Foville syndrome: a neurological emergency of clinical relevance. Case report
Síndrome de Foville: una emergencia neurológica de gran relevancia clínica. Reporte de caso
DOI:
https://doi.org/10.15446/cr.v8n2.94010Keywords:
Stroke, Basilar Artery, Angiography, Brain Stem Infarctions (en)Accidente Cerebrovascular, Arteria Basilar, Angiografía, Infartos del Tronco Encefálico (es)
Abstract
Introduction: Foville syndrome (inferior medial pontine syndrome) is a clinical entity that makes part of a subclassification of a broader category of posterior circulation stroke. It is characterized by a blockage of the basilar artery caused by lesions in the pontine tegmentum. This syndrome has a very low incidence worldwide, but its clinical relevance is considerable.
Case report: A 41-year-old patient without any medical history was admitted to the emergency department due to signs of focal neurologic deficits. Imaging findings were compatible with an ischemic lesion in the brainstem, and cerebral angiography showed involvement of the basilar artery territory. The patient was diagnosed and followed up in the intensive care unit (ICU) until his recovery.
Conclusion: Foville syndrome is a rare disease with high morbidity and mortality. Early recognition and a multidisciplinary approach are decisive to improve the patient's prognosis.
Resumen
Introducción. El síndrome de Foville (síndrome pontino dorsal inferior) es una entidad clínica que hace parte de una subclasificación de la categoría más amplia de eventos cerebrovasculares de la circulación posterior, se presenta como resultado de la oclusión de la arteria basilar debido a lesiones en el tegmento pontino. Este síndrome tiene una muy baja incidencia a nivel mundial, pero es de gran relevancia clínica.
Presentación del caso. Hombre de 41 años sin antecedentes patológicos, que ingresó al servicio de urgencias por signos de focalización neurológica. Sus hallazgos imagenológicos fueron compatibles con una lesión isquémica en el tronco encefálico y la angiografía cerebral evidenció un compromiso en el territorio de la arteria basilar. El paciente fue diagnosticado y se le dio seguimiento en la unidad de cuidados intensivos (UCI) hasta su rehabilitación.
Conclusión. El síndrome de Foville es una enfermedad infrecuente y de alta mortalidad. El reconocimiento temprano de esta afección y un abordaje multidisciplinario son determinantes para mejorar el pronóstico del paciente.
https://doi.org/10.15446/cr.v8n2.94010
Foville syndrome: a neurological emergency of clinical relevance. Case report
Keywords: Stroke; Basilar Artery; Angiography; Brain Stem Infarctions.
Palabras clave: Accidente Cerebrovascular; Arteria Basilar; Angiografía; Infartos del Tronco Encefálico.
Julián Andrés Téllez-Villa
Rafael Figueroa-Casanova
Mónica Brigitte Mosos-Patiño
Carlos José Pérez-Rivera
Clínica Avidanti - Intensive Care Department - Ibagué - Colombia.
Néstor Pablo Guarnizo-Bustamante
Francisco José Molina-Sánchez
Omar Eduardo Zapata-Diaz
Clínica Nuestra - Intensive Care Department - Ibagué - Colombia.
Víctor Gil-Aldana
Clínica Nuestra - Interventional Cardiology, Hemodynamics and Peripheral Vascular
Department - Ibagué - Colombia.
Corresponding author
Julián Andrés Téllez-Villa. Clínica Avidanti, Ibagué. Colombia. Email: andresvilla2930@gmail.com
Received: 28/02/2021 Accepted: 08/11/2021
Resumen
Introducción. El síndrome de Foville (síndrome pontino medial inferior) es una entidad clínica que hace parte de una subclasificación de la categoría más amplia de eventos cerebrovasculares de la circulación posterior, se presenta como resultado de la oclusión de la arteria basilar debido a lesiones en el tegmento pontino. Este síndrome tiene una muy baja incidencia a nivel mundial, pero es de gran relevancia clínica.
Presentación del caso. Hombre de 41 años sin antecedentes patológicos, que ingresó al servicio de urgencias por signos de focalización neurológica. Sus hallazgos imagenológicos fueron compatibles con una lesión isquémica en el tronco encefálico y la angiografía cerebral evidenció un compromiso en el territorio de la arteria basilar. El paciente fue diagnosticado y se le dio seguimiento en la unidad de cuidados intensivos (UCI) hasta su rehabilitación.
Conclusión. El síndrome de Foville es una enfermedad infrecuente y de alta mortalidad. El reconocimiento temprano de esta afección y un abordaje multidisciplinario son determinantes para mejorar el pronóstico del paciente.
Abstract
Introduction: Foville syndrome (inferior medial pontine syndrome) is a clinical entity that makes part of a subclassification of a broader category of posterior circulation stroke. It is characterized by a blockage of the basilar artery caused by lesions in the pontine tegmentum. This syndrome has a very low incidence worldwide, but its clinical relevance is considerable.
Case report: A 41-year-old patient without any medical history was admitted to the emergency department due to signs of focal neurologic deficits. Imaging findings were compatible with an ischemic lesion in the brainstem, and cerebral angiography showed involvement of the basilar artery territory. The patient was diagnosed and followed up in the intensive care unit (ICU) until his recovery.
Conclusion: Foville syndrome is a rare disease with high morbidity and mortality. Early recognition and a multidisciplinary approach are decisive to improve the patient’s prognosis.
Introduction
Foville syndrome (inferior medial pontine syndrome) is a cerebrovascular disease of the brainstem that is rarely reported worldwide but has a mortality rate of more than 85% (1). It is characterized by the involvement of the paramedian perforating branches of the basilar artery that supply each side of the caudal paramedian pons, which is a critical area containing major nerve nuclei. The affected structures are the sensory and motor nuclei of the trigeminal nerve, the nucleus of the abducens nerve, the nucleus of the facial nerve, and the nuclei of the vestibulocochlear nerve (2). Critical structures for horizontal gaze, such as the paramedian pontine reticular formation and the medial longitudinal fasciculus (MFL) are also involved (2). In addition, the medial lemniscus, the spinothalamic tract and the descending pyramidal tracts that go through this region may also be affected (1-3) (Figure 1).
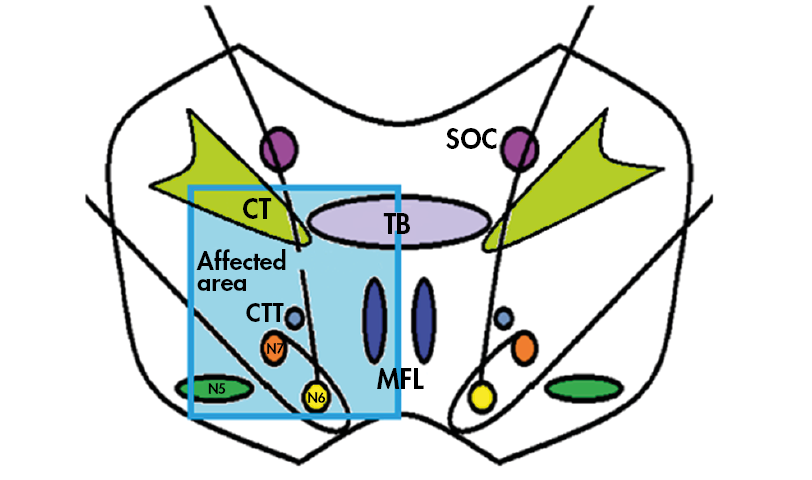
Figure 1. Figure of the pons depicting the affected anatomical area of the patient with Foville syndrome.
N5: trigeminal tract and nucleus; N6: nucleus abducens and fascicle; N7: facial nerve nucleus and fascicle; CTT: central tegmental tract; MFL: medial longitudinal fascicle; SOC: superior olivary complex; TB: trapezoid body; CT: corticospinal tract.
Source: Own elaboration.
Posterior circulation strokes account for approximately 15% to 20% of all strokes, and basilar artery occlusion, which is a subset of this category, represents 1% to 4% of all ischemic strokes (4).
Its clinical presentation is heterogeneous and is characterized by vertigo, headache, and cervical pain. When the lesion occurs unilaterally, the following signs are observed: ipsilateral conjugate gaze palsy due to involvement of the paramedian pontine reticular formation and/or the nucleus of the VI cranial nerve; facial paralysis and hypoesthesia; sensorineural hearing loss; and/or contralateral hemiparesis/hemiplegia secondary to a corticospinal tract lesion (5-7). Other signs include ataxia and Horner syndrome due to the involvement of afferent fibers in the white matter that are directed toward the middle cerebellar peduncle and sympathetic fibers, respectively (2,8,9) (Figure 2).
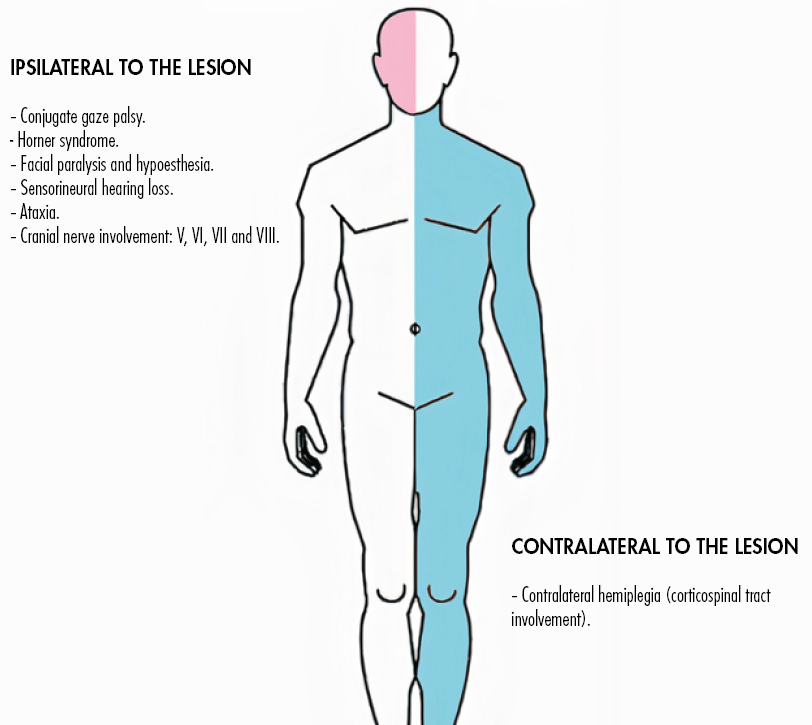
Figure 2. Graphic representation of neurological involvement in Foville syndrome.
Source: Own elaboration.
The most important treatment is antiplatelet therapy and management of vascular risk factors for secondary prevention (2,10). Treatment with antiplatelet agents and statins should begin upon admission to the hospital. The management of high blood pressure, diabetes, hyperlipidemia and smoking cessation adheres to the guidelines of the American Heart Association (AHA). Patients should be evaluated by physical or occupational therapists for rehabilitation following an acute stroke. Post-discharge follow-up and complications require outpatient care (2,10,11).
The following is a case that highlights the importance of combining knowledge of the anatomical structures with useful clinical findings in order to provide a timely diagnosis in cases of neurological emergencies.
Case Presentation
A 41-year-old male, Hispanic, resident of the city of Ibagué, Colombia, with no history of disease, visited the emergency service of a tertiary health care center in that same city with a one-day history of generalized headache associated with tinnitus, vertigo, emesis, and deviation of the labial commissure to the left. Physical examination on admission revealed normal vital signs, without fever. The neurological examination showed 15/15 on the Glasgow Coma Scale, vertical pendular nystagmus, normal horizontal gaze, isochoric pupils of 3mm reactive to light, bilateral fundus without papilledema or other alterations, oculocephalic and corneal reflexes, right facial paralysis, strong and deep tendon reflexes preserved in the four extremities, gait alteration with increased sustentation polygon, and no signs of meningitis or other neurological disorders. Cardiovascular, abdominal and thoracic findings were normal. Due to the diagnostic impression of a cerebrovascular disease, a non-enhanced CT scan of the brain was performed on admission, which found no alterations. The patient was admitted to the clinical neurology service 12 hours later.
On the following day, the patient presented with neurological deterioration that included dysarthria, generalized tonic-clonic seizure, and left hemiplegia; at that point, it was decided to admit him to the intensive care unit (ICU). Six hours after his admission to the ICU, his state of consciousness worsened, and he experienced stupor and ventilatory failure requiring airway support by orotracheal intubation and invasive mechanical ventilatory support.
After 48 hours of admission to the ICU, an enhanced brain MRI was requested, which showed involvement in the dorsal region. Moreover, an area of hyperintensity in FLAIR (fluid attenuated inversion recovery) and T2 was found to the right of the midline over the facial colliculus and median eminence, which restricted the diffusion sequence due to an acute stroke in the pontine region. These imaging findings led to conclude that the patient had a ischemic cerebrovascular disease of the vertebrobasilar arterial system, so studies were performed to determine the etiology (Figure 3).
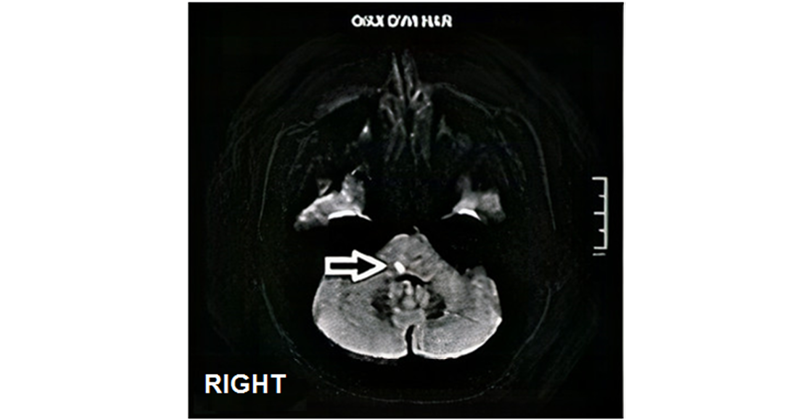
Figure 3. Enhanced magnetic resonance imaging of the brain. Axial diffusion section showing an ischemic area in the region of the pons to the right of the midline and towards the medial eminence and facial colliculus (horizontal arrow).
Source: Image obtained during the study.
Two days after his admission to the ICU, carotid and spinal Doppler ultrasound was performed with normal results, as well as thrombophilia tests (protein C,
protein S, antithrombin III, factor V Leiden, lupus anticoagulant, anti-cardiolipins,
and antiphospholipid antibodies), which ruled out hypercoagulability. On the third day, a transesophageal echocardiogram was requested, which showed no evidence of embolic origin, and on the fourth day, immunology laboratory tests were performed, which were negative for vasculitis. Six days after his admission to the ICU, a follow-up enhanced MRI of the brain was performed, which showed increased involvement of the brainstem with a significant lesion at the pons, being hypointense in T1, hyperintense in T2, and FLAIR (Figure 4).
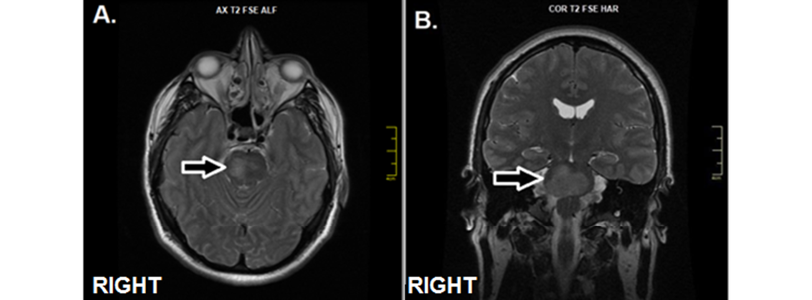
Figure 4. Enhanced magnetic resonance imaging of the brain. (A) Axial plane;
(B) T2-weighted coronal plane, showing significant subacute ischemic vascular lesions of the brainstem at the pons (horizontal arrow).
Source: Images obtained during the study.
Figure 5 shows lesions of the basal and posterior aspect of the left cerebellar hemisphere with similar characteristics, as well as lesions of a lesser degree in the right lateral aspect. These findings reflected subacute ischemic vascular lesions.
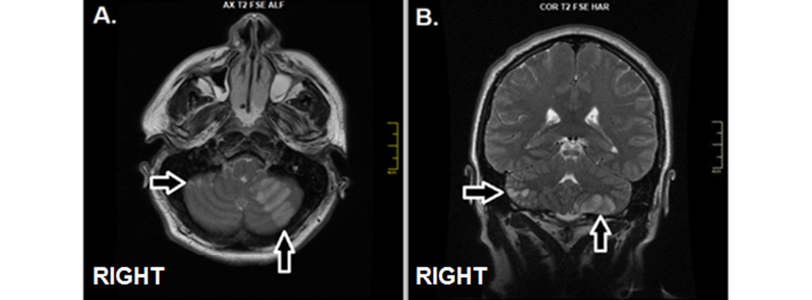
Figure 5. Enhanced magnetic resonance imaging of the brain. A) Axial plane;
B) T2-weighted coronal plane, showing subacute vasogenic edema and vascular ischemia of the basal and posterior region of the left cerebellar hemisphere (vertical arrow) and lateral region of the right cerebellar hemisphere (horizontal arrow).
Source: Images obtained during the study.
One week after admission to the health center, in order to identify the location and severity of the occlusion of the vertebrobasilar arterial system, the patient underwent a cerebral angiography that showed hypoplasia of the left vertebral artery, of aortic origin, ending in the posterior inferior cerebellar artery (PICA), without atherosclerotic changes or signs of dysplasia. At the intracranial level, occlusion of the entire right V4 vertebral segment and the lower two thirds of the basilar artery was documented, as well as a possible dissection without segmental alterations in the caliber of the vessels suggestive of vasculitis (Figure 6).
Based on clinical signs and in correlation with imaging and cerebral angiographic findings, a diagnosis of Foville syndrome was made.
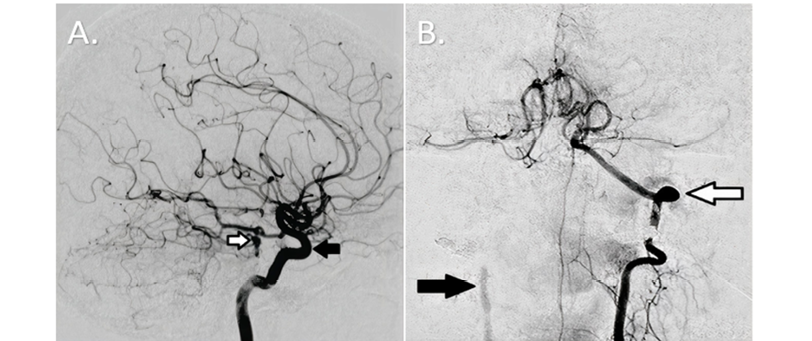
Figure 6. Cerebral angiography. A) Basilar artery (white arrow) occluded in its lower two thirds and left vertebral artery (black arrow); B) Right vertebral artery, occluded V4 segment (black arrow), and hypoplastic left vertebral artery (white arrow) ending in the posterior inferior cerebellar artery.
Source: Images obtained during the study.
The patient was outside the therapeutic range for thrombolysis and was not a candidate for mechanical endovascular treatment. He also required antiplatelet therapy (acetylsalicylic acid 100mg/day orally for 6 months), anticoagulation with low molecular weight heparin (enoxaparin 1mg/kg/day subcutaneously for 2 months), and statins (atorvastatin 40mg/day orally for 6 months). Two weeks after his admission to the ICU, he underwent a tracheostomy and gastrostomy; he did not require additional treatments or follow-up diagnostic support and did not present any adverse events associated with the interventions performed.
During his stay in the ICU, the patient’s brainstem reflexes were preserved, and the sleep-wake cycles were preserved with unimpaired cardiovascular and respiratory function; however, he never showed evidence of self-awareness or connection with the environment. Likewise, there were no voluntary movements, no comprehensible language or sphincter control, and he met the criteria for persistent vegetative state. Likewise, differential diagnoses such as minimally state were ruled out and coma was excluded since the patient preserved the sleep-wake cycles. In view of his impaired consciousness and the absence of communication through eye movements, he did not meet the criteria for the diagnosis of locked-in syndrome either.
After 24 days in the ICU, the patient was transferred to the clinical neurology hospitalization service, where he continued treatment by this specialty and completed 48 days of comprehensive care. Finally, he was discharged and continued with physical and speech therapy; however, 7 months after hospital discharge, he died as a result of community-acquired pneumonia.
Discussion
The vertebrobasilar arterial system comprises the extracranial and intracranial vertebral arteries (Figure 7), which join to form the basilar artery that runs midline along the ventral surface of the brainstem and gives rise to the bilateral anterior inferior cerebellar arteries, multiple paramedian and circumferential perforating pontine arteries, and the two superior cerebellar arteries (12-14).

Figure 7. Anatomical view of the path of the lateral (A) and anterior (B) vertebral artery.
V0-V4: segments of the vertebral artery; V0: origin in the subclavian artery; V1: from the origin of the vertebral artery to its entry into the transverse foramen of the cervical vertebrae C6; V2: from the entry into the transverse foramen of the cervical vertebrae C6 to the transverse foramen of the cervical vertebrae C2; V3: from the transverse foramen of cervical vertebrae C2 to the skull base; V4: intracranial segment. The vertebral arteries fuse to form the basilar artery and are intradural.
Source: Own elaboration.
As the basilar artery approaches the base of the pituitary gland, it divides to originate bilateral posterior cerebral arteries and the latter, in turn, anastomose with the ipsilateral internal carotid arteries through the posterior communicating arteries, completing the circle of Willis (Figure 8) (14) (14).
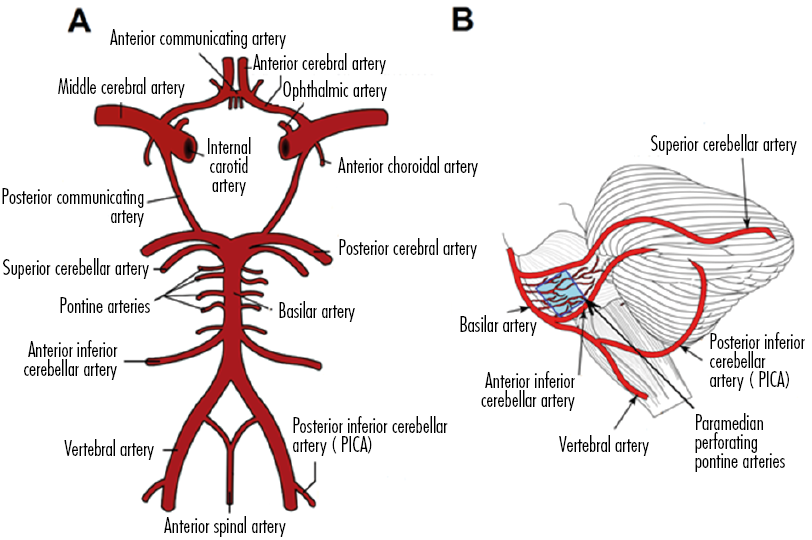
Figure 8. Graphic representation of the vertebrobasilar arterial system. A) Circle of Willis; B) Graphic representation of the brainstem (lateral view), the blue box shows the involvement of the paramedian perforating pontine arteries at the level of the paramedian caudal pons, a critical area affected in Foville syndrome.
Source: Own elaboration.
The vertebrobasilar arterial system perfuses the medulla, cerebellum, pons, midbrain, thalamus, and occipital cortex. An ischemia in this system has a mortality rate of more than 85% (1,15,16). Due to the involvement of the brainstem and cerebellum, most survivors develop multiple organ dysfunction and complications (respiratory infections, urinary tract infections, pulmonary embolism, depression, anxiety, and epilepsy) (17). Latency between the first prodromal symptoms and the onset of the stroke can last from days to months. The most common prodromal symptoms are vertigo and nausea, followed by headache and neck pain (4,18,19). In turn, the distinction between central and peripheral vertigo is clinically relevant, as late recognition of vascular vertigo leads to missed opportunities for thrombolysis and/or thrombectomy and may increase the risk of death and disability (4).
The Head Impulse, nystagmus type, and Test of Skew (HINTS) protocol evaluates the head impulse test, the nystagmus type, and the Skew test. The Head Impulse test uses the oculocephalic maneuver to assess the vestibulo-ocular reflex that generates a contralateral ocular deviation when the head is turned rapidly to one side. In nystagmus type, vertical nystagmus is a clear sign of central nervous system involvement; however, nystagmus with a predominantly horizontal vector can occur and is also associated with cerebrovascular disease. Finally, in the Skew test, an alternating ocular occlusion (cover test) is performed in order to detect ocular deviation in the vertical plane, with the purpose of looking for vertical or diagonal corrective ocular movements to maintain alignment. If the cephalic impulse test is normal, the nystagmus is vertical or changes direction, and there is also a vertical ocular deviation. This test has a sensitivity of 100% and specificity of 96% for cerebrovascular disease (20-22). The HINTS protocol has been proven to outperform brain MRI in the diagnosis of ischemic cerebrovascular disease in the first two days of onset of vertigo (4).
The most common causes of ischemia of the vertebrobasilar circulation include embolism, large artery atherosclerosis, penetrating small artery disease, and arterial dissection (23-25). Atherosclerotic intrinsic stenosis of the basilar artery is the most common cause and occurs most frequently in the sixth and seventh decade of life (26). Occlusion of the basilar artery secondary to cardiac or vertebral artery embolism is another significant cause (27-29). However, other etiologies such as hemorrhages, granulomas and tumors in the pons have been reported (9). All patients in whom occlusion of the vertebrobasilar arterial system is suspected should undergo neuroimaging (30,31).
Although non-enhanced brain tomography is sensitive for detecting intracranial hemorrhage, it is not particularly sensitive for the diagnosis of acute ischemic cerebrovascular disease, especially in the posterior cerebral circulation (4). In a brain CT scan without enhancement, a sign of hyperdensity of the basilar artery can be observed in 50% to 70% of patients with basilar artery thrombosis (4), which is presumed to represent a thrombus or clot (32,33,34). In general, sensitivity, specificity and reliability are low for this finding, and in most cases should not be used for direct patient care. However, in patients with a high probability of ischemic cerebrovascular disease of the posterior circulation, the presence of a hyperdense basilar artery is a specific predictor of basilar artery occlusion (4).
When a hypodense image in the territory of the posterior cerebral circulation is observed on brain tomography, the computed tomography-guided posterior circulation Alberta stroke program early CT scores (PC-ASPECTS) can be used to quantify early ischemia. This scoring system assigns posterior cerebral circulation 10 points in total, with points subtracted for ischemic changes. Thus, 1 point is subtracted for changes in the left or right thalamus, cerebellum or posterior cerebral artery territory and 2 points are subtracted for any hypodensity in the midbrain or pons (35,36). This scoring system has a higher sensitivity in predicting final infarct size and individuals who will have a poor functional outcome despite basilar artery recanalization (4,37,38). A PC-ASPECTS score of 8 or higher on MRI (or computed tomography angiography) is an independent predictor of favorable outcome, whereas a score of less than 8 may indicate patients with high mortality (4).
On the other hand, brain MRI is more sensitive than a non-enhanced brain CT scan for the detection of acute ischemic cerebrovascular disease (39). It is estimated that 50% of patients with cerebrovascular disease who present with isolated vertigo will have a false negative MRI up to 48 hours after onset (40-42). Doppler ultrasound is widely used in order to identify carotid stenosis, but it is much less sensitive in the detection of vertebral artery stenosis (16,43). The gold standard for vascular imaging is cerebral angiography and should be considered when initial noninvasive imaging is not diagnostic (4).
Acute treatment aims to restore cerebral blood flow to the occluded vessel and save brain tissue. If occlusion in the vertebrobasilar circulation is suspected, the first critical step is to verify that the patient can protect their airway, as acute symptoms may progress to decreased alertness, decreased respiratory drive, and coma (4). Available treatments include intravenous thrombolysis, intra-arterial thrombolysis, and/or endovascular mechanical treatment (44-46). If the brain CT scan does not reveal hemorrhage and symptoms begin within 4.5 hours from the onset of ischemic cerebrovascular disease, intravenous tissue plasminogen activator (tPA) is the standard treatment (4,47,48). Patients should be carefully monitored with MRI in order to assess cerebellar edema, which usually peaks 3 to 5 days after the stroke and may cause compression of the fourth ventricle and/or cerebral herniation (4).
After initial stabilization, etiology should be established by means of the following tests: complete blood count, lipid profile, C-reactive protein, coagulation panel, antiphospholipid antibodies, anticardiolipins, lupus anticoagulant, analysis of prothrombotic states, and echocardiogram to evaluate potential sources of emboli. In addition, patients should undergo continuous cardiac monitoring to detect cardiac arrhythmias (atrial fibrillation, etc.) (49). Identification of the cause is critical for choosing secondary prevention therapy (50,51).
In the case reported, the clinical manifestations were well correlated with anatomical involvement, evidencing semiology features representative of ischemia in the posterior cerebral circulation. Headache and vertigo were the initial prodromal symptoms and magnetic resonance imaging was superior to brain tomography in showing ischemia in the vertebrobasilar arterial system.
A limitation of this case, identified when reviewing the available literature, is the scarce development of guidelines for the care and management of cerebrovascular disease of the posterior circulation. More clinical research studies targeting the posterior cerebral circulation are needed to facilitate the diagnostic and therapeutic approach. In turn, strengths include a detailed neurological examination and imaging studies that allowed for a comprehensive assessment and multidisciplinary management of the patient.
Conclusion
Foville syndrome is a neurological emergency with a high mortality rate that requires a high index of suspicion. Patients presenting with sudden onset of headache or vertigo require an accurate neurological assessment. As soon as the diagnosis is confirmed by neuroimaging, intravenous thrombolysis or endovascular treatment should be performed to give patients a better chance of survival and avoid serious complications.
Ethical considerations
Informed consent was obtained from the patient’s legal guardians for the publication of this case report. Approval was also obtained from the institution’s ethics committee on May 27, 2021, minutes number: 27521.
Conflict of interest
None stated by the authors.
Funding
None stated by the authors.
Acknowledgments
To Dr. Carlos Hernán Roa, specialist in neuroradiology and interventional cardiologist at Fundación Clínica Shaio, in Bogotá, for his invaluable contribution to the assessment and review of the imaging scans.
References
1.Kaye V, Brandstater ME, Talavera F, Salcido R, Kishner S, Klein MJ. Vertebrobasilar Stroke. Medscape; 2020. [cited 2021 Apr 28]. Available from: https://bit.ly/3weOgzd.
2.Khazaal O, Marquez DL, Naqvi IA. Foville Syndrome. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2020. [cited 2021 Apr 28]. Available from: https://bit.ly/3J5hGYa.
3.Beucler N, Boissonneau S, Ruf A, Fuentes S, Carron R, Dufour H. Crossed brainstem syndrome revealing bleeding brainstem cavernous malformation: an illustrative case. BMC Neurol. 2021;21(1):204. https://doi.org/js69.
4.Demel LS, Broderick PJ. Basilar Occlusion Syndromes: An Update. The Neurohospitalist. 2015;5(3):142-50. https://doi.org/js7b.
5.Selvadurai C, Rondeau MW, Colorado RA, Feske SK, Prasad S. Teaching Video NeuroImages: Foville syndrome. Neurology. 2016;86(19):e203. https://doi.org/gmmhs7.
6.Man BL, Fu YP. Bronchogenic carcinoma presented as Foville’s syndrome. BMJ Case Rep. 2015;2015:bcr2014205025. https://doi.org/js7j.
7.Stephen M, Jayasri, Harigaravelu PJ, Baranitharan. Pontine hemorrhage presenting as Foville’s syndrome. IJAM. 2021;8(8):1226-8. https://doi.org/js7k.
8.Hubloue I, Laureys S, Michotte A. A rare case of diplopia: medial inferior pontine syndrome or Foville’s syndrome. Eur J Emerg Med. 1996;3(3):194-8. https://doi.org/bnzpqj.
9.Massi DG, Nyassinde J, Ndiaye MM. Superior Foville syndrome due to pontine hemorrhage: a case report. Pan Afr Med J. 2016;25:215. https://doi.org/js7q.
10.Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. Guidelines for the Early Management of Patients With Acute Ischemic Stroke: 2019 Update to the 2018 Guidelines for the Early Management of Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 2019;50(12):e344-e418. https://doi.org/dnbv.
11.Winstein CJ, Stein J, Arena R, Bates B, Cherney LR, Cramer SC, et al. Guidelines for Adult Stroke Rehabilitation and Recovery: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 2016;47(6):e98-e169. https://doi.org/gsm7.
12.Salerno A, Strambo D, Nannoni S, Dunet V, Michel P. Patterns of ischemic posterior circulation strokes: A clinical, anatomical, and radiological review. Int J Stroke. 2022;17(7):714-22. https://doi.org/js7v.
13.Jenkins JS, Stewart M. Endovascular Treatment of Vertebral Artery Stenosis. Prog Cardiovasc Dis. 2017;59(6):619-25. https://doi.org/gbngbd.
14.Piccinin MA, Munakomi. S. Neuroanatomy, Vertebrobasilar System. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2022. [cited 2023 Jan 19]. Available from: https://bit.ly/3IWyMYh.
15.Alwood BT, Dossani RH. Vertebrobasilar Stroke. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2022. [cited 2023 Jan 19]. Available from: https://bit.ly/3Wn981J.
16.Markus HS, van der Worp HB, Rothwell PM. Posterior circulation ischaemic stroke and transient ischaemic attack: diagnosis, investigation, and secondary prevention. Lancet Neurol. 2013;12(10):989-98. https://doi.org/f2fnrd.
17.Langhorne P, Stott DJ, Robertson L, MacDonald J, Jones L, McAlpine C, et al. Medical complications after stroke: a multicenter study. Stroke. 2000;31(6):1223-9. https://doi.org/b78b8x.
18.Cheng H-C, Yen M-Y, Wang A-G. Foville’s syndrome with ipsilateral internuclear ophthalmoplegia due to spontaneous pontine hemorrhage. Taiwan J Ophthalmol. 2013;3(2):75-7. https://doi.org/js74.
19.Ferbert A, Brückmann H, Drummen R. Clinical features of proven basilar artery occlusion. Stroke. 1990;21(8):1135-42. https://doi.org/fh3vwj.
20.Yebra González L, González Márquez R, Rueda Marcos A, Salas Álvarez FJ, Sanz Fernández R, Martín Sanz E. Unclear origin vertigo protocol. Acta Otorrinolaringol (Engl Ed). 2021;72(2):92-100. https://doi.org/js75.
21.Kattah JC. Use of HINTS in the acute vestibular syndrome. An Overview. Stroke Vasc Neurol. 2018;3(4):190-6. https://doi.org/gf5dwb.
22.Sankalia D, Kothari S, Phalgune DS. Diagnosing Stroke in Acute Vertigo: Sensitivity and Specificity of HINTS Battery in Indian Population. Neurol India. 2021;69(1):97-101. https://doi.org/js76.
23.Baran G, Gultekin TO, Baran O, Deniz C, Katar S, Yildiz GB, et al. Association between etiology and lesion site in ischemic brainstem infarcts: a retrospective observational study. Neuropsychiatr Dis Treat. 2018;14:757-66. https://doi.org/gc73m7.
24.Boehme AK, Esenwa C, Elkind MSV. Stroke Risk Factors, Genetics, and Prevention. Circ Res. 2017;120(3):472-95. https://doi.org/f9tt4f.
25.Shi Y, Wardlaw JM. Update on cerebral small vessel disease: a dynamic whole-brain disease. Stroke Vasc Neurol. 2016;1(3):83-92. https://doi.org/gbzw3s.
26.Samaniego EA, Shaban A, Ortega-Gutierrez S, Roa JA, Hasan DM, Derdeyn C, et al. Stroke mechanisms and outcomes of isolated symptomatic basilar artery stenosis. Stroke Vasc Neurol. 2019;4(4):189-97. https://doi.org/gk8krz.
27.Savitz SI, Caplan LR. Vertebrobasilar disease. N Engl J Med. 2005;352(25):2618-26. https://doi.org/b2w49z.
28.Arauz A, Ruíz-Franco A. Enfermedad vascular cerebral. Rev Fac Med (Méx.). 2012 [cited 2023 Jan 19];55(3):11-21. Available from: https://bit.ly/2HHx5Oe.
29.Huang R, Zhang X, Chen W, Lin J, Chai Z, Yi X. Stroke Subtypes and Topographic Locations Associated with Neurological Deterioration in Acute Isolated Pontine Infarction. J Stroke Cerebrovasc Dis. 2016;25(1):206-13. https://doi.org/js8g.
30.Hui C, Tadi P, Patti L. Ischemic Stroke. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2022. [cited 2023 Jan 19]. Available from: https://bit.ly/3wji1z4.
31.Lima Neto AC, Bittar R, Gattas GS, Bor-Seng-Shu E, Oliveira M, Monsanto R, et al. Pathophysiology and Diagnosis of Vertebrobasilar Insufficiency: A Review of the Literature. Int Arch Otorhinolaryngol. 2017;21(3):302-7. https://doi.org/js8h.
32.Ng CF, Chong CY. Acute Basilar Artery Occlusion: Early Computed Tomography Finding Predicts Catastrophic Outcome. J Neurosci Rural Pract. 2018;9(4):653-4. https://doi.org/js8k.
33.Reinemeyer NE, Tadi P, Lui F. Basilar Artery Thrombosis. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2022. [cited 2023 Jan 19] Available from: https://bit.ly/3GLMASI.
34.Garg R, Biller J. Neuroimaging Predictors of Clinical Outcome in Acute Basilar Artery Occlusion. Front Neurol. 2017;8:293. https://doi.org/gf6ckz.
35.Pallesen L-P, Lambrou D, Eskandari A, Barlinn J, Barlinn K, Reichmann H, et al. Perfusion computed tomography in posterior circulation stroke: predictors and prognostic implications of focal hypoperfusion. Eur J Neurol. 2018;25(5):725-31. https://doi.org/js8m.
36.Caruso P, Ridolfi M, Lugnan C, Ajčević M, Furlanis G, Bellavita G, et al. Multimodal CT pc-ASPECTS in infratentorial stroke: diagnostic and prognostic value. Neurol Sci. 2021;42(10):4231-40. https://doi.org/js8n.
37.Lin S-F, Chen C-I, Hu H-H, Bai C-H. Predicting functional outcomes of posterior circulation acute ischemic stroke in first 36 h of stroke onset. J Neurol. 2018;265(4):926-32. https://doi.org/gdcsxw.
38.Kim JG, Lee D, Choi JC, Song Y, Lee DH, Suh DC. DWI-pc-ASPECT score in basilar artery occlusion: is 6 points or less always indicative of a bad outcome? Interv Neuroradiol. 2019;25(4):371-9. https://doi.org/js8p.
39.Hoyer C, Szabo K. Pitfalls in the Diagnosis of Posterior Circulation Stroke in the Emergency Setting. Front Neurol. 2021;12:682827. https://doi.org/js8q.
40.Tehrani ASS, Kattah JC, Mantokouis G, Pula JH, Nair D, Blitz A, et al. Small strokes causing severe vertigo: frequency of false-negative MRIs and nonlacunar mechanisms. Neurology. 2014;83(2):169-73. https://doi.org/f6cnfh.
41.Bulut HT, Yildirim A, Ekmekci B, Eskut N, Gunbey HP. False-negative diffusion-weighted imaging in acute stroke and its frequency in anterior and posterior circulation ischemia. J Comput Assist Tomogr. 2014;38(5):267-33. https://doi.org/f6j4bm.
42.Simonsen CZ, Madsen MH, Schmitz ML, Mikkelsen IK, Fisher M, Andersen G. Sensitivity of diffusion- and perfusion-weighted imaging for diagnosing acute ischemic stroke is 97.5%. Stroke. 2015;46(1):98-101. https://doi.org/f6v59j.
43.Brunser AM, Lavados PM, Cavada G, Muñoz-Venturelli P, Olavarría VM, Navia V, et al. Transcranial Doppler as a Predictor of Ischemic Events in Vertebral Artery Dissection. J Neuroimaging. 2020;30(6):890-5. https://doi.org/js8r.
44.Weber R, Minnerup J, Nordmeyer H, Eyding J, Krogias C, Hadisurya J, et al. Thrombectomy in posterior circulation stroke: differences in procedures and outcome compared to anterior circulation stroke in the prospective multicentre REVASK registry. Eur J Neurol. 2019;26(2):299-305. https://doi.org/gfftqk.
45.Nguyen TN, Strbian D. Endovascular Therapy for Stroke due to Basilar Artery Occlusion: A BASIC Challenge at BEST. Stroke. 2021;52(10):3410-3. https://doi.org/js8s.
46.Langezaal LCM, van der Hoeven EJRJ, Mont’Alverne FJA, de Carvalho JJF, Lima FO, Dippel DWJ, et al. Endovascular Therapy for Stroke Due to Basilar-Artery Occlusion. N Engl J Med. 2021;384(20):1910-20. https://doi.org/gj38sv.
47.Logallo N, Novotny V, Assmus J, Kvistad CE, Alteheld L, Rønning OM, et al. Tenecteplase versus alteplase for management of acute ischaemic stroke (NOR-TEST): a phase 3, randomised, open-label, blinded endpoint trial. Lancet Neurol. 2017;16(10):781-8. https://doi.org/fgs3.
48.Campbell BCV, De Silva DA, Macleod MR, Coutts SB, Schwamm LH, Davis SM, et al. Ischaemic stroke. Nat Rev Dis Primers. 2019;5(1):70. https://doi.org/ggsdqm.
49.Pirau L, Lui F. Vertebrobasilar Insufficiency. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2022. [cited 2023 Jan 19]. Available from: https://bit.ly/3GLPoPK.
50.Schoen JC, Boysen MM, Warren CR, Chakravarthy B, Lotfipour S. Vertebrobasilar artery occlusion. West J Emerg Med. 2011 [cited 2023 Jan 19];12(2):233-9. Available from: https://bit.ly/3J2vXVI.
51.Sparaco M. Basilar Artery Occlusion: Clinical management and Therapy. Clin Manag Issues. 2018;12(1):67-76. https://doi.org/js8t.
References
References
Kaye V, Brandstater ME, Talavera F, Salcido R, Kishner S, Klein MJ. Vertebrobasilar Stroke. Medscape; 2020. [cited 2021 Apr 28]. Available from: https://bit.ly/3weOgzd.
Khazaal O, Marquez DL, Naqvi IA. Foville Syndrome. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2020. [cited 2021 Apr 28]. Available from: https://bit.ly/3J5hGYa.
Beucler N, Boissonneau S, Ruf A, Fuentes S, Carron R, Dufour H. Crossed brainstem syndrome revealing bleeding brainstem cavernous malformation: an illustrative case. BMC Neurol. 2021;21(1):204. https://doi.org/js69. DOI: https://doi.org/10.1186/s12883-021-02223-7
Demel LS, Broderick PJ. Basilar Occlusion Syndromes: An Update. The Neurohospitalist. 2015;5(3):142-50. https://doi.org/js7b. DOI: https://doi.org/10.1177/1941874415583847
Selvadurai C, Rondeau MW, Colorado RA, Feske SK, Prasad S. Teaching Video NeuroImages: Foville syndrome. Neurology. 2016;86(19):e203. https://doi.org/gmmhs7. DOI: https://doi.org/10.1212/WNL.0000000000002658
Man BL, Fu YP. Bronchogenic carcinoma presented as Foville's syndrome. BMJ Case Rep. 2015;2015:bcr2014205025. https://doi.org/js7j. DOI: https://doi.org/10.1136/bcr-2014-205025
Stephen M, Jayasri, Harigaravelu PJ, Baranitharan. Pontine hemorrhage presenting as Foville’s syndrome. IJAM. 2021;8(8):1226-8. https://doi.org/js7k. DOI: https://doi.org/10.18203/2349-3933.ijam20212873
Hubloue I, Laureys S, Michotte A. A rare case of diplopia: medial inferior pontine syndrome or Foville's syndrome. Eur J Emerg Med. 1996;3(3):194-8. https://doi.org/bnzpqj. DOI: https://doi.org/10.1097/00063110-199609000-00011
Massi DG, Nyassinde J, Ndiaye MM. Superior Foville syndrome due to pontine hemorrhage: a case report. Pan Afr Med J. 2016;25:215. https://doi.org/js7q. DOI: https://doi.org/10.11604/pamj.2016.25.215.10648
Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. Guidelines for the Early Management of Patients With Acute Ischemic Stroke: 2019 Update to the 2018 Guidelines for the Early Management of Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 2019;50(12):e344-e418. https://doi.org/dnbv. DOI: https://doi.org/10.1161/STR.0000000000000211
Winstein CJ, Stein J, Arena R, Bates B, Cherney LR, Cramer SC, et al. Guidelines for Adult Stroke Rehabilitation and Recovery: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 2016;47(6):e98-e169. https://doi.org/gsm7. DOI: https://doi.org/10.1161/STR.0000000000000098
Salerno A, Strambo D, Nannoni S, Dunet V, Michel P. Patterns of ischemic posterior circulation strokes: A clinical, anatomical, and radiological review. Int J Stroke. 2022;17(7):714-22. https://doi.org/js7v. DOI: https://doi.org/10.1177/17474930211046758
Jenkins JS, Stewart M. Endovascular Treatment of Vertebral Artery Stenosis. Prog Cardiovasc Dis. 2017;59(6):619-25. https://doi.org/gbngbd. DOI: https://doi.org/10.1016/j.pcad.2017.02.005
Piccinin MA, Munakomi. S. Neuroanatomy, Vertebrobasilar System. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2022. [cited 2023 Jan 19]. Available from: https://bit.ly/3IWyMYh.
Alwood BT, Dossani RH. Vertebrobasilar Stroke. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2022. [cited 2023 Jan 19]. Available from: https://bit.ly/3Wn981J.
Markus HS, van der Worp HB, Rothwell PM. Posterior circulation ischaemic stroke and transient ischaemic attack: diagnosis, investigation, and secondary prevention. Lancet Neurol. 2013;12(10):989-98. https://doi.org/f2fnrd. DOI: https://doi.org/10.1016/S1474-4422(13)70211-4
Langhorne P, Stott DJ, Robertson L, MacDonald J, Jones L, McAlpine C, et al. Medical complications after stroke: a multicenter study. Stroke. 2000;31(6):1223-9. https://doi.org/b78b8x. DOI: https://doi.org/10.1161/01.STR.31.6.1223
Cheng H-C, Yen M-Y, Wang A-G. Foville’s syndrome with ipsilateral internuclear ophthalmoplegia due to spontaneous pontine hemorrhage. Taiwan J Ophthalmol. 2013;3(2):75-7. https://doi.org/js74. DOI: https://doi.org/10.1016/j.tjo.2012.12.001
Ferbert A, Brückmann H, Drummen R. Clinical features of proven basilar artery occlusion. Stroke. 1990;21(8):1135-42. https://doi.org/fh3vwj. DOI: https://doi.org/10.1161/01.STR.21.8.1135
Yebra González L, González Márquez R, Rueda Marcos A, Salas Álvarez FJ, Sanz Fernández R, Martín Sanz E. Unclear origin vertigo protocol. Acta Otorrinolaringol (Engl Ed). 2021;72(2):92-100. https://doi.org/js75. DOI: https://doi.org/10.1016/j.otoeng.2020.02.008
Kattah JC. Use of HINTS in the acute vestibular syndrome. An Overview. Stroke Vasc Neurol. 2018;3(4):190-6. https://doi.org/gf5dwb. DOI: https://doi.org/10.1136/svn-2018-000160
Sankalia D, Kothari S, Phalgune DS. Diagnosing Stroke in Acute Vertigo: Sensitivity and Specificity of HINTS Battery in Indian Population. Neurol India. 2021;69(1):97-101. https://doi.org/js76. DOI: https://doi.org/10.4103/0028-3886.310089
Baran G, Gultekin TO, Baran O, Deniz C, Katar S, Yildiz GB, et al. Association between etiology and lesion site in ischemic brainstem infarcts: a retrospective observational study. Neuropsychiatr Dis Treat. 2018;14:757-66. https://doi.org/gc73m7. DOI: https://doi.org/10.2147/NDT.S154224
Boehme AK, Esenwa C, Elkind MSV. Stroke Risk Factors, Genetics, and Prevention. Circ Res. 2017;120(3):472-95. https://doi.org/f9tt4f. DOI: https://doi.org/10.1161/CIRCRESAHA.116.308398
Shi Y, Wardlaw JM. Update on cerebral small vessel disease: a dynamic whole-brain disease. Stroke Vasc Neurol. 2016;1(3):83-92. https://doi.org/gbzw3s. DOI: https://doi.org/10.1136/svn-2016-000035
Samaniego EA, Shaban A, Ortega-Gutierrez S, Roa JA, Hasan DM, Derdeyn C, et al. Stroke mechanisms and outcomes of isolated symptomatic basilar artery stenosis. Stroke Vasc Neurol. 2019;4(4):189-97. https://doi.org/gk8krz. DOI: https://doi.org/10.1136/svn-2019-000246
Savitz SI, Caplan LR. Vertebrobasilar disease. N Engl J Med. 2005;352(25):2618-26. https://doi.org/b2w49z. DOI: https://doi.org/10.1056/NEJMra041544
Arauz A, Ruíz-Franco A. Enfermedad vascular cerebral. Rev Fac Med (Méx.). 2012 [cited 2023 Jan 19];55(3):11-21. Available from: https://bit.ly/2HHx5Oe.
Huang R, Zhang X, Chen W, Lin J, Chai Z, Yi X. Stroke Subtypes and Topographic Locations Associated with Neurological Deterioration in Acute Isolated Pontine Infarction. J Stroke Cerebrovasc Dis. 2016;25(1):206-13. https://doi.org/js8g. DOI: https://doi.org/10.1016/j.jstrokecerebrovasdis.2015.09.019
Hui C, Tadi P, Patti L. Ischemic Stroke. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2022. [cited 2023 Jan 19]. Available from: https://bit.ly/3wji1z4.
Lima Neto AC, Bittar R, Gattas GS, Bor-Seng-Shu E, Oliveira M, Monsanto R, et al. Pathophysiology and Diagnosis of Vertebrobasilar Insufficiency: A Review of the Literature. Int Arch Otorhinolaryngol. 2017;21(3):302-7. https://doi.org/js8h. DOI: https://doi.org/10.1055/s-0036-1593448
Ng CF, Chong CY. Acute Basilar Artery Occlusion: Early Computed Tomography Finding Predicts Catastrophic Outcome. J Neurosci Rural Pract. 2018;9(4):653-4. https://doi.org/js8k. DOI: https://doi.org/10.4103/jnrp.jnrp_40_18
Reinemeyer NE, Tadi P, Lui F. Basilar Artery Thrombosis. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2022. [cited 2023 Jan 19] Available from: https://bit.ly/3GLMASI.
Garg R, Biller J. Neuroimaging Predictors of Clinical Outcome in Acute Basilar Artery Occlusion. Front Neurol. 2017;8:293. https://doi.org/gf6ckz. DOI: https://doi.org/10.3389/fneur.2017.00293
Pallesen L-P, Lambrou D, Eskandari A, Barlinn J, Barlinn K, Reichmann H, et al. Perfusion computed tomography in posterior circulation stroke: predictors and prognostic implications of focal hypoperfusion. Eur J Neurol. 2018;25(5):725-31. https://doi.org/js8m. DOI: https://doi.org/10.1111/ene.13578
Caruso P, Ridolfi M, Lugnan C, Ajčević M, Furlanis G, Bellavita G, et al. Multimodal CT pc-ASPECTS in infratentorial stroke: diagnostic and prognostic value. Neurol Sci. 2021;42(10):4231-40. https://doi.org/js8n. DOI: https://doi.org/10.1007/s10072-021-05072-x
Lin S-F, Chen C-I, Hu H-H, Bai C-H. Predicting functional outcomes of posterior circulation acute ischemic stroke in first 36 h of stroke onset. J Neurol. 2018;265(4):926-32. https://doi.org/gdcsxw. DOI: https://doi.org/10.1007/s00415-018-8746-6
Kim JG, Lee D, Choi JC, Song Y, Lee DH, Suh DC. DWI-pc-ASPECT score in basilar artery occlusion: is 6 points or less always indicative of a bad outcome? Interv Neuroradiol. 2019;25(4):371-9. https://doi.org/js8p. DOI: https://doi.org/10.1177/1591019919827505
Hoyer C, Szabo K. Pitfalls in the Diagnosis of Posterior Circulation Stroke in the Emergency Setting. Front Neurol. 2021;12:682827. https://doi.org/js8q. DOI: https://doi.org/10.3389/fneur.2021.682827
Tehrani ASS, Kattah JC, Mantokouis G, Pula JH, Nair D, Blitz A, et al. Small strokes causing severe vertigo: frequency of false-negative MRIs and nonlacunar mechanisms. Neurology. 2014;83(2):169-73. https://doi.org/f6cnfh. DOI: https://doi.org/10.1212/WNL.0000000000000573
Bulut HT, Yildirim A, Ekmekci B, Eskut N, Gunbey HP. False-negative diffusion-weighted imaging in acute stroke and its frequency in anterior and posterior circulation ischemia. J Comput Assist Tomogr. 2014;38(5):267-33. https://doi.org/f6j4bm. DOI: https://doi.org/10.1097/RCT.0000000000000095
Simonsen CZ, Madsen MH, Schmitz ML, Mikkelsen IK, Fisher M, Andersen G. Sensitivity of diffusion- and perfusion-weighted imaging for diagnosing acute ischemic stroke is 97.5%. Stroke. 2015;46(1):98-101. https://doi.org/f6v59j. DOI: https://doi.org/10.1161/STROKEAHA.114.007107
Brunser AM, Lavados PM, Cavada G, Muñoz-Venturelli P, Olavarría VM, Navia V, et al. Transcranial Doppler as a Predictor of Ischemic Events in Vertebral Artery Dissection. J Neuroimaging. 2020;30(6):890-5. https://doi.org/js8r. DOI: https://doi.org/10.1111/jon.12773
Weber R, Minnerup J, Nordmeyer H, Eyding J, Krogias C, Hadisurya J, et al. Thrombectomy in posterior circulation stroke: differences in procedures and outcome compared to anterior circulation stroke in the prospective multicentre REVASK registry. Eur J Neurol. 2019;26(2):299-305. https://doi.org/gfftqk. DOI: https://doi.org/10.1111/ene.13809
Nguyen TN, Strbian D. Endovascular Therapy for Stroke due to Basilar Artery Occlusion: A BASIC Challenge at BEST. Stroke. 2021;52(10):3410-3. https://doi.org/js8s. DOI: https://doi.org/10.1161/STROKEAHA.121.035948
Langezaal LCM, van der Hoeven EJRJ, Mont'Alverne FJA, de Carvalho JJF, Lima FO, Dippel DWJ, et al. Endovascular Therapy for Stroke Due to Basilar-Artery Occlusion. N Engl J Med. 2021;384(20):1910-20. https://doi.org/gj38sv.
Logallo N, Novotny V, Assmus J, Kvistad CE, Alteheld L, Rønning OM, et al. Tenecteplase versus alteplase for management of acute ischaemic stroke (NOR-TEST): a phase 3, randomised, open-label, blinded endpoint trial. Lancet Neurol. 2017;16(10):781-8. https://doi.org/fgs3. DOI: https://doi.org/10.1016/S1474-4422(17)30253-3
Campbell BCV, De Silva DA, Macleod MR, Coutts SB, Schwamm LH, Davis SM, et al. Ischaemic stroke. Nat Rev Dis Primers. 2019;5(1):70. https://doi.org/ggsdqm. DOI: https://doi.org/10.1038/s41572-019-0118-8
Pirau L, Lui F. Vertebrobasilar Insufficiency. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2022. [cited 2023 Jan 19]. Available from: https://bit.ly/3GLPoPK.
Schoen JC, Boysen MM, Warren CR, Chakravarthy B, Lotfipour S. Vertebrobasilar artery occlusion. West J Emerg Med. 2011 [cited 2023 Jan 19];12(2):233-9. Available from: https://bit.ly/3J2vXVI.
Sparaco M. Basilar Artery Occlusion: Clinical management and Therapy. Clin Manag Issues. 2018;12(1):67-76. https://doi.org/js8t. DOI: https://doi.org/10.7175/cmi.v12i1.1363
How to Cite
APA
ACM
ACS
ABNT
Chicago
Harvard
IEEE
MLA
Turabian
Vancouver
Download Citation
License

This work is licensed under a Creative Commons Attribution 4.0 International License.
The authors, when submitting their manuscripts, accept to transfer to Case reports the copyright of the published articles. The publisher has the right of use, reproduction, transmission, distribution and publication in any form or medium. The authors cannot allow or authorize the use of the contribution without the written consent of the journal.
Uniform Disclosure Form for possible Conflicts of Interest, the assignment of rights and responsibility must be delivered together with the original.
Those authors who have publications with this journal accept the following terms:
The authors will keep their copyright and guarantee the journal the right of first publication of their work, which will be simultaneously subject to the Creative Commons Recognition License that allows third parties to share the work whenever its author is indicated and his first publication this journal
The authors may adopt other non-exclusive licensing agreements for the distribution of the published version of the work (eg, deposit it in an institutional telematic file or publish it in a monographic volume) whenever the initial publication in this journal is indicated.
Authors are allowed and advised to disseminate their work through the Internet (eg in institutional telematic files or on their website) before and during the submission process, which can produce interesting exchanges and increase citations of the published work. (See The effect of open access).