Alcohol consumption in Spanish mental health patients vs. working population
Consumo de alcohol en España en pacientes de unidades de salud mental versus trabajadores en general
DOI:
https://doi.org/10.15446/revfacmed.v66n2.63324Palabras clave:
Alcoholism, Public Health, Occupational Health, Mental Health (en)Alcohol, Salud pública, Salud laboral, Salud mental (es)
Descargas
Introduction: Alcohol consumption has a high prevalence in society and its chronic consumption is one of the main factors related to health condition in an individual, along with other aspects concerning lifestyle. Regarding the health-disease correlation, it is one of the main determinants of health, from an epidemiological point of view, and has been a traditional object of study from different perspectives and in diverse population groups.
Objective: To compare consumption patterns and related variables in two different groups: patients in mental health units and workers in general.
Materials and methods: Cross-sectional study in a population of 1 180 service workers and 304 patients in a mental health unit. Sociodemographic and work aspects, as well as pattern of alcohol consumption were analyzed for both populations.
Results: Differences in both groups were observed regarding the number of consumers, quantity of consumption and type of beverages consumed, differences that disappear, in part, when comparing groups of workers of both population samples.
Conclusions: Differences in the consumption pattern of both populations lead to different preventive-assistance strategies and to the need for implementing coordinated actions by specific programs among those affected.
Introducción. El consumo de alcohol tiene una elevada prevalencia en la sociedad y su consumo crónico es uno de los principales factores relacionados con el estado de salud de los individuos, junto a otros aspectos concernientes al estilo de vida. Debido a su importancia, este tema ha sido objeto tradicional de estudio desde diferentes perspectivas epidemiológicas y en diversos colectivos poblacionales.
Objetivo. Realizar una comparativa de patrones de consumo y variables relacionadas en dos colectivos diferenciados: pacientes de unidades de salud mental y trabajadores en general.
Materiales y métodos. Estudio transversal realizado en una población de 1 180 trabajadores del sector servicios de la administración pública y 304 pacientes de una unidad de salud mental. Se analizaron variables sociodemográficas y laborales y el patrón de consumo de alcohol.
Resultados. Existen diferencias en ambos colectivos en cuanto al número de consumidores, cantidad de consumo y tipo de bebidas consumidas, diferencias que desaparecen en parte cuando se comparan colectivos de trabajadores de ambas muestras poblacionales.
Conclusiones. Las diferencias en el patrón de consumo de ambas poblaciones orientan hacia actuaciones preventivo-asistenciales distintas en ambos grupos y hacia una necesidad de implementar actuaciones coordinadas entre todos los afectados mediante programas específicos.
original research
DOI: https://doi.org/10.15446/revfacmed.v66n2.63324
Alcohol consumption in Spanish mental health patients vs. working population
Consumo de alcohol en España en pacientes de unidades de salud mental versus trabajadores en general
Received: 14/03/2017. Accepted: 23/05/2017.
Miguel Ruiz-Flores Bistuer1 • María Teófila Vicente-Herrero2 • Silvia Lladosa-Marco3 • Luisa Mercedes Capdevila-García4
Ángel Arturo López-González5
1 IBSALUT - Mental Health Unit - Ibiza - Spain.
2 Grupo Correos - Occupational Medicine Service - Valencia - Spain.
3 Universidad de Valencia - Faculty of Mathematical Sciences - Department of Statistics and Operations Research - Valencia - Spain.
4 MAPFRE - Prevention service - Valencia - Spain.
5 IBSALUT - Occupational Medicine Service - Palma de Mallorca - Spain.
Corresponding author: María Teofila Vicente-Herrero. Occupational Medicine Service, Grupo Correos. Plaza del ayuntamiento 24-2. Telephone number: +34 96 606334666. Valencia. España. Email: mtvh@ono.com/correoteo@gmail.com.
| Abstract |
Introduction: Alcohol consumption has a high prevalence in society and its chronic consumption is one of the main factors related to health condition in an individual, along with other aspects concerning lifestyle. Regarding the health-disease correlation, it is one of the main determinants of health, from an epidemiological point of view, and has been a traditional object of study from different perspectives and in diverse population groups.
Objective: To compare consumption patterns and related variables in two different groups: patients in mental health units and workers in general.
Materials and methods: Cross-sectional study in a population of 1 180 service workers and 304 patients in a mental health unit. Sociodemographic and work aspects, as well as pattern of alcohol consumption were analyzed for both populations.
Results: Differences in both groups were observed regarding the number of consumers, quantity of consumption and type of beverages consumed, differences that disappear, in part, when comparing groups of workers of both population samples.
Conclusions: Differences in the consumption pattern of both populations lead to different preventive-assistance strategies and to the need for implementing coordinated actions by specific programs among those affected.
Keywords: Alcoholism; Public Health; Occupational Health; Mental Health (MeSH).
Ruiz-Flores Bistuer M, Vicente-Herrero MT, Lladosa-Marco S, Capdevila-García LM, López-González AA. Alcohol consumption in Spanish mental health patients vs. working population. Rev. Fac. Med. 2018;66(2):171-7. English. doi: https://doi.org/10.15446/revfacmed.v66n2.63324.
| Resumen |
Introducción. El consumo de alcohol tiene una elevada prevalencia en la sociedad y su consumo crónico es uno de los principales factores relacionados con el estado de salud de los individuos, junto a otros aspectos concernientes al estilo de vida. Debido a su importancia, este tema ha sido objeto tradicional de estudio desde diferentes perspectivas epidemiológicas y en diversos colectivos poblacionales.
Objetivo. Realizar una comparativa de patrones de consumo y variables relacionadas en dos colectivos diferenciados: pacientes de unidades de salud mental y trabajadores en general.
Materiales y métodos. Estudio transversal realizado en una población de 1 180 trabajadores del sector servicios de la administración pública y 304 pacientes de una unidad de salud mental. Se analizaron variables sociodemográficas y laborales y el patrón de consumo de alcohol.
Resultados. Existen diferencias en ambos colectivos en cuanto al número de consumidores, cantidad de consumo y tipo de bebidas consumidas, diferencias que desaparecen en parte cuando se comparan colectivos de trabajadores de ambas muestras poblacionales.
Conclusiones. Las diferencias en el patrón de consumo de ambas poblaciones orientan hacia actuaciones preventivo-asistenciales distintas en ambos grupos y hacia una necesidad de implementar actuaciones coordinadas entre todos los afectados mediante programas específicos.
Palabras clave: Alcohol; Salud pública; Salud laboral; Salud mental (DeCS).
Ruiz-Flores Bistuer M, Vicente-Herrero MT, Lladosa-Marco S, Capdevila-García LM, López-González AA. [Consumo de alcohol en España en pacientes de unidades de salud mental versus trabajadores en general]. Rev. Fac. Med. 2018;66(2):171-7. English. doi: https://doi.org/10.15446/revfacmed.v66n2.63324.
Introduction
Alcoholic beverages are highly consumed worldwide. Although most adults have a low risk drinking pattern, there are people who present harmful alcohol consumption patterns, which range from daily heavy drinkers to occasional/social risk consumers. Given the danger they pose to health, these types of patterns create a public health and safety issue in almost all countries, with estimated figures of 3.3 million deaths per year attributable to alcohol consumption. (1) Nearly 5.9% of the deaths recorded in 2014 in the world were related to alcohol consumption (7.6% for men and 4% for women). (2)
Bearing in mind that there are different modes of consumption, different types of beverages and different social and cultural characteristics in each subpopulation, morbidity and mortality may vary greatly, since they do not depend only on the amount of alcohol consumed, which may affect the estimates and the methodology used in various studies. (3) If the International Classification of Diseases ICD-10 codes (4) are taken as a basis, it is possible to see that there are more than 30 codes directly related to alcohol. Furthermore, alcohol is a leading cause of disease in more than 200 of them.
Different consumption patterns give way to very different outcomes in relation to the health condition of different population groups. Therefore, this work aims to define the consumption patterns in two well-differentiated populations: a population of workers in general and a population of patients-users of a mental health unit (MHU), regarding the quantity of measured consumption and the subjective perception of said consumption. Both concepts will be expanded to explain more precisely the impact of alcohol consumption and, in this way, identify harmful consumption patterns as quickly as possible and propose differentiated interventionist strategies. This type of intervention is recommended among psychiatric patients depending on their diagnoses. (5)
Methodology
Cross-sectional observational study in which data were collected from two different groups: workers of public administration companies in the Balearic Islands and the Valencian Community (Spain) and patients of a MHU of the Balearic Islands (Spain). In the workers population, the study was carried out during the application of specific health surveillance surveys by the companies; this procedure was carried out between January and November 2011. Informed consent was obtained from all the people involved, who participated voluntarily. Sampling was randomly obtained and it was brought to the attention of the health and safety committees. Data of MHU patients were collected between February and October 2014 during a clinical interview made by a psychiatrist, without previous selection, with voluntary participation, random sampling and informed consent for subsequent epidemiological use.
Age, sex, educational attainment (elementary, secondary and higher education), type of work (manual and non-manual) and social class (1: high, 2: medium and 3: low) were studied in both groups —as proposed by the working group of the Spanish Society of Epidemiology and the Spanish Society of Family and Community Medicine (6)—, days of consumption per week, drinks consumed and type of alcohol (wine, beer, spirits and various/all, both fermented and distilled beverages). In the case of MHU patients, social and work conditions were established (housewife, unemployed, retired, permanent worker and casual worker).
To quantify consumption, standard drinking units (SDU) were used to measure consumption/day/person. (7) The Spanish Scientific Society for Research on Alcohol, Alcoholism and Other Drug Addictions established that a SDU is equivalent to 10g of pure alcohol. (8) It should be noted that, in countries such as the USA, drinks express their alcohol content in grams of ethanol/100mL of beverage, instead of 1mL of ethanol/100mL of beverage (mL%), a formula used in almost all countries, which lowers figures by 20%. Based on this, three consumption profiles are defined: low risk (<14 SDU/week in women and <21 SDU/week in men), risky (14-20.9 SDU/week in women and 21-34.9 SDU/week in men) and abusive (>21 SDU/week in women and >35 SDU/week in men).
Diagnoses of MHU patients were grouped according to the ICD-10 chapters F00-F09, Organic, including symptomatic, mental disorders; F10-F19, Mental and behavioral disorders due to psychoactive substance use; F20-F29, Schizophrenia, schizotypal and delusional disorders; F30-F39 Mood [affective] disorders; F40-49, Neurotic, stress-related and somatoform disorders; F50-59, Behavioral syndromes associated with physiological disturbances and physical factors; F60-69, Disorders of adult personality and behavior; F70-79, Mental retardation; F80-89, Disorders of psychological development; and F90-98, Behavioral and emotional disorders with onset usually occurring in childhood and adolescence.
Non-drinkers were separated into abstainers and ex-drinkers (those who quit drinking within the past year). To assess the perception of consumption, the validated version of the AUDIT questionnaire was applied (9) and a descriptive analysis was carried out using frequency tables for categorical variables and descriptive statistics (mean, median, quartiles and standard deviation) for quantitative variables. A bivariate analysis was carried out for statistical inference, using the t-Student and Wilcoxon tests for continuous variables, depending on the nature of the variables.
Normality hypotheses were verified using Kolmogorov-Smirnov or Shapiro-Wilk test. In the case of categorical variables, the Chi-square or Fisher test was used depending on whether applicability conditions for the expected values were met or not. Regression models (logistic or linear) were used for multivariate analysis.
Results
The population sample included 1 180 workers and 304 patients from a MHU. The characteristics of both samples are described in Table 1.
Table 1. Characteristics of the sample.
|
Characteristics |
WP (n=1180) |
MHUP (n=304) |
|||
|
Age |
minimum 22; maximum 67; average 46.03 |
minimum 19; maximum 85; average 47.81 |
|||
|
Sex |
Women |
438 |
37.12% |
175 |
57.57% |
|
Men |
742 |
62.88% |
129 |
42.43% |
|
|
Educational attainment |
Elementary |
309 |
26.19% |
179 |
58.88% |
|
Secondary |
729 |
61.78% |
122 |
40.13% |
|
|
Higher |
142 |
12.03% |
3 |
0.99% |
|
|
Type of job |
Manual |
778 |
65.93 |
86 |
28.29% |
|
Not manual |
402 |
34.07 |
40 |
13.16% |
|
|
Unemployed |
0 |
0% |
178 |
58.55% |
|
|
Social class * |
I |
184 |
15.59 |
9 |
2.96% |
|
III |
941 |
79.75 |
31 |
10.20% |
|
|
VII |
55 |
4.66 |
86 |
28.29% |
|
WP: working population; MHUP: mental health unit patients.
* Class I: directors/managers, university professionals, athletes and artists; class II: intermediate occupations, self-employed workers, unemployed individuals; Class III: unskilled workers.
Source: Own elaboration based on the data obtained in the study.
Considering the classification described above, according to the National Occupational Classification 2011 (NOC-11), differences were found in both populations regarding the characteristics of alcohol consumption. It is worth noting that the working population consumes alcohol by 81.19%, with a weekend consumption pattern, and mainly wine and beer, while 57.24% of MHU patients report not consuming alcohol in the past year (Table 2).
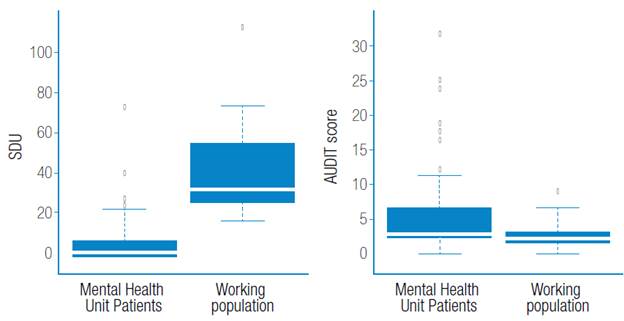
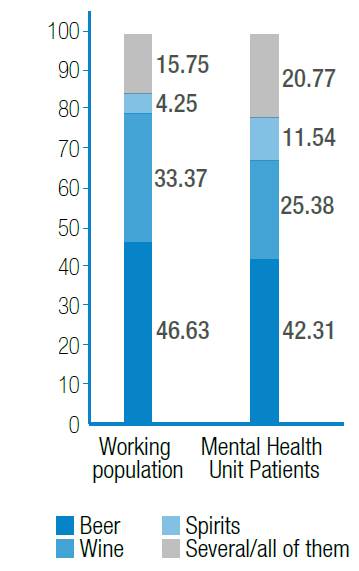
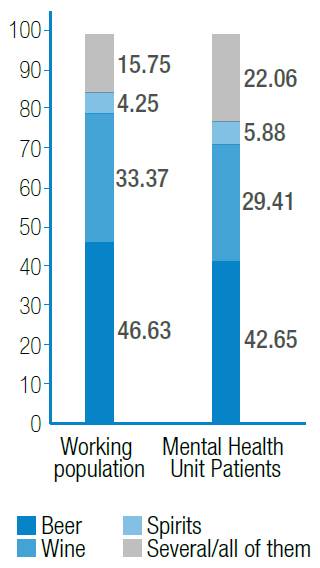
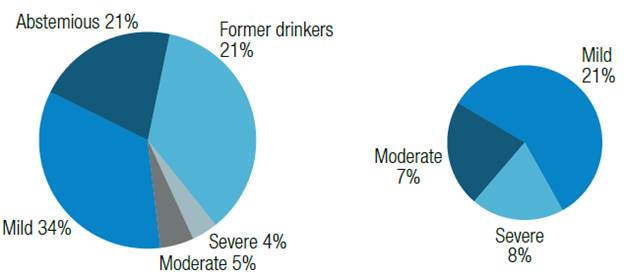
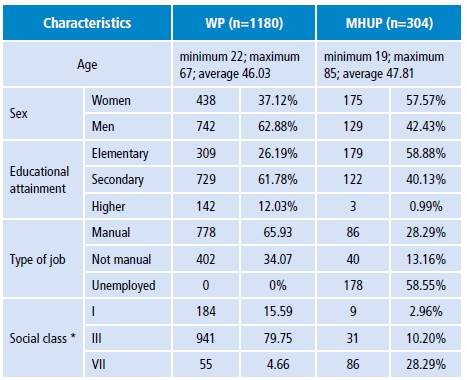
Furthermore, a striking discrepancy was observed regarding the subjective perception of alcohol consumption, since MHU patients, despite having a lower quantified alcohol consumption in comparison to the working population, have a greater consumption perception, in other words, they are more aware and accurate when it comes to assessing alcohol consumption (Figure 1). Moreover, differences were found in relation to the type of beverage consumed in both population groups (Figure 2).
Table 2. Levels of consumption among the population.
|
Variable |
WP |
MHUP |
||||
|
n |
% |
n |
% |
|||
|
Frequency |
Never |
215 |
18.22% |
174 |
57.24% |
|
|
Monthly |
164 |
14.40% |
43 |
14.14% |
||
|
Weekly |
4 |
0.34% |
17 |
5.59% |
||
|
Weekends |
472 |
40.00% |
17 |
5.59% |
||
|
3 days/week |
29 |
2.46% |
7 |
2.30% |
||
|
Every day |
298 |
25.25% |
46 |
15.13% |
||
|
Number of drinks/day |
0 |
215 |
18.22% |
174 |
57.24% |
|
|
1 |
280 |
23.73% |
59 |
19.41% |
||
|
2 |
599 |
18.22% |
34 |
11.18% |
||
|
3 |
70 |
5.93% |
16 |
5.26% |
||
|
>3 |
16 |
23.73% |
21 |
6.91% |
||
|
Type of alcohol |
Beer |
450 |
38.14% |
55 |
18.09% |
|
|
Wine |
322 |
27.29% |
33 |
10.86% |
||
|
Spirits |
41 |
3.47% |
15 |
4.93% |
||
|
Several/all of them |
152 |
12.88% |
27 |
8.88% |
||
|
None |
215 |
18.22% |
174 |
57.24% |
||
|
SDU score |
Low risk |
97 |
10,05% |
104 |
80% |
|
|
Risky consumption |
349 |
36.17% |
15 |
11.54% |
||
|
Abusive consumption |
519 |
53.78% |
11 |
8.46% |
||
WP: working population; MHUP: mental health unit patients; SDU: standard drinking units.
Source: Own elaboration based on the data obtained in the study.
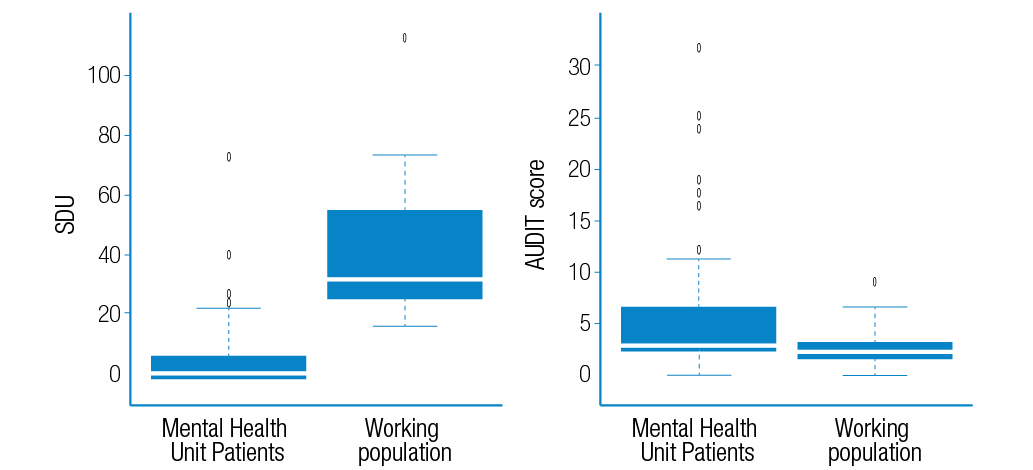
Figure 1. Quantified consumption (SDU) versus perceived consumption (AUDIT) in both populations.
Source: Own elaboration based on the data obtained in the study.
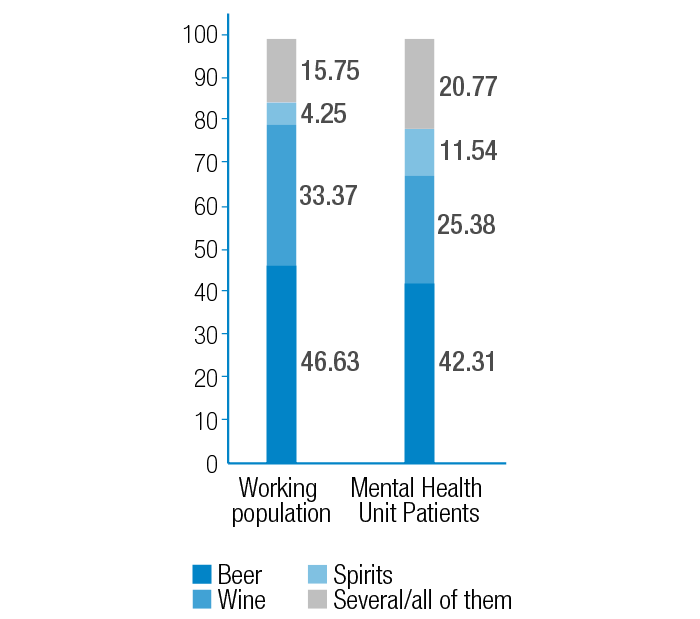
Figure 2. Comparison of type of alcohol consumed in both populations.
Source: Own elaboration based on the data obtained in the study.
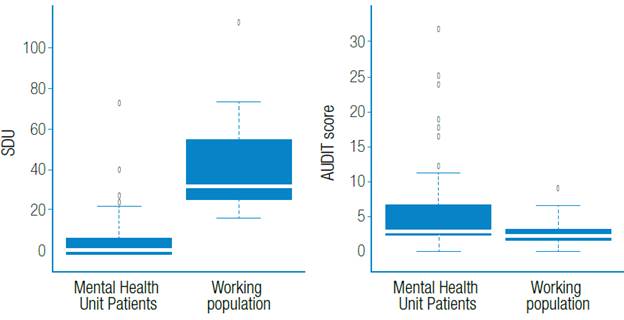
The differences were modified when the workers of both samples were compared selectively by types of beverage consumed (Figure 3).
However, differences in consumption perception between both populations studied remained (Figure 4).

Figure 3. Comparison of workers of both populations. Quantified consumption (SDU) vs. Perceived Consumption (AUDIT).
Source: Own elaboration based on the data obtained in the study.
The comparison of current MHU consumers and the status of former drinkers before the study can be seen in Figure 5.
Discussion
The main objective of this study is to compare alcohol consumption and the perception of consumption in two well-differentiated groups of the Spanish population: working population in general and MHU patients. It is based on the hypothesis that there are qualitative and quantitative differences between them that are related to their personal, cultural, social and work conditions —in the case of those who are part of the work force. (10)
The findings of this research show high alcohol consumption among workers, which coincides with other previous investigations with different study groups; in consequence, higher consumption figures are obtained in the hotel or construction industry, than those obtained here. (11) Aspects assessed as occasional do not coincide either, since other studies consider aspects related to work stress or work shifts —which were not assessed in this research— as predisposing factors for greater consumption. (12)
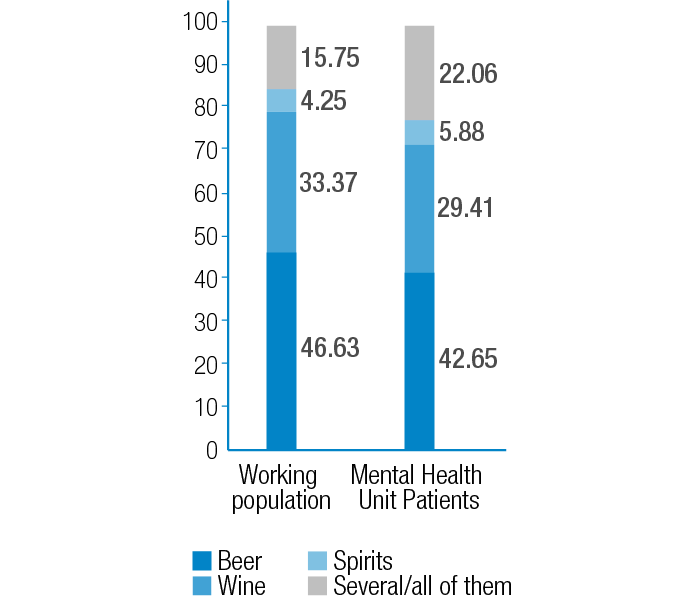
Figure 4. Comparison of type of alcohol consumed by the workers of both populations.
Source: Own elaboration based on the data obtained in the study.

Figure 5. Comparison of consumption in former drinkers at the mental health unit: quantified consumption (SDU) versus perceived consumption (AUDIT) in workers of both populations.
Source: Own elaboration based on the data obtained in the study.
Low consumption perception observed in the workers group had already been pointed out by other authors, who were oriented towards educational interventions to support prevention. (13) Regarding the type of beverage consumed as a priority in both groups (wine and beer), there are coincidences with other researches, both in men and women (14), although Finnish authors highlight greater consumption of wine and beer among men and other types of liqueurs in women. (15)
Furthermore, the so-called blue collar worker is another common point in relation to greater consumption among manual workers of both groups, which coincides with other works; this may be caused by greater permissiveness and lack of skills on the part of supervisors regarding the management of abusive consumption and to the lower work risks increased by consumption. Additionally, it is pointed out that the greater the isolation of these workers, the greater the consumption of alcohol. (16)
Knowing about consumption perception favors more effective preventive actions on predictive factors. (17) In MHU patients, there was a significant ratio of non-consumers at the time of the interview (regarding consumption in the past year). However, among alcohol consumers, high levels of consumption —above the working population in general— were detected, at the expense of high-alcohol-content beverages, although beer and wine are the most common.
The correlation with greater vulnerability to alcohol consumption in psychiatric patients had already been evidenced in previous studies and had been oriented towards coordinated actions between psychiatrists and addictologist to achieve better results. (18) However, proper consumption perception among MHU patients contrasts with the low perception among workers in general.
After inquiring about previous alcohol consumption, it was possible to see that there was a high previous consumption among the patients, being higher in lower educational levels. During the visit paid to the patients, the psychiatrist usually advised them to quit drinking, which would explain the high percentage of former drinkers. It must be taken into account that the association of both pathologies hinders the prognosis in the psychiatric process that motivates consultation and delays recovery. (19) In fact, the psychiatric pathology itself can lead to a relapse in alcohol consumption or in other types of addictions, so the psychiatric interview should consider these aspects altogether based on structured clinical interviews. (20)
Among working population in general, consumption levels are lower, but the perception of consumption is also lower, which may hinder the effectiveness of intervention programs in this group as it is considered a falsely healthy population and include alcohol consumption in their daily life habits.
The perception of alcohol consumption is relevant to establish prevention programs and avoid side effects and even associated deaths. Most alcohol users are unaware of health service programs or social services and, in most cases, interventions are linked to the mediation of legal services. Better management for early detection and assessment of problems associated to consumption is necessary in the light of guidelines based on evidence. (21) American authors advocate interventions from primary health services and from public health in high-risk consumers, where intervention strategies are implemented and incorporated as a routine in primary care and preventive medicine. (22-24)
The differences observed regarding consumption in relation to social class support the hypotheses of other works that seek to initiate combined actions to reduce alcohol consumption, in which additional measures are included to facilitate reaching all social groups. (25)
Differences found in this work, in terms of alcohol consumption based on social status, had already been exposed in other studies. However, in order to understand better the mechanisms and pathways that influence the differential risk among people in low and high socioeconomic statuses, all authors suggest the need for more research to characterize better the correlation between alcohol consumption, socioeconomic status and risk of disease attributable to alcohol. (26)
One of the strengths of this work is the comparison made between quantified and perceived alcohol consumption and the conditioning factors studied. Also, the comparison between two distinctly different population groups and the scores of a “healthy” population versus a group of “patients” is highlighted.
On the other hand, individual information provided by the worker or by the MHU patient is a limitation as a reference for consumption, since it may be subjective and may lead to bias of the results. Additionally, the impossibility of extrapolating the results to the working population in general is also considered a limitation since all participants are subject of the same work sector.
Conclusions
Knowledge on alcohol consumption, as well as on the subject’s perception of how much they consume and the variables that influence said consumption provide basic information to design preventive strategies and more effective interventions. Future research should include other groups and aspects not covered in this work in order to modulate the results obtained here.
Conflicts of interests
None stated by the authors.
Funding
None stated by the authors.
Acknowledgements
None stated by the authors.
References
1.World Health Organization. Global status report on alcohol and health-2014. Geneva: WHO; 2014 [cited 2015 Sep 1]. Available from: https://goo.gl/EXK8Et.
2.World Health Organization. Alcohol. Nueva York: Nota descriptiva No. 349; 2015 [cited 2017 Sep 19]. Available from: https://goo.gl/aXwhgA.
3.Courtney KE, Polich J. Binge drinking in Young adults: Data, definitions, and determinants. Psychol Bull. 2009;135(1):142-56. http://doi.org/fghvmv.
4.World Health Organization. CIE-10: Trastornos mentales y del comportamiento: descripciones clínicas y pautas para el diagnóstico. Madrid: Meditor; 1992.
5.Bradizza CM, Stasiewicz PR, Paas ND. Relapse to alcohol and drug use among individuals diagnosed with co-occurring mental health and substance use disorders: a review. Clin Psychol Rev. 2006;26(2):162-78. http://doi.org/cmhxt6.
6.Domingo-Salvany A, Regidor E, Alonso J, Alvarez-Dardet C, Borrell C, Doz, F, et al. Una propuesta de medida de la clase social.. Aten Primaria. 2000;25(5):350-63.
7.Edwards G, Marshall EJ, Cook CCH. The treatment of drinking problems: A guide for the helping professions. New York: Cambridge University Press; 2003.
8.Rodríguez-Martos Dauer A, Gual Solé A, Llopis Llácer JJ. La “unidad de bebida estándar” como registro simplificado del consumo de bebidas alcohólicas y su determinación en España. Med Clín. 1999;112(12):446-50.
9.Gual A, Segura L, Contel M, Heather N, Colom J. Audit-3 and audit-4: effectiveness of two short forms of the alcohol use disorders identification test. Alcohol Alcohol. 2002;37(6):591-6.
10.Ruiz-Flores Bistuer M. Consumo de alcohol en población general trabajadora versus pacientes de unidad de salud mental [tesis doctoral]. Ibiza: Universidad de las Islas Baleares; 2016.
11.Benavides FG, Ruiz-Forès N, Delclós J, Domingo-Salvany A. Consumo de alcohol y otras drogas en el medio laboral en España. Gac Sanit. 2013;27(3):248-53. http://doi.org/f2fpn3.
12.Morikawa Y, Sakurai M, Nakamura K, Nagasawa SY, Ishizaki M, Kido T, et al. Correlation between shift-work-related sleep problems and heavy drinking in Japanese male factory workers. Alcohol Alcohol. 2013;48(2):202-6. http://doi.org/f4mcs6.
13.Sprague DJ, Vinson DC. Patient perceptions of risky drinking: knowledge of daily and weekly low-risk guidelines and standard drink sizes. Subst Abus. 2015;38(3):253-6. http://doi.org/cjfp.
14.Halonen JI, Kivimäki M, Pentti J, Virtanen M, Subramanian SV, Kawachi I, et al. Association of the Availability of Beer, Wine, and Liquor Outlets with Beverage-Specific Alcohol Consumption: A Cohort Study. Alcohol Clin Exp Res. 2014;38(4):1086-93. http://doi.org/cjfq.
15.Kerr WC, Greenfield TK, Bond J, Ye Y, Rehm J. Age, period and cohort influences on beer, wine and spirits consumption trends in the US National Alcohol Surveys. Addiction. 2004;99(9):1111-20. http://doi.org/bmk5h4.
16.Biron M, Bamberger PA, Noyman T. Work-related risk factors and employee substance use: insights from a sample of Israeli blue-collar workers. J Occup Health Psychol. 2011;16(2):247-63. http://doi.org/fr2gjb.
17.Hwang WJ, Hong O, Kim MJ. Factors associated with blue-collar workers’ risk perception of cardiovascular disease. J Korean Acad Nurs. 2012;42(7):1095-104. http://doi.org/cjfr.
18.Lang JP, Bonnewitz ML, Kusterer M, Lalanne-Tongio L. Usage d’alcool chez les patients souffrant de troubles psychiatriques : quelles évaluations? Quelle prise en soin? Encephale. 2014;40(4):301-7. http://doi.org/cjfs.
19.Alves H, Kessler F, Ratto LR. Comorbidity: alcohol use and other psychiatric disorders. Rev Bras Psiquiatt. 2004;26(Suppl 1):51-3. http://doi.org/bq5wk6.
20.Gonzalez VM, Bradizza CM, Vincent PC, Stasiewicz PR, Paas ND. Do individuals with a severe mental illness experience greater alcohol and drug-related problems? A test of the supersensitivity hypothesis. Addict Behav. 2007;32(3):477-90 http://doi.org/bww5hz.
21.Morris M, Johnson D, Morrison DS. Opportunities for prevention of alcohol-related death in primary care: results from a population-based cross-sectional study. Alcohol. 2012;46(7):703-7. http://doi.org/f37rmg.
22.Whitlock EP, Polen MR, Green CA, Orleans T, Klein J. Behavioral counseling interventions in primary care to reduce risky/harmful alcohol use by adults: a summary of the evidence for the US Preventive Services Task Force. Ann Intern Med. 2004;140(7):557-68. http://doi.org/cjft.
23.Carter MA. Review: brief multicontact behavioural counselling interventions in primary care reduce risky or harmful alcohol use. Evid Based Nurs. 2004;7(4):108. http://doi.org/cm988p.
24.US Preventive Services Task Force. Screening and counseling to reduce alcohol misuse: recommendations from the United States Preventive Services Task Force. Ann Intern Med. 2004;140(7):1-64. http://doi.org/cjfv.
25.Romelsjö A, Diderichsen F. Changes in alcohol-related inpatient care in Stockholm County in relation to socioeconomic status during a period of decline in alcohol consumption. Am J Public Health. 1989;79(1):52-6.
26.Jones L, Bates G, McCoy E, Bellis MA. Relationship between alcohol-attributable disease and socioeconomic status, and the role of alcohol consumption in this relationship: a systematic review and meta-analysis. BMC Public Health. 2015;15:400. http://doi.org/4d6.

Jean Marc Bourgery
“Traité complet de l’anatomie de l’homme”
Paris 1832-1854
Recibido: 14 de marzo de 2017; Aceptado: 23 de mayo de 2017
Abstract
Introduction:
Alcohol consumption has a high prevalence in society and its chronic consumption is one of the main factors related to health condition in an individual, along with other aspects concerning lifestyle. Regarding the health-disease correlation, it is one of the main determinants of health, from an epidemiological point of view, and has been a traditional object of study from different perspectives and in diverse population groups.
Objective:
To compare consumption patterns and related variables in two different groups: patients in mental health units and workers in general.
Materials and methods:
Cross-sectional study in a population of 1 180 service workers and 304 patients in a mental health unit. Sociodemographic and work aspects, as well as pattern of alcohol consumption were analyzed for both populations.
Results:
Differences in both groups were observed regarding the number of consumers, quantity of consumption and type of beverages consumed, differences that disappear, in part, when comparing groups of workers of both population samples.
Conclusions:
Differences in the consumption pattern of both populations lead to different preventive-assistance strategies and to the need for implementing coordinated actions by specific programs among those affected.
Keywords:
Alcoholism, Public Health, Occupational Health, Mental Health (MeSH).Resumen
Introducción.
El consumo de alcohol tiene una elevada prevalencia en la sociedad y su consumo crónico es uno de los principales factores relacionados con el estado de salud de los individuos, junto a otros aspectos concernientes al estilo de vida. Debido a su importancia, este tema ha sido objeto tradicional de estudio desde diferentes perspectivas epidemiológicas y en diversos colectivos poblacionales.
Objetivo.
Realizar una comparativa de patrones de consumo y variables relacionadas en dos colectivos diferenciados: pacientes de unidades de salud mental y trabajadores en general.
Materiales y métodos.
Estudio transversal realizado en una población de 1 180 trabajadores del sector servicios de la administración pública y 304 pacientes de una unidad de salud mental. Se analizaron variables sociodemográficas y laborales y el patrón de consumo de alcohol.
Resultados.
Existen diferencias en ambos colectivos en cuanto al número de consumidores, cantidad de consumo y tipo de bebidas consumidas, diferencias que desaparecen en parte cuando se comparan colectivos de trabajadores de ambas muestras poblacionales.
Conclusiones.
Las diferencias en el patrón de consumo de ambas poblaciones orientan hacia actuaciones preventivo-asistenciales distintas en ambos grupos y hacia una necesidad de implementar actuaciones coordinadas entre todos los afectados mediante programas específicos.
Palabras clave:
Alcohol, Salud pública, Salud laboral, Salud mental (DeCS).Introduction
Alcoholic beverages are highly consumed worldwide. Although most adults have a low risk drinking pattern, there are people who present harmful alcohol consumption patterns, which range from daily heavy drinkers to occasional/social risk consumers. Given the danger they pose to health, these types of patterns create a public health and safety issue in almost all countries, with estimated figures of 3.3 million deaths per year attributable to alcohol consumption. 1 Nearly 5.9% of the deaths recorded in 2014 in the world were related to alcohol consumption (7.6% for men and 4% for women). 2
Bearing in mind that there are different modes of consumption, different types of beverages and different social and cultural characteristics in each subpopulation, morbidity and mortality may vary greatly, since they do not depend only on the amount of alcohol consumed, which may affect the estimates and the methodology used in various studies. 3 If the International Classification of Diseases ICD-10 codes 4 are taken as a basis, it is possible to see that there are more than 30 codes directly related to alcohol. Furthermore, alcohol is a leading cause of disease in more than 200 of them.
Different consumption patterns give way to very different outcomes in relation to the health condition of different population groups. Therefore, this work aims to define the consumption patterns in two well-differentiated populations: a population of workers in general and a population of patients-users of a mental health unit (MHU), regarding the quantity of measured consumption and the subjective perception of said consumption. Both concepts will be expanded to explain more precisely the impact of alcohol consumption and, in this way, identify harmful consumption patterns as quickly as possible and propose differentiated interventionist strategies. This type of intervention is recommended among psychiatric patients depending on their diagnoses. 5
Methodology
Cross-sectional observational study in which data were collected from two different groups: workers of public administration companies in the Balearic Islands and the Valencian Community (Spain) and patients of a MHU of the Balearic Islands (Spain). In the workers population, the study was carried out during the application of specific health surveillance surveys by the companies; this procedure was carried out between January and November 2011. Informed consent was obtained from all the people involved, who participated voluntarily. Sampling was randomly obtained and it was brought to the attention of the health and safety committees. Data of MHU patients were collected between February and October 2014 during a clinical interview made by a psychiatrist, without previous selection, with voluntary participation, random sampling and informed consent for subsequent epidemiological use.
Age, sex, educational attainment (elementary, secondary and higher education), type of work (manual and non-manual) and social class (1: high, 2: medium and 3: low) were studied in both groups -as proposed by the working group of the Spanish Society of Epidemiology and the Spanish Society of Family and Community Medicine 6-, days of consumption per week, drinks consumed and type of alcohol (wine, beer, spirits and various/all, both fermented and distilled beverages). In the case of MHU patients, social and work conditions were established (housewife, unemployed, retired, permanent worker and casual worker).
To quantify consumption, standard drinking units (SDU) were used to measure consumption/day/person. 7 The Spanish Scientific Society for Research on Alcohol, Alcoholism and Other Drug Addictions established that a SDU is equivalent to 10g of pure alcohol. 8 It should be noted that, in countries such as the USA, drinks express their alcohol content in grams of ethanol/100mL of beverage, instead of 1mL of ethanol/100mL of beverage (mL%), a formula used in almost all countries, which lowers figures by 20%. Based on this, three consumption profiles are defined: low risk (<14 SDU/week in women and <21 SDU/week in men), risky (14-20.9 SDU/week in women and 21-34.9 SDU/week in men) and abusive (>21 SDU/week in women and >35 SDU/week in men).
Diagnoses of MHU patients were grouped according to the ICD-10 chapters F00-F09, Organic, including symptomatic, mental disorders; F10-F19, Mental and behavioral disorders due to psychoactive substance use; F20-F29, Schizophrenia, schizotypal and delusional disorders; F30-F39 Mood [affective] disorders; F40-49, Neurotic, stress-related and somatoform disorders; F50-59, Behavioral syndromes associated with physiological disturbances and physical factors; F60-69, Disorders of adult personality and behavior; F70-79, Mental retardation; F80-89, Disorders of psychological development; and F90-98, Behavioral and emotional disorders with onset usually occurring in childhood and adolescence.
Non-drinkers were separated into abstainers and ex-drinkers (those who quit drinking within the past year). To assess the perception of consumption, the validated version of the AUDIT questionnaire was applied 9 and a descriptive analysis was carried out using frequency tables for categorical variables and descriptive statistics (mean, median, quartiles and standard deviation) for quantitative variables. A bivariate analysis was carried out for statistical inference, using the t-Student and Wilcoxon tests for continuous variables, depending on the nature of the variables.
Normality hypotheses were verified using Kolmogorov-Smirnov or Shapiro-Wilk test. In the case of categorical variables, the Chi-square or Fisher test was used depending on whether applicability conditions for the expected values were met or not. Regression models (logistic or linear) were used for multivariate analysis.
Results
The population sample included 1 180 workers and 304 patients from a MHU. The characteristics of both samples are described in Table 1.
WP: working population; MHUP: mental health unit patients. * Class I: directors/managers, university professionals, athletes and artists; class II: intermediate occupations, self-employed workers, unemployed individuals; Class III: unskilled workers. Source: Own elaboration based on the data obtained in the study.Table 1: Characteristics of the sample.
Considering the classification described above, according to the National Occupational Classification 2011 (NOC-11), differences were found in both populations regarding the characteristics of alcohol consumption. It is worth noting that the working population consumes alcohol by 81.19%, with a weekend consumption pattern, and mainly wine and beer, while 57.24% of MHU patients report not consuming alcohol in the past year (Table 2).
WP: working population; MHUP: mental health unit patients; SDU: standard drinking units. Source: Own elaboration based on the data obtained in the study.Table 2: Levels of consumption among the population.

Furthermore, a striking discrepancy was observed regarding the subjective perception of alcohol consumption, since MHU patients, despite having a lower quantified alcohol consumption in comparison to the working population, have a greater consumption perception, in other words, they are more aware and accurate when it comes to assessing alcohol consumption (Figure 1). Moreover, differences were found in relation to the type of beverage consumed in both population groups (Figure 2).
Figure 1: Quantified consumption (SDU) versus perceived consumption (AUDIT) in both populations.
Figure 2: Comparison of type of alcohol consumed in both populations.
The differences were modified when the workers of both samples were compared selectively by types of beverage consumed (Figure 3).
Figure 3: Comparison of workers of both populations. Quantified consumption (SDU) vs. Perceived Consumption (AUDIT).
However, differences in consumption perception between both populations studied remained (Figure 4).
Figure 4: Comparison of type of alcohol consumed by the workers of both populations.
The comparison of current MHU consumers and the status of former drinkers before the study can be seen in Figure 5.
Figure 5: Comparison of consumption in former drinkers at the mental health unit: quantified consumption (SDU) versus perceived consumption (AUDIT) in workers of both populations.
Discussion
The main objective of this study is to compare alcohol consumption and the perception of consumption in two well-differentiated groups of the Spanish population: working population in general and MHU patients. It is based on the hypothesis that there are qualitative and quantitative differences between them that are related to their personal, cultural, social and work conditions -in the case of those who are part of the work force. 10
The findings of this research show high alcohol consumption among workers, which coincides with other previous investigations with different study groups; in consequence, higher consumption figures are obtained in the hotel or construction industry, than those obtained here. 11 Aspects assessed as occasional do not coincide either, since other studies consider aspects related to work stress or work shifts -which were not assessed in this research- as predisposing factors for greater consumption. 12
Low consumption perception observed in the workers group had already been pointed out by other authors, who were oriented towards educational interventions to support prevention. 13 Regarding the type of beverage consumed as a priority in both groups (wine and beer), there are coincidences with other researches, both in men and women 14, although Finnish authors highlight greater consumption of wine and beer among men and other types of liqueurs in women. 15
Furthermore, the so-called blue collar worker is another common point in relation to greater consumption among manual workers of both groups, which coincides with other works; this may be caused by greater permissiveness and lack of skills on the part of supervisors regarding the management of abusive consumption and to the lower work risks increased by consumption. Additionally, it is pointed out that the greater the isolation of these workers, the greater the consumption of alcohol. 16
Knowing about consumption perception favors more effective preventive actions on predictive factors. 17 In MHU patients, there was a significant ratio of non-consumers at the time of the interview (regarding consumption in the past year). However, among alcohol consumers, high levels of consumption -above the working population in general- were detected, at the expense of high-alcohol-content beverages, although beer and wine are the most common.
The correlation with greater vulnerability to alcohol consumption in psychiatric patients had already been evidenced in previous studies and had been oriented towards coordinated actions between psychiatrists and addictologist to achieve better results. 18 However, proper consumption perception among MHU patients contrasts with the low perception among workers in general.
After inquiring about previous alcohol consumption, it was possible to see that there was a high previous consumption among the patients, being higher in lower educational levels. During the visit paid to the patients, the psychiatrist usually advised them to quit drinking, which would explain the high percentage of former drinkers. It must be taken into account that the association of both pathologies hinders the prognosis in the psychiatric process that motivates consultation and delays recovery. 19 In fact, the psychiatric pathology itself can lead to a relapse in alcohol consumption or in other types of addictions, so the psychiatric interview should consider these aspects altogether based on structured clinical interviews. 20
Among working population in general, consumption levels are lower, but the perception of consumption is also lower, which may hinder the effectiveness of intervention programs in this group as it is considered a falsely healthy population and include alcohol consumption in their daily life habits.
The perception of alcohol consumption is relevant to establish prevention programs and avoid side effects and even associated deaths. Most alcohol users are unaware of health service programs or social services and, in most cases, interventions are linked to the mediation of legal services. Better management for early detection and assessment of problems associated to consumption is necessary in the light of guidelines based on evidence. 21 American authors advocate interventions from primary health services and from public health in high-risk consumers, where intervention strategies are implemented and incorporated as a routine in primary care and preventive medicine. 22-24
The differences observed regarding consumption in relation to social class support the hypotheses of other works that seek to initiate combined actions to reduce alcohol consumption, in which additional measures are included to facilitate reaching all social groups. 25
Differences found in this work, in terms of alcohol consumption based on social status, had already been exposed in other studies. However, in order to understand better the mechanisms and pathways that influence the differential risk among people in low and high socioeconomic statuses, all authors suggest the need for more research to characterize better the correlation between alcohol consumption, socioeconomic status and risk of disease attributable to alcohol. 26
One of the strengths of this work is the comparison made between quantified and perceived alcohol consumption and the conditioning factors studied. Also, the comparison between two distinctly different population groups and the scores of a "healthy" population versus a group of "patients" is highlighted.
On the other hand, individual information provided by the worker or by the MHU patient is a limitation as a reference for consumption, since it may be subjective and may lead to bias of the results. Additionally, the impossibility of extrapolating the results to the working population in general is also considered a limitation since all participants are subject of the same work sector.
Conclusions
Knowledge on alcohol consumption, as well as on the subject's perception of how much they consume and the variables that influence said consumption provide basic information to design preventive strategies and more effective interventions. Future research should include other groups and aspects not covered in this work in order to modulate the results obtained here.
Acknowledgements
None stated by the authors.
References
Referencias
World Health Organization. Global status report on alcohol and health-2014. Geneva: WHO; 2014 [cited 2015 Sep 1]. Available from: https://goo.gl/EXK8Et.
World Health Organization. Alcohol. Nueva York: Nota descriptiva No. 349; 2015 [cited 2017 Sep 19]. Available from: https://goo.gl/aXwhgA.
Courtney KE, Polich J. Binge drinking in Young adults: Data, definitions, and determinants. Psychol Bull. 2009;135(1):142-56. http://doi.org/fghvmv.
World Health Organization. CIE-10: Trastornos mentales y del comportamiento: descripciones clínicas y pautas para el diagnóstico. Madrid: Meditor; 1992.
Bradizza CM, Stasiewicz PR, Paas ND. Relapse to alcohol and drug use among individuals diagnosed with co-occurring mental health and substance use disorders: a review. Clin Psychol Rev. 2006;26(2):162-78. http://doi.org/cmhxt6.
Domingo-Salvany A, Regidor E, Alonso J, Alvarez-Dardet C, Borrell C, Doz, F, et al. Una propuesta de medida de la clase social.. Aten Primaria. 2000;25(5):350-63.
Edwards G, Marshall EJ, Cook CCH. The treatment of drinking problems: A guide for the helping professions. New York: Cambridge University Press; 2003.
Rodríguez-Martos Dauer A, Gual Solé A, Llopis Llácer JJ. La “unidad de bebida estándar” como registro simplificado del consumo de bebidas alcohólicas y su determinación en España. Med Clín. 1999;112(12):446-50.
Gual A, Segura L, Contel M, Heather N, Colom J. Audit-3 and audit-4: effectiveness of two short forms of the alcohol use disorders identification test. Alcohol Alcohol. 2002;37(6):591-6.
Ruiz-Flores Bistuer M. Consumo de alcohol en población general trabajadora versus pacientes de unidad de salud mental [tesis doctoral]. Ibiza: Universidad de las Islas Baleares; 2016.
Benavides FG, Ruiz-Forès N, Delclós J, Domingo-Salvany A. Consumo de alcohol y otras drogas en el medio laboral en España. Gac Sanit. 2013;27(3):248-53. http://doi.org/f2fpn3.
Morikawa Y, Sakurai M, Nakamura K, Nagasawa SY, Ishizaki M, Kido T, et al. Correlation between shift-work-related sleep problems and heavy drinking in Japanese male factory workers. Alcohol Alcohol. 2013;48(2):202-6. http://doi.org/f4mcs6.
Sprague DJ, Vinson DC. Patient perceptions of risky drinking: knowledge of daily and weekly low-risk guidelines and standard drink sizes. Subst Abus. 2015;38(3):253-6. http://doi.org/cjfp.
Halonen JI, Kivimäki M, Pentti J, Virtanen M, Subramanian SV, Kawachi I, et al. Association of the Availability of Beer, Wine, and Liquor Outlets with Beverage-Specific Alcohol Consumption: A Cohort Study. Alcohol Clin Exp Res. 2014;38(4):1086-93. http://doi.org/cjfq.
Kerr WC, Greenfield TK, Bond J, Ye Y, Rehm J. Age, period and cohort influences on beer, wine and spirits consumption trends in the US National Alcohol Surveys. Addiction. 2004;99(9):1111-20. http://doi.org/bmk5h4.
Biron M, Bamberger PA, Noyman T. Work-related risk factors and employee substance use: insights from a sample of Israeli blue-collar workers. J Occup Health Psychol. 2011;16(2):247-63. http://doi.org/fr2gjb.
Hwang WJ, Hong O, Kim MJ. Factors associated with blue-collar workers’ risk perception of cardiovascular disease. J Korean Acad Nurs. 2012;42(7):1095-104. http://doi.org/cjfr.
Lang JP, Bonnewitz ML, Kusterer M, Lalanne-Tongio L. Usage d’alcool chez les patients souffrant de troubles psychiatriques : quelles évaluations? Quelle prise en soin?Encephale. 2014;40(4):301-7. http://doi.org/cjfs.
Alves H, Kessler F, Ratto LR. Comorbidity: alcohol use and other psychiatric disorders. Rev Bras Psiquiatt. 2004;26(Suppl 1):51-3. http://doi.org/bq5wk6.
Gonzalez VM, Bradizza CM, Vincent PC, Stasiewicz PR, Paas ND. Do individuals with a severe mental illness experience greater alcohol and drug-related problems? A test of the supersensitivity hypothesis. Addict Behav. 2007;32(3):477-90 http://doi.org/bww5hz.
Morris M, Johnson D, Morrison DS. Opportunities for prevention of alcohol-related death in primary care: results from a population-based cross-sectional study. Alcohol. 2012;46(7):703-7. http://doi.org/f37rmg.
Whitlock EP, Polen MR, Green CA, Orleans T, Klein J. Behavioral counseling interventions in primary care to reduce risky/harmful alcohol use by adults: a summary of the evidence for the US Preventive Services Task Force. Ann Intern Med. 2004;140(7):557-68. http://doi.org/cjft.
Carter MA. Review: brief multicontact behavioural counselling interventions in primary care reduce risky or harmful alcohol use. Evid Based Nurs. 2004;7(4):108. http://doi.org/cm988p.
US Preventive Services Task Force. Screening and counseling to reduce alcohol misuse: recommendations from the United States Preventive Services Task Force. Ann Intern Med. 2004;140(7):1-64. http://doi.org/cjfv.
Romelsjö A, Diderichsen F. Changes in alcohol-related inpatient care in Stockholm County in relation to socioeconomic status during a period of decline in alcohol consumption. Am J Public Health. 1989;79(1):52-6.
Jones L, Bates G, McCoy E, Bellis MA. Relationship between alcohol-attributable disease and socioeconomic status, and the role of alcohol consumption in this relationship: a systematic review and meta-analysis. BMC Public Health. 2015;15:400. http://doi.org/4d6.
Cómo citar
APA
ACM
ACS
ABNT
Chicago
Harvard
IEEE
MLA
Turabian
Vancouver
Descargar cita
Licencia
Derechos de autor 2018 Revista de la Facultad de Medicina

Esta obra está bajo una licencia Creative Commons Reconocimiento 3.0 Unported.
-