Lower gastrointestinal endoscopy and biopsy. In: Hawkey CJ, Bosch J, Richter JE, García-Tsa G, Chan FKL, editors. Textbook of Clinical Gastroenterology and hepatology. 2nd edition. Oxford: Wiley-Blackwell; 2012. p. 936-942.
The Paris endoscopic classification of superficial neoplastic lesions: esophagus, stomach, and colon: November 30 to December 1, 2002. Gastrointest Endosc. 2003;58(Supple 6):S3-43. http://doi.org/d3wr28.
Li M, Ali SM, Umm-a-OmarahGilani S, Liu J, Li YQ, Zuo XL. Kudo’s pit pattern classification for colorectal neoplasms: A meta-analysis. World J Gastroenterol. 2014;20(35):12649-56. http://doi.org/f6gznk.
Lagares-Garcia JA, Kurek S, Collier B, Diaz F, Schilli R, Richey J, et al. Colonoscopy in octogenarians and older patients. Surg Endosc. 2001;15(3):262-5. http://doi.org/frd49r.
Cardona-Villamizar HJ, Otero-Regino W, Forero-Piñeros EA, Gutierrez-Ceballos O. Significado de los pólipos en colon distal, en una población de un país en vía de desarrollo: prevalencia y asociación con neoplasia proximal sincrónica. Rev Colomb Gastroenterol. 2004;19(4):253-62.
Overholt BF, Brooks-Belli L, Grace MG, Rankin K, Harrell R, Turyk M, et al. Evaluating Screening Age for Colonoscopy: A Quality Assurance Assessment. J Clin Gastroenterol. 2010;44(7):e147-53. http://doi.org/bszrgz.
Centers for Disease Control and Prevention (CDC). Vital Signs: Colorectal Cancer Screening Among Adults Aged 50-75 Years. United States, 2008. MMWR. 2010;59(26);808-12.
Hassan C, Repici A, Zullo A, Sharma P. New Paradigms for Colonoscopic Management of Diminutive Colorectal Polyps: Predict, Resect, and Discard or Do Not Resect? Clin Endosc. 2013;46(2):130-7. http://doi.org/f4txcg.
Lin OS. Performing colonoscopy in elderly and very elderly patients: Risks, costs and benefits. World J Gastrointest Endosc. 2014;16(6):220-6. http://doi.org/b6qv.
Asociación Médica Mundial. Declaración de Helsinki de la Asociación Médica Mundial. Principios éticos para las investigaciones médicas en seres humanos. Fortaleza: 64a Asamblea General de la AMM; 2013 [cited 2014 Dec 20]. Available from: https://goo.gl/hvf7l1.
Colombia. Ministerio de Salud. Resolución 8430 de 1993 (octubre 4): Por la cual se establecen las normas científicas, técnicas y administrativas para la investigación en salud. Bogotá D.C.; octubre 4 de 1993.
Silva SM, Rosa VF, Santos AC, RM, Oliveira PG, Susa JB. Influence of patients age and colorectal polips size on histopatholgy findings. Arq Bras Cir Dig. 2014;27(2):109-13. http://doi.org/b6pp.
López-Köstner F, Kronber U, Zárate AJ, Wielandt AM, Pinto E, Suazo C, et al. Programa de detección de neoplasias colorrectales en población mayor de 50 años. Rev Med Chil. 2012;140(3):281-6. http://doi.org/b6qw.
Ko HJ, Youn CH. Determination of the beginning age for colonoscopic screening among colonoscopy-naïve individuals. Clin Res Hepatol Gastroenterol. 2012;36(4):384-90. http://doi.org/f4bw6h.
Bafandeh Y, Khoshbaten M, Eftekhar Sadat AT, Farhang S. Clinical predictors of colorectal polyps and carcinoma in a low prevalence region: Results of a colonoscopy based study. World J Gastroenterol. 2008;14(10):1534-8.
Zare-Mirzaie A, Abolhasani M, Aryamanesh A. Left sided colorectal adenomatous polyps have more risk for high grade dysplasia. Acta Med Iran. 2013;51(3):172-7.
Rundle AG, Lebwohl B, Vogel R, Levine S, Neugut AI. Colonoscopic screening in average -isk individual ages 40 to 49 vs 50 to 59 years. Gastroenterology. 2008;134(5):1311-5. http://doi.org/dq6mkk.
Iravani S, Kashfi SM, Azimzadeh P, Lashkari MH. Prevalence and characteristics of colorectal polyps in symptomatic and asymptomatic Iranian patients undergoing colonoscopy from 2009-2013. Asian Pac J Cancer Prev. 2014;15(22):9933-7. http://doi.org/b6qx.
Giuliani A, Caporale A, Corona M, Ricciardulli T, Di Bari M, Demoro M, et al. Large size, villous content and distal location are associated with severe dysplasia in colorectal adenomas. Anticancer Res. 2006;26(5B):3717-22.
Eshghi MJ, Fatemi R, Hashemy A, Aldulaimi D, Khodadoostan M. A retrospective study of patients with colorectal polyps. Gastroenterol Hepatol Bed Bench. 2011;4(1):17-22.
Morimoto LM, Newcomb PA, Ulrich CM, Bostick RM, Lais CJ, Potter JD. Risk factors for hyperplastic and adenomatous polyps: evidence for malignant potential? Cancer Epidemiol Biomarkers Prev. 2002;11(10 Pt 1):1012-8.
Castells A, Bessa X, Quintero E, Bujanda L, Cubiella J, Salas D, et al. Risk of advanced proximal neoplasms according to distal colorectal findings: comparison of sigmoidoscopy-based strategies. J Natl Cancer Inst. 2013;105(12):878-86. http://doi.org/f43c9p.
Terhaar Sive Droste JS, Craanen ME, van der Hulst RWM, Bartelsman JF, Bezemer DP, Cappendijk KR, et al. Colonoscopic yield of colorectal neoplasia in dailyclinical practice. World J Gastroenterol. 2009;15(9):1085-92. http://doi.org/d8dtrk.
Segnan N, Armaroli P, Bonelli L, Risio M, Scioallero S, Zappa M, et al. Once-Only Sigmoidoscopy in Colorectal Cancer Screening: Follow-up Findings of the Italian Randomized Controlled Trial—SCORE. J Natl Cancer. 2011;103(17):1310-22. http://doi.org/cz9ddx.
Wang FW, Hsu PI, Chuang HY, Tu MS, Mar GY, King TM, et al. Prevalence and risk factors of asymptomatic colorectal polyps in taiwan. Gastroenterol Res Pract. 2014;2014:985205. http://doi.org/f58gkv.
Binda V, Pereira-Lima J, Nunes CA, Falkemberg LT, Azambuja DB, Cruz JV. Is there a role for sigmoidoscopy in symptomatic patients? Analysis of a study correlating distal and proximal colonic neoplasias detected by colonoscopy in a symptomatic population. Arg Gastroenterol. 2007;4(1):2-7. http://doi.org/b97t4w.
Marderstein EL, Church JM. Classic “outlet” rectal bleeding does not require full colonoscopy to exclude significant pathology. Dis Colon Rectum. 2008;51(2):202-6. http://doi.org/b9pmqn.
Cómo citar
APA
ACM
ACS
ABNT
Chicago
Harvard
IEEE
MLA
Turabian
Vancouver
Descargar cita
Licencia
Derechos de autor 2017 Revista de la Facultad de Medicina

Esta obra está bajo una licencia Creative Commons Reconocimiento 3.0 Unported.
-