Síndrome constitucional y anemia como debut de vasculitis en un adulto mayor. Reporte de caso
Constitutional symptoms and anemia as the initial manifestation of vasculitis in an older adult. Case Report
DOI:
https://doi.org/10.15446/cr.v7n2.89388Keywords:
Adulto mayor, Anemia, Insuficiencia renal, Vasculitis sistémica (es)Aged, Anemia, Renal Insufficiency, Systemic Vasculitis (en)
Introducción. Las vasculitis son enfermedades graves que suelen tener un debut muy inespecífico y un diagnóstico tardío, lo que implica una alta tasa de fracaso terapéutico. Se presenta un caso de vasculitis que puede contribuir a considerar esta enfermedad como parte del diagnóstico diferencial desde las primeras etapas del proceso de atención para garantizar un abordaje integral y un inicio temprano del tratamiento, lo que reduciría la morbimortalidad asociada a estas entidades y mejoraría la tasa de éxito de los tratamientos.
Presentación del caso. Mujer caucásica de 77 años que como único antecedente presentaba hipertensión arterial de dos años de evolución y quien consultó al servicio de urgencias de una institución de segundo nivel por cuadro clínico de un mes de evolución consistente en astenia, febrícula, hiporexia y pérdida de peso. La paciente fue hospitalizada para completar la historia clínica y dados los hallazgos se sospechó de una posible translocación bacteriana secundaria a una neoplasia intestinal y se inició cobertura antibiótica empírica, pero su condición seguía empeorando. Se realizaron pruebas complementarias que no arrojaron resultados concluyentes; ante la persistencia de la fiebre, la insuficiencia renal y la anemia, se realizó una biopsia de riñón que mostró vaso arterial con necrosis fibrinoide e infiltrados de polimorfonucleares asociados, claros signos de una vasculitis activa del tipo poliangeítis microscópica. Se instauró el tratamiento indicado pero la paciente tuvo una evolución desfavorable y falleció.
Conclusiones. La exposición de este caso inusual contribuye a que los profesionales de la salud consideren el diagnóstico de vasculitis desde el inicio de la atención, aun cuando la sintomatología sugiere otras patologías o incluso cuando se presentan síntomas tan inespecíficos como anemia y pérdida de peso, ya que esto ayudará a establecer un diagnóstico temprano.
Introduction: Vasculitis comprises a group of often serious diseases that have an unspecific onset and a late diagnosis. The following report describes a case of vasculitis that may lead to considering this disorder as a differential diagnosis from the beginning of the care process to ensure a comprehensive approach and early treatment initiation that reduce associated morbidity and mortality and improve the success rate of treatments.
Case presentation: A 77-year-old female, with a 2-year history of arterial hypertension was admitted to the emergency department of a secondary care center for having experienced symptoms of asthenia, fever, hyporexia and weight loss for a month.
The patient was hospitalized for further testing and, given the findings, a possible bacterial translocation secondary to intestinal neoplasm was suspected. Empirical antibiotic treatment was started, but her condition continued to worsen. Complementary tests were performed, although they were not conclusive. Due to the persistence of fever, kidney failure and anemia, a kidney biopsy was performed, revealing arterial vessel with fibrinoid necrosis and associated polymorphonuclear infiltrates, clear signs of an active vasculitis of the microscopic polyangiitis type. Several lines of treatment were used, but the patient evolved unfavorably and died.
Conclusions: The presentation of this unusual case intends to contribute to the early diagnosis of this disorder by making medical staff aware of the possibility of considering it when symptoms suggest other diseases, or even when nonspecific symptoms such as anemia and weight loss occur.
https://doi.org/10.15446/cr.v7n2.89388
Constitutional symptoms and anemia as the initial manifestation of vasculitis in an older adult. Case Report
Keywords: Aged; Anemia; Renal Insufficiency; Systemic Vasculitis.
Palabras clave: Adulto mayor; Anemia; Insuficiencia renal; Vasculitis sistémica.
Virginia Naranjo-Velasco
Patricia Rubio-Marín
Juan Carlos Anglada-Pintado
Hospital Universitario de Jerez de la Frontera - Internal Medicine Service -
Cadiz - Spain.
Marta Pastor-Mena
Hospital Universitario de Jerez de la Frontera - Rheumatology Service -
Cadiz - Spain.
Corresponding author
Patricia Rubio-Marín. Servicio de Medicina Interna, Hospital Universitario de Jerez de la Frontera.
Cádiz. España.
Email: prubiomarin@gmail.com.
Received: 24/07/2020 Accepted: 20/04/2021
Resumen
Introducción. Las vasculitis son enfermedades graves que suelen tener un debut muy inespecífico y un diagnóstico tardío, lo que implica una alta tasa de fracaso terapéutico. Se presenta un caso de vasculitis que puede contribuir a considerar esta enfermedad como parte del diagnóstico diferencial desde las primeras etapas del proceso de atención para garantizar un abordaje integral y un inicio temprano del tratamiento, lo que reduciría la morbimortalidad asociada a estas entidades y mejoraría la tasa de éxito de los tratamientos.
Presentación del caso. Mujer caucásica de 77 años que como único antecedente presentaba hipertensión arterial de dos años de evolución y quien consultó al servicio de urgencias de una institución de segundo nivel por cuadro clínico de un mes de evolución consistente en astenia, febrícula, hiporexia y pérdida de peso. La paciente fue hospitalizada para completar la historia clínica y dados los hallazgos se sospechó de una posible translocación bacteriana secundaria a una neoplasia intestinal y se inició cobertura antibiótica empírica, pero su condición seguía empeorando. Se realizaron pruebas complementarias que no arrojaron resultados concluyentes; ante la persistencia de la fiebre, la insuficiencia renal y la anemia, se realizó una biopsia de riñón que mostró vaso arterial con necrosis fibrinoide e infiltrados de polimorfonucleares asociados, claros signos de una vasculitis activa del tipo poliangeítis microscópica. Se instauró el tratamiento indicado pero la paciente tuvo una evolución desfavorable y falleció.
Conclusiones. La exposición de este caso inusual contribuye a que los profesionales de la salud consideren el diagnóstico de vasculitis desde el inicio de la atención, aun cuando la sintomatología sugiere otras patologías o incluso cuando se presentan síntomas tan inespecíficos como anemia y pérdida de peso, ya que esto ayudará a establecer un diagnóstico temprano.
Abstract
Introduction: Vasculitis comprises a group of often serious diseases that have an unspecific onset and a late diagnosis. The following report describes a case of vasculitis that may lead to considering this disorder as a differential diagnosis from the beginning of the care process to ensure a comprehensive approach and early treatment initiation that reduce associated morbidity and mortality and improve the success rate of treatments.
Case presentation: A 77-year-old female, with a 2-year history of arterial hypertension was
admitted to the emergency department of a secondary care center for having experienced symptoms of asthenia, fever, hyporexia and weight loss for a month. The patient was hospitalized for
further testing and, given the findings, a possible bacterial translocation secondary to intestinal neoplasm was suspected. Empirical antibiotic treatment was started, but her condition continued to worsen. Complementary tests were performed, although they were not conclusive. Due to the persistence of fever, kidney failure and anemia, a kidney biopsy was performed, revealing arterial vessel with fibrinoid necrosis and associated polymorphonuclear infiltrates, clear signs of an active vasculitis of the microscopic polyangiitis type. Several lines of treatment were used, but the patient evolved unfavorably and died.
Conclusions: The presentation of this unusual case intends to contribute to the early diagnosis of this disorder by making medical staff aware of the possibility of considering it when symptoms suggest other diseases, or even when nonspecific symptoms such as anemia and weight loss occur.
Introduction
Primary systemic vasculitis is a heterogeneous group of highly complex and severe clinical processes characterized by inflammation and necrosis of blood vessels. The location and size of those vessels, as well as the severity of the damage and the histological pattern of involvement, are the features that differentiate each type of vasculitis and allow for their individualization (1).
A proper clinical assessment includes the preparation of a detailed medical history, doing a comprehensive physical examination, and requesting certain complementary tests. However, vasculitis is not usually considered as part of the differential diagnosis since the first moments of care because it has nonspecific symptoms, thus delaying diagnosis and implementation of appropriate treatment (2).
The following is the case of a patient with a rare type of vasculitis, which may prompt health staff to consider this diagnosis from the beginning.
Case presentation
A 77-year-old middle-class woman of Spanish origin, retired, and with a good quality of life, attended the emergency department of a secondary care center in the city of Jerez de la Frontera, Spain, on July 1, 2019. She reported symptoms consisting of asthenia, fever, hyporexia and weight loss of 7kg for a month (Figure 1). The patient claimed that she had no relevant family history but a personal history of arterial hypertension for two years treated with angiotensin II receptor blockers; she also stated that she was neither a smoker nor a habitual alcohol user.

Figure 1. Timeline showing the dates of the most important procedures and interventions performed on the patient.
Source: Own elaboration.
Laboratory tests performed on the day of hospital admission showed hemoglobin of 7.4 g/dL with mean corpuscular volume (MCV) of 75fL and creatinine of 1.6 g/dL. Since previous values (one year earlier) were normal, she was admitted to the hospital in the internal medicine unit at 17:54 on the same day to complete the clinical assessment.
During the interview, the patient reported experiencing melena without alteration of the intestinal transit, as well as weight loss (7kg) and asthenia. On physical examination, her blood pressure was normal. She was awake and alert, with adequate skin and mucous membrane hydration, and no adenopathies, neurological alterations or dermal lesions, or organomegaly. Her temperature was 37.5ºC and her body mass index was 23 kg/m2. Cardiac auscultation revealed that the heart was rhythmic, with normal pulse rate and no murmurs, while respiratory auscultation showed normal breath sounds. The abdomen was normal and bilateral kidney percussion was negative. No edema was evident, and all four limbs maintained their usual strength.
At 24 hours after admission, the patient had fever over 38ºC and a possible bacterial translocation secondary to intestinal neoplasm was suspected. Therefore, serial blood cultures were taken, and empirical antibiotic treatment was initiated with ceftriaxone 1g IV every 24 hours for 7 days. Despite the treatment provided, the fever did not go down and the overall condition of the woman did not improve; in fact, blood tests taken 10 days after admission (July 10, 2019) showed a deterioration in her condition (Table 1).
Table 1. Timeline of the patient’s blood tests.
|
Blood test |
01/07/2019 First day of hospitalization |
10/07/2019 Tenth day of hospitalization |
Reference values |
|
Glucose (mg/dL) |
89 |
69 |
80-110 |
|
Creatinine (mg/dL) |
2.25 |
6.19 |
0.5-1.11 |
|
Urea (mg/dL) |
86 |
216 |
21-43 |
|
GF (mL/min) |
20.44 |
6.01 |
90-100 |
|
Uric acid (mg/dL) |
6.1 |
11 |
2.6-6 |
|
Proteins (g/dL) |
6.2 |
5.4 |
6.4-8.3 |
|
Albumin (g/dl) |
3 |
2.6 |
3.2-4.6 |
|
Total bilirubin(mg/dL) |
0.6 |
3.1 |
0.30-1.20 |
|
AST (U/L) |
20 |
22 |
5-37 |
|
ALT (U/L) |
16 |
20 |
5-33 |
|
GGT (U/L) |
27 |
89 |
9-36 |
|
ALP (U/L) |
100 |
149 |
40-150 |
|
LDH (U/L) |
186 |
300 |
120-225 |
|
CK (U/L) |
15 |
43 |
29-169 |
|
TROP (ng/L) |
13 |
433 |
2.0-15.6 |
|
Sodium (mEq/L) |
135 |
125 |
135-145 |
|
Potassium (mEq/L) |
3.6 |
4.2 |
3.5-5.1 |
|
Phosphorus (mg/dL) |
3 |
6.1 |
2.3-4.7 |
|
Calcium (mg/dL) |
8 |
7 |
8.8-10.2 |
|
NT-proBNP (pg/mL) |
10.000 |
>35.000 |
0-300 |
|
C-reactive protein (mg/L) |
180 |
196 |
0.0-5.0 |
|
Procalcitonin |
1 |
9.5 |
0.02-0.5 |
|
ESR (mm/h) |
90 |
100 |
0.0-30.1 |
|
Hemoglobin (g/dL) |
10 |
7.4 |
11.8-15.8 |
|
Leukocytes (x10^3) |
12.10 |
19.89 |
3.6-10.5 |
|
Neutrophils (x10^3) |
10.82 |
15.45 |
1.5-7.5 |
|
Platelets (x10^3) |
348 |
489 |
130-400 |
|
Sediment in urine |
|||
|
Proteins (mg/dL) |
0 |
50 |
0 |
|
Red blood cells (UL) |
30 |
300 |
0 |
GF: glomerular filtration rate; AST: aspartate aminotransferase; ALT: alanine aminotransferase; GGT: gamma glutamyl transferase; ALP: alkaline phosphatase; LDH: lactate dehydrogenase; CK: creatine kinase; TROP: troponin I; NT-ProBNP: N-terminal pro-b-type natriuretic peptide; ESR: erythrocyte sedimentation rate.
Source: Own elaboration.
As the patient’s condition continued to worsen, within 10 days of admission, antibiotic coverage was extended for 7 days to piperacillin 4g and tazobactam 500mg every 8 hours in extended perfusion adjusted for kidney function and linezolid 600mg every 12 hours for adequate coverage of gram-positive bacteria. Similarly, an echocardiographic study was requested to assess the existence of a possible hematogenous infectious endocarditis originated in an abdominal focus that could explain the persistence of the fever.
Both serial blood cultures and echocardiography were negative, and microbiological tests showed serology without acute infection. Tests for human immunodeficiency virus, hepatitis C virus, Coxiella burnetii, urine smear, mantoux and quantiFERON were also negative, while immunoglobulin G was positive for both cytomegalovirus and parvovirus B19. An additional finding was previous hepatitis B virus infection.
On the other hand, due to the constitutional symptoms and the anemia presented by the patient, a digestive neoplasm was suspected. A study of anemia was requested, showing saturation index of 8%; ferritin and iron levels of 421 ng/mL and 3 3mcg/dL, respectively; normal vitamin B12, folic acid and haptoglobin levels; and reticulocytes at 2%. Similarly, a fecal occult blood test (FOBT) was performed, which was positive in all 3 samples, and endoscopic studies (gastroscopy without findings and colonoscopy with uncomplicated diverticula without other findings) were performed for Helicobacter pylori, which was negative.
Given the lack of conclusive findings, chest and abdominal CT scans were performed, showing hiatal hernia, bilateral pleural effusion, fluid in the pelvis and a subcentimeter space-occupying liver lesion. The patient was also screened for chronic diseases that could explain the anemia and the onset of acute kidney failure by proteinogram, immunoglobulin chain quantification and immunofixation, tests that ruled out a monoclonal gammopathy.
Immunoglobulins A, G, and M were normal; hematuria (150 erythrocytes/field) and proteinuria (750mg proteins in 24 hours) were found in urine, although proteinuria in the 24-hour urine for Bence Jones was negative. The albumin-to-creatinine ratio was 160 mg/g, and the protein-to-creatinine ratio was 760 mg/dL, and renal echo-Doppler showed an increase in resistance rates of intraparenchymal arteries (Figures 2 and 3).

Figure 2. Renal Doppler ultrasound of the right kidney.
Source: Document obtained during the course of the study.
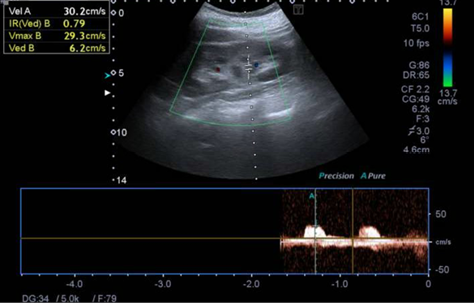
Figure 3. Renal Doppler ultrasound of the left kidney.
Source: Document obtained during the course of the study.
Although renal dysfunction was initially attributed to a prerenal kidney failure due to hyporexia, poor water intake and decreased blood flow due to anemia, it was necessary to look for other causes considering the progressive deterioration of the patient despite having implemented management with serum therapy and red blood cell concentrates.
Finally, due to the inconclusive results of the complementary tests and the persistence of fever, kidney failure and progressive anemia without externalization of bleeding despite the treatments given, the hypothesis that the patient suffered from an autoimmune disease of the vasculitis type was reinforced.
After expanding the spectrum of diagnostic tests to confirm the clinical suspicion, an autoimmunity study was performed. It was positive for perinuclear myeloperoxidase antineutrophil cytoplasmic antibodies (MPO-ANCA), with a 1/80 dilution. A Doppler ultrasound of temporal arteries was also performed and was normal (Figure 4). However, in view of the existing involvement, and since the confirmatory diagnosis of vasculitis is anatomopathological, a kidney biopsy was performed in which the presence of an arterial vessel with fibrinoid necrosis and associated infiltration of polymorphonuclear cells was observed. These are clear signs of active microscopic polyangiitis (MPA) vasculitis (Figure 5).

Figure 4. Doppler ultrasound of temporal arteries without alterations in temporal artery flow.
Source: Document obtained during the course of the study.
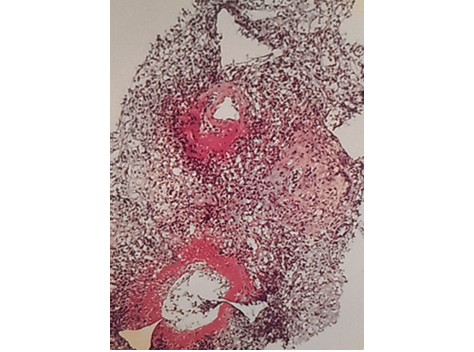
Figure 5. Kidney biopsy showing an arterial vessel with fibrinoid necrosis and associated polymorphonuclear infiltrates suggestive of microscopic polyangiitis.
Source: Document obtained during the course of the study.
After establishing the diagnosis of MAP, treatment was started with methylprednisolone 500mg per day for five days; however, the patient’s condition did not improve and she had complications in different target organs, requiring combination therapy as follows: acute renal failure with the need for replacement therapy prompted the initiation of management with cyclophosphamide 15 mg/kg IV every two weeks; the development of ischemic pancolitis required the administration of a single dose of rituximab 1g IV; and acute respiratory failure caused by alveolar hemorrhage (Figure 6) made it necessary to perform 5 sessions of plasmapheresis. Despite all efforts, the patient had an unfavorable course and died.
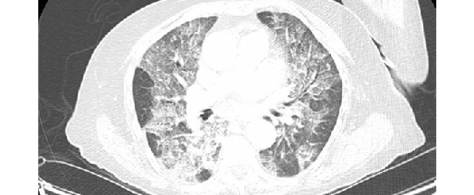
Figure 6. Computed tomography of the chest showing alveolar hemorrhage.
Source: Document obtained during the course of the study.
Discussion
According to the World Health Organization, anemia in older adults is defined as hemoglobin concentration <13g/dL in men and <12g/dL in women (3). This condition has a global prevalence ranging from 10% to 24% (4-5) and its origin is usually multifactorial: one third of cases are caused by nutritional deficiencies (iron, vitamin B12 or folic acid); another third is caused by chronic diseases (neoplastic, inflammatory and/or infectious processes), with or without associated kidney disease; and the causes of the other third are not clear (6).
When anemia occurs due to iron, folic acid, or vitamin B12 deficiency, it may be explained by bleeding lesions (benign or malignant), gastritis, polytherapy, H. pylori infection, malnutrition, intestinal malabsorption or inflammatory processes such as chronic kidney disease, cancer, autoimmune diseases or chronic infections (5).
In cases of microcytic or normocytic anemia, which are part of ferropenic anemias, a pattern with a transferrin saturation (TS) index <20% and ferritin level <30μg/L is usually observed; in these cases, FOBT tests and endoscopic studies are recommended. However, if TS<20% and ferritin levels >100μg/L are present, chronic inflammatory anemia caused by neoplasms, infections, or even autoimmune diseases should be considered (7). On the other hand, IS>20% suggests a renal or medullary origin, or deficiencies of vitamin B12 and folic acid (4).
The present case suggested a mixed pattern: microcytic anemia and occult blood in feces with elevated ferritin. Therefore, screening was performed for establishing gastrointestinal disorders, while other chronic conditions such as solid tumor, monoclonal gammopathy, infections (tuberculosis, infectious endocarditis, etc.) and viral and/or autoimmune diseases were subsequently ruled out.
The main causes of progressive kidney failure in the elderly include vascular nephropathy and diabetic nephropathy. However, ANCA vasculitis and vasculitis associated with monoclonal gammopathies are commonly developed by the elderly and may cause kidney damage (8).
In the present case, the patient had mild kidney damage with creatinine levels of 1.6 mg/dL, so it was considered that low food intake secondary to hyporexia and renal hypoperfusion had led to prerenal failure. Nevertheless, both the lack of response to serum therapy and red blood cell transfusion, as well as the progressive kidney failure led to search for other etiologies, including renal stenosis, monoclonal gammopathy, or vasculitis.
After ruling out a solid tumor, infectious causes, monoclonal gammopathy, and gastrointestinal bleeding, it was established that symptoms could be explained by the presence of an autoimmune disease, which led to request a kidney biopsy.
Vasculitis, defined as the presence of inflammatory leukocytes in the walls of blood vessels, comprises a group of conditions that cause both hemorrhagic and ischemic processes that can be primary or secondary to another underlying disease (infectious diseases, paraneoplastic syndromes, etc.) (9), and are classified according to the size of the vessel they affect and their location.
It is worth noting that the classification of vasculitis has generated great controversy for decades. Therefore, the 2012 Chapel Hill Consensus Conference on the Nomenclature of Systemic Vasculitides established a classification based mainly on the size of the affected vessel (9), bearing in mind that certain forms do not involve a single size. This classification indicated that vasculitis affecting small vessels include those that express ANCA and those that do not (10). However, ANCAs are not a criterion despite their potential value for clinical guidance.
Similarly, the 2012 Chapel Hill Consensus Conference included MPA, eosinophilic granulomatosis with polyangiitis (EGPA), and granulomatosis with polyangiitis (GPA) within vasculitis with positive ANCA. These are usually associated with specific markers such as myeloperoxidase (MPO-ANCA) or proteinase 3 (PR3-ANCA) (9). Moreover, PR3-ANCA vasculitis is the most frequent subgroup in the West and appears to be associated with greater multiorgan involvement (1).
Microscopic polyangiitis, on the other hand, is a necrotizing vasculitis that mainly affects the capillaries, venules or arterioles and it manifests more frequently as necrotizing glomerulonephritis and/or pulmonary capillaritis, with rare involvement at the digestive level. Medium and small arteries may also be involved in polyangiitis and early diagnosis is important to initiate adequate therapy and prevent organ failure, so a kidney biopsy should be performed for confirmation, although it should not delay the start of treatment (11).
Some limitations of the present case were the delay in diagnosis and the start of treatment; however, its main strength was diagnostic confirmation by anatomopathological study.
Conclusions
This case demonstrates the importance of a broad differential diagnosis in patients with constitutional symptoms of unknown etiology, in whom the most common causes should be ruled out, without forgetting other conditions that could explain their origin.
The information presented above, combined with the proper use of complementary tests, helps to confirm the diagnosis of disorders that can cause a variety of symptoms, such as the vasculitis described here, and to determine the most accurate therapeutic approach, which required a kidney biopsy in this case. Furthermore, early diagnosis allows for earlier initiation of treatment, which aids in obtaining a better response and avoiding consequences associated with a more severe disease.
Ethical considerations
This case report was approved by the Research Ethics Committee of the Hospital Universitario Puerto del Mar de Cadiz, belonging to the Andalusian Health Service of the Andalusian Regional Government, Spain, according to the minutes of October 30, 2020. Personal details were processed in accordance with the regulations in force in Spain (12).
Conflicts of interest
None stated by the authors.
Funding
None stated by the authors.
Acknowledgments
None stated by the authors.
ReferencEs
- Zazueta-Montiel B, Flores-Suárez LF. Ruta y retos diagnósticos en vasculitis primarias. Reumatol Clin. 2011;7(S3):S1-S6. https://doi.org/bjhttv.
- Tenorio-Cañamás MT, Galeano-Álvarez C, Rodríguez-Mendiola N, Liaño-García F. Diagnóstico diferencial de la insuficiencia renal aguda. NefroPlus. 2010;3(2):16-32. https://doi.org/f25sp3.
- WHO Scientific Group on Nutritional Anaemias & World Health Organization. Anemias nutricionales: informe de un Grupo Científico de la OMS [se reunió en Ginebra del 13 al 17 de marzo de 1967]. Ginebra: World Health Organization; 1968 [cited 2021 Jun 23]. Available from: https://bit.ly/3zPSr53.
- Gómez Ramírez S, Remacha Sevilla AF y Muñoz Gómez M. Anemia en el anciano. Med Clin (Barc). 2017;149(11):496-503. https://doi.org/gj66.
- Stauder R, Thein SL. Anemia in the elderly: clinical implications and new therapeutic concepts. Haematologica. 2014;99(7):1127-30. https://doi.org/gj7f.
- Robalo-Nunes A, Fonseca C, Marques F, Belo A, Brilhante D, Cortez J. Prevalence of anemia and iron deficiency in older Portuguese adults: An EMPIRE substudy. Geriatr Gerontol Int. 2017;17(11):1814-22. https://doi.org/gj7g.
- Muñoz M, Gómez-Ramírez S, Kozek-Langeneker S, Shander A, Richards T, Pavía J, et al. «Fit to fly»: overcoming barriers to preoperative haemoglobin optimization in surgical patients. Br J Anaesth. 2015;115(1):15-24. https://doi.org/gj7h.
- Hamroun A, Frimat M, Beuscart JB, Buob D, Lionet A, Lebas C, et al. Spécificités des néphropathies du sujet âgé. Nephro Ther. 2019;15(7):533-52. https://doi.org/ghb43w.
- Jennette JC, Falk RJ, Bacon PA, Basu N, Cid MC, Ferrario F, et al. 2012 revised International Chapel Hill Consensus Conference Nomenclature of Vasculitides. Arthritis Rheum. 2013;65(1):1-11. https://doi.org/b7cw.
- Guchelaar NAD, Waling MM, Adhin AA, van Daele PLA, Schreurs MWJ, Rombach SM.. The value of anti-neutrophil cytoplasmic antibodies (ANCA) testing for the diagnosis of ANCA-associated vasculitis, a systematic review and meta-analysis. Autoimmun Rev. 2021;20(1):102716. https://doi.org/gj7j.
- Jayne D. The diagnosis of vasculitis. Best Pract Res Clin Rheumatol. 2009;23(3):445-53. https://doi.org/bxrdzm.
- España. Jefatura del Estado. Ley Orgánica 3 de 2018 (diciembre 5): de Protección de Datos Personales y garantía de los derechos digitales. Madrid: Boletín Oficial del Estado 294; diciembre 6 de 2018.
References
Zazueta-Montiel B, Flores-Suárez LF. Ruta y retos diagnósticos en vasculitis primarias. Reumatol Clin. 2011;7(S3):S1-S6. https://doi.org/bjhttv. DOI: https://doi.org/10.1016/j.reuma.2011.10.001
Tenorio-Cañamás MT, Galeano-Álvarez C, Rodríguez-Mendiola N, Liaño-García F. Diagnóstico diferencial de la insuficiencia renal aguda. NefroPlus. 2010;3(2):16-32. https://doi.org/f25sp3.
WHO Scientific Group on Nutritional Anaemias & World Health Organization. Anemias nutricionales: informe de un Grupo Científico de la OMS [se reunió en Ginebra del 13 al 17 de marzo de 1967]. Ginebra: World Health Organization; 1968 [cited 2021 Jun 23]. Available from: https://bit.ly/3zPSr53.
Gómez Ramírez S, Remacha Sevilla AF y Muñoz Gómez M. Anemia en el anciano. Med Clin (Barc). 2017;149(11):496-503. https://doi.org/gj66. DOI: https://doi.org/10.1016/j.medcli.2017.06.025
Stauder R, Thein SL. Anemia in the elderly: clinical implications and new therapeutic concepts. Haematologica. 2014;99(7):1127-30. https://doi.org/gj7f. DOI: https://doi.org/10.3324/haematol.2014.109967
Robalo-Nunes A, Fonseca C, Marques F, Belo A, Brilhante D, Cortez J. Prevalence of anemia and iron deficiency in older Portuguese adults: An EMPIRE substudy. Geriatr Gerontol Int. 2017;17(11):1814-22. https://doi.org/gj7g. DOI: https://doi.org/10.1111/ggi.12966
Muñoz M, Gómez-Ramírez S, Kozek-Langeneker S, Shander A, Richards T, Pavía J, et al. «Fit to fly»: overcoming barriers to preoperative haemoglobin optimization in surgical patients. Br J Anaesth. 2015;115(1):15-24. https://doi.org/gj7h. DOI: https://doi.org/10.1093/bja/aev165
Hamroun A, Frimat M, Beuscart JB, Buob D, Lionet A, Lebas C, et al. Spécificités des néphropathies du sujet âgé. Nephro Ther. 2019;15(7):533-52. https://doi.org/ghb43w. DOI: https://doi.org/10.1016/j.nephro.2019.10.001
Jennette JC, Falk RJ, Bacon PA, Basu N, Cid MC, Ferrario F, et al. 2012 revised International Chapel Hill Consensus Conference Nomenclature of Vasculitides. Arthritis Rheum. 2013;65(1):1-11. https://doi.org/b7cw.
Guchelaar NAD, Waling MM, Adhin AA, van Daele PLA, Schreurs MWJ, Rombach SM.. The value of anti-neutrophil cytoplasmic antibodies (ANCA) testing for the diagnosis of ANCA-associated vasculitis, a systematic review and meta-analysis. Autoimmun Rev. 2021;20(1):102716. https://doi.org/gj7j. DOI: https://doi.org/10.1016/j.autrev.2020.102716
Jayne D. The diagnosis of vasculitis. Best Pract Res Clin Rheumatol. 2009;23(3):445-53. https://doi.org/bxrdzm. DOI: https://doi.org/10.1016/j.berh.2009.03.001
España. Jefatura del Estado. Ley Orgánica 3 de 2018 (diciembre 5): de Protección de Datos Personales y garantía de los derechos digitales. Madrid: Boletín Oficial del Estado 294; diciembre 6 de 2018.
How to Cite
APA
ACM
ACS
ABNT
Chicago
Harvard
IEEE
MLA
Turabian
Vancouver
Download Citation
License
Copyright (c) 2021 Case reports

This work is licensed under a Creative Commons Attribution 4.0 International License.
The authors, when submitting their manuscripts, accept to transfer to Case reports the copyright of the published articles. The publisher has the right of use, reproduction, transmission, distribution and publication in any form or medium. The authors cannot allow or authorize the use of the contribution without the written consent of the journal.
Uniform Disclosure Form for possible Conflicts of Interest, the assignment of rights and responsibility must be delivered together with the original.
Those authors who have publications with this journal accept the following terms:
The authors will keep their copyright and guarantee the journal the right of first publication of their work, which will be simultaneously subject to the Creative Commons Recognition License that allows third parties to share the work whenever its author is indicated and his first publication this journal
The authors may adopt other non-exclusive licensing agreements for the distribution of the published version of the work (eg, deposit it in an institutional telematic file or publish it in a monographic volume) whenever the initial publication in this journal is indicated.
Authors are allowed and advised to disseminate their work through the Internet (eg in institutional telematic files or on their website) before and during the submission process, which can produce interesting exchanges and increase citations of the published work. (See The effect of open access).