Seudotumor ureteral por enfermedad relacionada con IgG4. Reporte de caso
IgG4-related inflammatory pseudotumor of the ureter: Case report
DOI:
https://doi.org/10.15446/cr.v9n1.95562Keywords:
Informes de casos, Enfermedad relacionada con inmunoglobulina G4, Enfermedades ureterales (es)Case Reports, Immunoglobulin G4-Related Disease, Ureteral Diseases (en)
Resumen
Introducción. La enfermedad relacionada con inmunoglobulina G4 (IgG4-RD, por sus siglas en inglés) es una condición poco común que causa lesiones fibroinflamatorias en casi cualquier órgano y se caracteriza histológicamente por un infiltrado linfoplasmocitario asociado a fibrosis y células plasmáticas con marcador positivo para inmunoglobulina G4 (IgG4). En casos de IgG4-RD la afectación del tracto urinario es inusual y puede imitar una patología oncológica. El manejo de esta enfermedad se basa en glucocorticoides e inmunomoduladores, requiriendo manejo quirúrgico en algunos casos.
Presentación del caso. Mujer de 55 años con dolor lumbar, infección urinaria e hidronefrosis. El estudio radiológico evidenció una masa en el tercio distal del uréter izquierdo. Se realizó una ureterectomía con estudio histopatológico que confirmó un seudotumor ureteral por IgG4-RD.
Conclusiones. La IgG4-RD es una condición inusual, más aún con manifestaciones urológicas, por lo que es importante incluirla en el diagnóstico diferencial de tumores ureterales, ya que puede simular características clínicas e imagenológicas de una patología neoplásica con desenlaces adversos.
Abstract
Introduction: Immunoglobulin G4-related disease (IgG4-RD) is a rare condition that causes fibroinflammatory lesions in almost any organ. It is characterized histologically by lymphoplasmacytic infiltrates with fibrosis and IgG4-positive plasma cells. Urinary tract involvement is uncommon and may mimic an oncologic disease. Treatment is based on glucocorticoids and immunomodulators, with surgical interventions required in selected cases.
Case presentation: A 55-year-old woman who presented with lumbar pain, urinary tract infection, and hydronephrosis. Radiologic study showed a mass located in the left distal ureter. Ureterectomy was required, confirming a histologically IgG4-related inflammatory pseudotumor of the ureter.
Conclusion: IgG4-related disease is a relatively rare condition, and urogenital manifestations are even less common. It is important to include this condition within the differential diagnosis of ureteral tumors, considering that it has clinical and radiologic features that may mimic ureteral neoplasm.
https://doi.org/10.15446/cr.v9n1.95562
IgG4-related inflammatory pseudotumor of the ureter: Case report
Keywords: Case Reports; Immunoglobulin G4-Related Disease; Ureteral Diseases.
Palabras clave: Informes de casos; Enfermedad relacionada con inmunoglobulina G4; Enfermedades ureterales.
Manuel Duque-Galán
Fundación Valle del Lili - Urology Service -
Cali - Colombia.
Paola Andrea Orrego-Rojas
Universidad Militar Nueva Granada -
Faculty of Medicine - Department of Urology - Bogotá - Colombia.
Carlos Andrés Jiménez-Guerrero
Fundación Valle del Lili - Pathology Service - Cali - Colombia.
Andrés Augusto González-Arboleda
Universidad Icesi - Faculty of Health Sciences - Cali - Colombia.
Corresponding author
Andrés Augusto González-Arboleda. Universidad Icesi, Facultad Ciencias de la Salud. Cali. Colombia. Email: andresaugusto97@hotmail.com
Received: 06/05/2021 Accepted: 16/07/2021
Resumen
Introducción. La enfermedad relacionada con inmunoglobulina G4 (IgG4-RD, por sus siglas en inglés) es una condición poco común que causa lesiones fibroinflamatorias en casi cualquier órgano y se caracteriza histológicamente por un infiltrado linfoplasmocitario asociado a fibrosis y células plasmáticas con marcador positivo para inmunoglobulina G4 (IgG4). En casos de IgG4-RD la afectación del tracto urinario es inusual y puede imitar una patología oncológica. El manejo de esta enfermedad se basa en glucocorticoides e inmunomoduladores, requiriendo manejo quirúrgico en algunos casos.
Presentación del caso. Mujer de 55 años con dolor lumbar, infección urinaria e hidronefrosis. El estudio radiológico evidenció una masa en el tercio distal del uréter izquierdo. Se realizó una ureterectomía con estudio histopatológico que confirmó un seudotumor ureteral por IgG4-RD.
Conclusiones. La IgG4-RD es una condición inusual, más aún con manifestaciones urológicas, por lo que es importante incluirla en el diagnóstico diferencial de tumores ureterales, ya que puede simular características clínicas e imagenológicas de una patología neoplásica con desenlaces adversos.
Abstract
Introduction: Immunoglobulin G4-related disease (IgG4-RD) is a rare condition that causes fibroinflammatory lesions in almost any organ. It is characterized histologically by lymphoplasmacytic infiltrates with fibrosis and IgG4-positive plasma cells. Urinary tract involvement is uncommon and may mimic an oncologic disease. Treatment is based on glucocorticoids and immunomodulators, with surgical interventions required in selected cases.
Case presentation: A 55-year-old woman who presented with lumbar pain, urinary tract infection, and hydronephrosis. Radiologic study showed a mass located in the left distal ureter. Ureterectomy was required, confirming a histologically IgG4-related inflammatory pseudotumor of the ureter.
Conclusion: IgG4-related disease is a relatively rare condition, and urogenital manifestations are even less common. It is important to include this condition within the differential diagnosis of ureteral tumors, considering that it has clinical and radiologic features that may mimic ureteral neoplasm.
Introduction
Immunoglobulin G4-related disease (IgG4-RD) is a rare immune-mediated condition that can cause fibroinflammatory lesions in almost any organ (1). This condition was first identified in patients with autoimmune pancreatitis (2,3) and, although its etiology has not been fully elucidated, there are clinical and pathological features that make it a systemic disorder (2,3). Such characteristics comprise multiple organ and system involvement (pancreas, hepatobiliary and genitourinary systems, salivary glands, etc.), elevated serum immunoglobulin G4 (IgG4) levels, dense lymphoplasmacytic infiltrate, storiform fibrosis, obliterative phlebitis, and an IgG4/IgG ratio >40%, with the latter 4 being typical histopathologic features of IgG4-RD (4-6). The onset of the lesions can take months or years, and clinical symptoms vary depending on the organ involved (5).
In order to establish a histopathological diagnosis, 2 or more of the following features must be observed: dense lymphoplasmacytic infiltrate, storiform fibrosis pattern, obliterative phlebitis, and an IgG4/IgG ratio >40% (6). Multifocal involvement, as described by Bledsoe et al. (4), has been reported in 31-62% of cases. These authors also concluded that, bearing in mind the low incidence of this condition, the differential diagnosis should include neoplasms, infections, and other inflammatory disorders (4).
The prevalence of IgG4-RD is still unclear and may be underestimated because of the few cases reported to date. However, Uchida and colleagues [cited by Bledsoe et al. (4) and Floreani et al. (7)], in a nationwide survey conducted in 2009 in Ishikawa, Japan, reported an incidence of 0.28 to 1.08 cases per 100 000 people, affecting mostly males.
Other inflammatory conditions are encompassed in the IgG4-RD spectrum, such as dacryoadenitis, chronic sclerosing sialadenitis, chronic thyroiditis, orbital pseudotumor, pulmonary inflammatory pseudotumor, mediastinal fibrosis, retroperitoneal fibrosis, among others. These are conditions that share pathologic and immunologic features with IgG4-RD (8).
According to Carrillo-Córdova et al. (9), up to 30% of IgG4-RD cases resolve spontaneously, and a similar percentage of cases is refractory or relapses. These authors also state that the first-line treatment is the administration of corticosteroids at low doses, but other drugs used for autoimmune diseases (rituximab, methotrexate, or azathioprine) may be considered for patients in whom steroid therapy fails or relapses occur (9).
Case presentation
A 55-year-old housewife from Cali, Colombia, who was referred by the general urology service to the urologic oncology outpatient clinic of the Fundación Valle del Lili, a quaternary care center in Cali. At the time of consultation, the patient reported no surgical or pharmacological history, but stated that over the last year she had presented moderate intermittent colicky pain in the left lumbar region accompanied by dysuria and increased frequency of urination, and that this pain had worsened in the last two months. Physical examination revealed no alterations.
The patient brought a renal and urinary tract ultrasound (performed two months earlier) that showed hydronephrosis in the left kidney and an image suggestive of a mass in the left ureter. Moreover, on that occasion, the patient reported a urine culture positive for Escherichia coli with an ampicillin resistance pattern, prompting the administration of an outpatient antibiotic treatment with ciprofloxacin 250mg every 12 hours for 7 days.
One month before the urologic oncology visit, she was evaluated by the urology service of another institution. At that time, she underwent ureteroscopy and urinary diversion with a double J stent in the left kidney, but the patient did not submit an adequate report of the findings of these procedures. Two weeks after the double J stent urinary diversion procedure, the patient underwent an abdominal MRI which showed a mass in the left distal ureter where the double J stent had been placed. This mass was obstructing the lumen of the ureter and extended into the fundus of the rectovaginal pouch.
In view of these findings, transitional cell carcinoma (TCC) with invasion of adjacent structures was considered as the first diagnostic possibility. Five months after being evaluated by the urologic oncology service, the patient underwent a distal ureterectomy and left ureterovesical reimplantation. Macroscopically, there was evidence of a hard mass in the distal ureter with marked adhesion to the uterus and vagina, and infiltration of adjacent structures.
Histopathologic studies of the excised tissue were performed within the first 3 postoperative weeks, and the pathology report revealed the presence of marked stromal fibrosis with abundant lymphoplasmacytic inflammatory infiltrate. Immunostaining was performed in the same histopathological study, revealing that plasma cells were reactive for CD38 with polytypic expression of kappa and lambda chains. Staining for IgG4 was positive in more than 10 plasma cells with a ratio of IgG4+/IgG+ cells >40% (Figures 1 and 2).
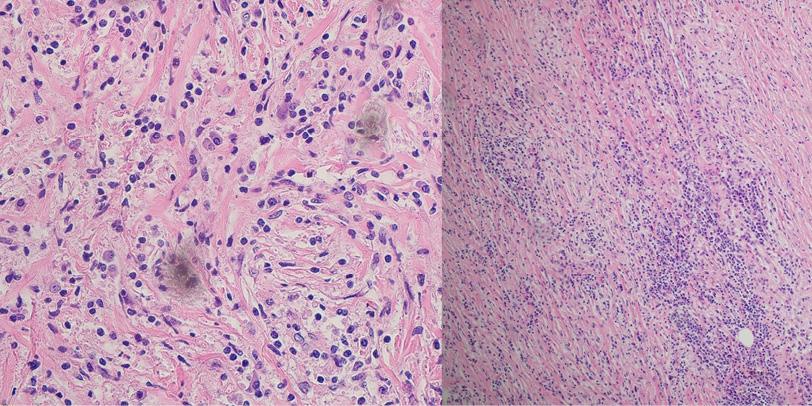
Figure 1. Lymphoplasmacytic infiltrate associated with stromal fibrosis.
Source: Image obtained during the study.
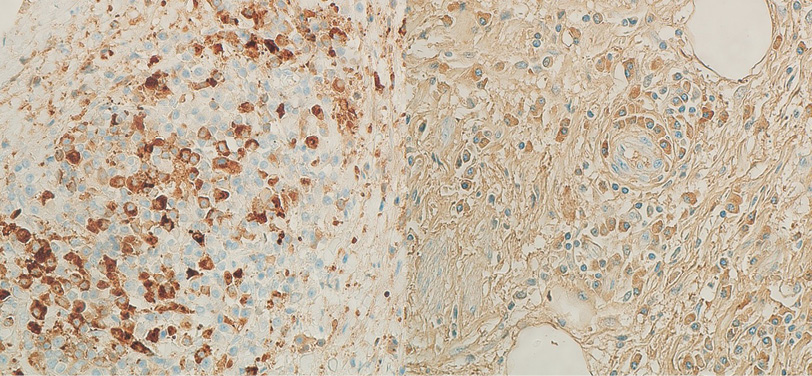
Figure 2. Plasma cells with IgG4/IgG ratio >40%.
Source: Imagen obtained during the study.
The patient was admitted to the hospital for postoperative follow-up, and since there were no complications, she was discharged the following day. One month later, she attended a follow-up visit reporting urinary incontinence and urine leakage through the vagina, so a cystoscopy and a pelvic computed axial tomography (CT) scan were performed two weeks later, showing no recurrence of the lesion, but evidencing a vesicovaginal fistula communicating the vagina with the bladder.
Two months after the procedure, a successful transurethral closure of the vesicovaginal fistula was performed and, although the most common approach to repair vesicovaginal fistula is the transvaginal approach, transurethral closure was preferred because it had been previously performed at the institution with good results.
Follow-up was carried out with cystoscopy and pelvic CT scan, both taken 6 and 12 months after the initial surgical procedure, and no recurrence of the ureteral lesion or vesicovaginal fistula was evidenced on any occasion. The patient did not receive pharmacological treatment since the surgical resection of the lesion was complete.
Discussion
IgG4-RD is a rare disease in medical practice and is not considered as a first diagnostic possibility when masses are detected in different tissues. However, it should be noted that it can mimic many inflammatory or oncologic disorders in different organs.
There are some genetic factors that increase the production of inflammatory cytokines and the susceptibility to develop IgG4-RD (6). There are also theories that suggest that there is homology between bacterial antigens and human proteins that leads to increased IgG4 production in people predisposed to the disease. However, although autoantigens are recognized as a possible initial immune stimulus, this has not been fully elucidated (8).
IgG4 is the least abundant antibody in the immunoglobulin G family (8). Its molecular constitution results in a limited role in the activation of the immune response. Nevertheless, interaction with other IgG4 molecules may contribute to its anti-inflammatory role, which is controlled by the Th2 lymphocyte response. Cytokine production can cause an increase in eosinophil and immunoglobulin E (IgE) levels, characteristics reported in some patients with IgG4-RD, as well as activation of regulatory T lymphocytes (8,10).
Regulatory T lymphocytes increase the production of interleukin-10 and transforming growth factor beta, which are anti-inflammatory cytokines that play an important role in the formation of fibrosis in the affected tissue. In this context, it has been suggested that the increase in IgG4 levels is a counter-regulatory response to a primary inflammatory process. Nonetheless, the actual role of IgG4 in the disease has not been fully identified (8,10).
Manifestations in the urinary tract are not the most common within the IgG4-RD spectrum; however, the most affected organ is the kidney. Other common urological manifestations are retroperitoneal fibrosis, urachal tumors, collecting duct carcinoma, prostatitis, and orchiepididymitis (9). The most representative kidney injury is tubulointerstitial nephritis, followed by masses in the parenchyma or renal pelvis, which can mimic an oncologic disorder (11). In this regard, Wang et al. (12) reported the case of a female patient with imaging findings of a tumor in the renal pelvis, in whom, based on histopathological findings after surgical resection, a lesion resulting from IgG4-RD that mimicked an oncologic disorder was confirmed. The manifestations of the patient reported here are similar to those described in four reports found in the literature (13-16).
There are no clinical or imaging features to differentiate IgG4-RD from other neoplastic or inflammatory diseases of the ureter. In this sense, considering the prognostic implications of a transitional cell carcinoma, the diagnostic and therapeutic approach will aim to rule out and treat a possible neoplasm, while surgical management will be essential for histological confirmation, and the extent of the procedure will depend on the location of the mass. Regarding the type of intervention, several procedures have been reported, ranging from radical nephroureterectomy to segmental ureterectomy with ureteral reimplantation, such as the one performed on the patient in the case reported here (13-16).
In the diagnostic approach to IgG4-RD, the results of some laboratory studies have been taken into account, such as elevated IgG4 blood levels, which have a sensitivity of 90% and a specificity of 60%, but a positive predictive value of only 34% (17). In addition, up to half of histologically confirmed cases may have normal blood IgG4 levels (18). Activity of complement proteins in blood (hypocomplementemia), resulting in more severe immune activity, is observed in only 25% of cases, but is more frequently seen when there is renal involvement. However, according to the pathophysiology and immune function of IgG4, the ability to activate complement is low, and in these patients other elevated IgG subunits that may explain complement activity are observed (8,19). On the other hand, elevated IgE levels have been reported in 35% of patients, while eosinophilia is described in 27% of cases (20).
When involvement is observed in commonly affected organs (pancreas, salivary glands, lung or kidney), IgG4-RD is more likely to be included as a differential diagnosis; in addition, the diagnostic approach can be broadened by measuring IgG4 levels, serum complement and IgE levels, which, needless to say, were not assessed in the reported patient. In organs that are not usually involved, such as the ureter, the priority is to exclude an oncologic disorder and surgical management takes on greater importance. Likewise, laboratory studies can vary considerably in cases of IgG4-RD, so histopathological study is the gold standard in the diagnosis of this disease (21).
In 2019, a classification system was proposed taking into account inclusion and exclusion criteria to confirm the diagnosis of IgG4-RD. In cases with no clinical manifestations in the commonly affected organs and no laboratory findings, histological features are sufficient to confirm the diagnosis, as in the reported case (22).
According to the literature review conducted for the preparation of this case report, there are no randomized trials evaluating the treatment of this disease; however, observational studies and expert recommendations propose glucocorticoids as the first line of treatment, with an efficacy of >90%, but with relapses in up to 33% of cases (21,23). In cases that do not respond to initial treatment or with multiple organ involvement, other immunomodulators such as azathioprine, methotrexate or rituximab can be considered (24).
These pharmacological treatments are widely described with acceptable results in residual lesions in cases in which the histopathological diagnosis has been confirmed by biopsy. There are some specific cases requiring surgical management or other mechanical interventions; for example, if hydronephrosis is present, as in the reported case, urinary diversion with a double J stent or nephrostomy may be required (25,26). It should be noted that the lesion was completely excised in the present case, so no glucocorticoids or immunomodulators were used to treat the lesion. No relapses occurred during the 12-month follow-up, suggesting that complete resection of the lesion may be the only management required, as long as the location allows a complete surgical procedure, and no new lesions are present.
Conclusions
IgG4-RD is a relatively rare disease, and urologic manifestations are uncommon.
Since it can involve almost any organ and has a wide range of manifestations, IgG4-RD has become a systemic disease with the capacity to mimic other etiologies, so it is important to include it in the differential diagnosis of unusual presentations of hydronephrosis or ureteral tumors, as in the reported case. Surgical management continues to play an important role in the treatment of this disease when the collecting duct system is involved, given that it is imperative to rule out an oncologic disease.
Ethical considerations
The patient’s informed consent was obtained for the preparation of this case report.
Conflict of interest
None stated by the authors.
Funding
None stated by the authors.
Acknowledgments
None stated by the authors.
References
1.Wallace ZS, Perugino C, Matza M, Deshpande V, Sharma A, Stone JH. Immunoglobulin G4-related Disease. Clin Chest Med. 2019;40(3):583-97. https://doi.org/gg5spk.
2.Deshpande V, Zen Y, Chan JK, Yi EE, Sato Y, Yoshino T, et al. Consensus statement on the pathology of IgG4-related disease. Mod Pathol. 2012;25(9):1181-92. https://doi.org/ggqzsj.
3.Tan TJ, Ng YL, Tan D, Fong WS, Low ASC. Extrapancreatic findings of IgG4-related disease. Clin Radiol. 2014;69(2):209-18. https://doi.org/f5qmvd.
4.Bledsoe JR, Della-Torre E, Rovati L, Deshpande V. IgG4-related disease: review of the histopathologic features, differential diagnosis, and therapeutic approach. Apmis. 2018;126(6):459-76. https://doi.org/gg5spg.
5.Perugino CA, Stone JH. IgG4-related disease: an update on pathophysiology and implications for clinical care. Nat Rev Rheumatol. 2020;16(12):702-14. https://doi.org/gjgzrt.
6.Kubo K, Yamamoto K. IgG4-related disease. Int J Rheum Dis. 2015;19(8):747-62. https://doi.org/gg5sph.
7.Floreani A, Okazaki K, Uchida K, Gershwin ME. IgG4-related disease: Changing epidemiology and new thoughts on a multisystem disease. J Transl Autoimmun. 2021;4:100074. https://doi.org/jzcx.
8.Stone JH, Zen Y, Deshpande V. IgG4-Related Disease. N Engl J Med. 2012;366(6):539-51. https://doi.org/gfvpcq.
9.Carrillo-Córdova LD, Carrillo-Córdova CA, Vitar-Sandoval J, Jaspersen-Álvarez J, Villena-López EL, Carrillo-Esper R. Manifestaciones urológicas de la enfermedad relacionada con la inmunoglobulina G4 Cir Cir. 2018;86(1):63-70. https://doi.org/jzc3.
10.Zen Y, Fujii T, Harada K, Kawano M, Yamada K, Takahira M, et al. Th2 and Regulatory Immune Reactions Are Increased in Immunoglobin G4-Related Sclerosing Pancreatitis and Cholangitis. Hepatology. 2007;45(6):1538-46. https://doi.org/bpmxqk.
11.Kawano M, Saeki T, Nakashima H. IgG4-related kidney disease and retroperitoneal fibrosis: An update. Mod Rheumatol. 2019;29(2):231-9. https://doi.org/gq3z62.
12.Wang Y, Chen X, Luo R, Wang H, Wang G, Hou Y, et al. IgG4-related systemic disease mimicking renal pelvic cancer: A rare case. World J Surg Oncol. 2014;12(1):395. https://doi.org/f6z5bq.
13.Kim SA, Lee SR, Huh J, Shen SS, Ro JY. IgG4-associated inflammatory pseudotumor of ureter: Clinicopathologic and immunohistochemical study of 3 cases. Hum Pathol. 2011;42(8):1178-84. https://doi.org/cj53tt.
14.Marando A, D’Ambrosio G, Catanzaro F, La Rosa S, Sessa F. IgG4-related disease of the ureter: Report of two cases and review of the literature. Virchows Arch. 2013;462(6):673-8. https://doi.org/f4223k.
15.Lei WH, Xin J, Shao CX, Mao MF, Zhu CY, Wu CF, et al. IgG4-related kidney disease mimicking malignant ureter tumor: Case report and literature review. Medicine. 2016;95(3):e2550.
https://doi.org/jzc6.
16.Ueki T, Miyake T, Narita M, Kojima M, Kaida S, Iida H, et al. IgG4-related focal retroperitoneal fibrosis in ureter suggestive of colon cancer recurrence and resected laparoscopically: a case report. Surg Case Reports. 2020;6(1):197. https://doi.org/jzc7.
17.Carruthers MN, Khosroshahi A, Augustin T, Deshpande V, Stone JH. The diagnostic utility of serum IgG4 concentrations in IgG4-related disease. Ann Rheum Dis. 2015;74(1):14-8. https://doi.org/f6shdc.
18.Karadeniz H, Vaglio A. Igg4-related disease: a contemporary review. Turkish J Med Sci. 2020;50(2):1616-31. https://doi.org/jzc8.
19.Wallace ZS, Deshpande V, Mattoo H, Mahajan VS, Kulikova M, Pillai S, et al. IgG4-Related Disease: Clinical and Laboratory Features in One Hundred Twenty-Five Patients. Arthritis Rheumatol. 2015;67(9):2466-75. https://doi.org/gg5sfk.
20.Della-Torre E, Mattoo H, Mahajan VS, Carruthers M, Pillai S, Stone JH. Prevalence of Atopy, Eosinophilia, and IgE Elevation in IgG4-Related Disease. Allergy. 2014;69(2):269-72. https://doi.org/f5qs6h.
21.Abraham M, Khosroshahi A. Diagnostic and Treatment Workup for IgG4-Related Disease. Expert Rev Clin Immunol. 2017;13(9):867-75. https://doi.org/gqp399.
22.Wallace ZS, Naden RP, Chari S, Choi HK, Della-Torre E, Dicaire JF, et al. The 2019 American College of Rheumatology/European League against Rheumatism classification criteria for IgG4-related disease. Arthritis Rheumatol. 2020;72(1):7-19. https://doi.org/ggmphc.
23.Brito-Zerón P, Kostov B, Bosch X, Acar-Denizli N, Ramos-Casals M, Stone JH. Therapeutic approach to IgG4-related disease: A systematic review. Medicine (Baltimore). 2016;95(26):e4002. https://doi.org/jzc9.
24.Martínez-Valle F, Orozco-Gálvez O, Fernández-Codina A. Update in ethiopathogeny, diagnosis and treatment of the IgG4 related disease. Med Clin (Barc). 2018;151(1):18-25. https://doi.org/jzdc.
25.Zhang W, Stone JH. Management of IgG4-related disease. Lancet Rheumatol. 2019;1(1):e55-65. https://doi.org/ggmphd.
26.Maritati F, Peyronel F, Vaglio A. IgG4-related disease: a clinical perspective. Rheumatology (Oxford). 2020;59(Suppl 3):iii123-31. https://doi.org/gq336f.
References
References
Wallace ZS, Perugino C, Matza M, Deshpande V, Sharma A, Stone JH. Immunoglobulin G4-related Disease. Clin Chest Med. 2019;40(3):583-97. https://doi.org/gg5spk. DOI: https://doi.org/10.1016/j.ccm.2019.05.005
Deshpande V, Zen Y, Chan JK, Yi EE, Sato Y, Yoshino T, et al. Consensus statement on the pathology of IgG4-related disease. Mod Pathol. 2012;25(9):1181-92. https://doi.org/ggqzsj. DOI: https://doi.org/10.1038/modpathol.2012.72
Tan TJ, Ng YL, Tan D, Fong WS, Low ASC. Extrapancreatic findings of IgG4-related disease. Clin Radiol. 2014;69(2):209-18. https://doi.org/f5qmvd. DOI: https://doi.org/10.1016/j.crad.2013.09.021
Bledsoe JR, Della-Torre E, Rovati L, Deshpande V. IgG4-related disease: review of the histopathologic features, differential diagnosis, and therapeutic approach. Apmis. 2018;126(6):459-76. https://doi.org/gg5spg. DOI: https://doi.org/10.1111/apm.12845
Perugino CA, Stone JH. IgG4-related disease: an update on pathophysiology and implications for clinical care. Nat Rev Rheumatol. 2020;16(12):702-14. https://doi.org/gjgzrt. DOI: https://doi.org/10.1038/s41584-020-0500-7
Kubo K, Yamamoto K. IgG4-related disease. Int J Rheum Dis. 2015;19(8):747-62. https://doi.org/gg5sph. DOI: https://doi.org/10.1111/1756-185X.12586
Floreani A, Okazaki K, Uchida K, Gershwin ME. IgG4-related disease: Changing epidemiology and new thoughts on a multisystem disease. J Transl Autoimmun. 2021;4:100074. https://doi.org/jzcx. DOI: https://doi.org/10.1016/j.jtauto.2020.100074
Stone JH, Zen Y, Deshpande V. IgG4-Related Disease. N Engl J Med. 2012;366(6):539-51. https://doi.org/gfvpcq. DOI: https://doi.org/10.1056/NEJMra1104650
Carrillo-Córdova LD, Carrillo-Córdova CA, Vitar-Sandoval J, Jaspersen-Álvarez J, Villena-López EL, Carrillo-Esper R. Manifestaciones urológicas de la enfermedad relacionada con la inmunoglobulina G4 Cir Cir. 2018;86(1):63-70. https://doi.org/jzc3. DOI: https://doi.org/10.24875/CIRU.M18000004
Zen Y, Fujii T, Harada K, Kawano M, Yamada K, Takahira M, et al. Th2 and Regulatory Immune Reactions Are Increased in Immunoglobin G4-Related Sclerosing Pancreatitis and Cholangitis. Hepatology. 2007;45(6):1538-46. https://doi.org/bpmxqk. DOI: https://doi.org/10.1002/hep.21697
Kawano M, Saeki T, Nakashima H. IgG4-related kidney disease and retroperitoneal fibrosis: An update. Mod Rheumatol. 2019;29(2):231-9. https://doi.org/gq3z62. DOI: https://doi.org/10.1080/14397595.2018.1554321
Wang Y, Chen X, Luo R, Wang H, Wang G, Hou Y, et al. IgG4-related systemic disease mimicking renal pelvic cancer: A rare case. World J Surg Oncol. 2014;12(1):395. https://doi.org/f6z5bq. DOI: https://doi.org/10.1186/1477-7819-12-395
Kim SA, Lee SR, Huh J, Shen SS, Ro JY. IgG4-associated inflammatory pseudotumor of ureter: Clinicopathologic and immunohistochemical study of 3 cases. Hum Pathol. 2011;42(8):1178-84. https://doi.org/cj53tt. DOI: https://doi.org/10.1016/j.humpath.2010.03.011
Marando A, D’Ambrosio G, Catanzaro F, La Rosa S, Sessa F. IgG4-related disease of the ureter: Report of two cases and review of the literature. Virchows Arch. 2013;462(6):673-8. https://doi.org/f4223k. DOI: https://doi.org/10.1007/s00428-013-1421-5
Lei WH, Xin J, Shao CX, Mao MF, Zhu CY, Wu CF, et al. IgG4-related kidney disease mimicking malignant ureter tumor: Case report and literature review. Medicine. 2016;95(3):e2550. https://doi.org/jzc6. DOI: https://doi.org/10.1097/MD.0000000000002550
Ueki T, Miyake T, Narita M, Kojima M, Kaida S, Iida H, et al. IgG4-related focal retroperitoneal fibrosis in ureter suggestive of colon cancer recurrence and resected laparoscopically: a case report. Surg Case Reports. 2020;6(1):197. https://doi.org/jzc7. DOI: https://doi.org/10.1186/s40792-020-00964-0
Carruthers MN, Khosroshahi A, Augustin T, Deshpande V, Stone JH. The diagnostic utility of serum IgG4 concentrations in IgG4-related disease. Ann Rheum Dis. 2015;74(1):14-8. https://doi.org/f6shdc. DOI: https://doi.org/10.1136/annrheumdis-2013-204907
Karadeniz H, Vaglio A. Igg4-related disease: a contemporary review. Turkish J Med Sci. 2020;50(2):1616-31. https://doi.org/jzc8. DOI: https://doi.org/10.3906/sag-2006-375
Wallace ZS, Deshpande V, Mattoo H, Mahajan VS, Kulikova M, Pillai S, et al. IgG4-Related Disease: Clinical and Laboratory Features in One Hundred Twenty-Five Patients. Arthritis Rheumatol. 2015;67(9):2466-75. https://doi.org/gg5sfk. DOI: https://doi.org/10.1002/art.39205
Della-Torre E, Mattoo H, Mahajan VS, Carruthers M, Pillai S, Stone JH. Prevalence of Atopy, Eosinophilia, and IgE Elevation in IgG4-Related Disease. Allergy. 2014;69(2):269-72. https://doi.org/f5qs6h. DOI: https://doi.org/10.1111/all.12320
Abraham M, Khosroshahi A. Diagnostic and Treatment Workup for IgG4-Related Disease. Expert Rev Clin Immunol. 2017;13(9):867-75. https://doi.org/gqp399. DOI: https://doi.org/10.1080/1744666X.2017.1354698
Wallace ZS, Naden RP, Chari S, Choi HK, Della-Torre E, Dicaire JF, et al. The 2019 American College of Rheumatology/European League against Rheumatism classification criteria for IgG4-related disease. Arthritis Rheumatol. 2020;72(1):7-19. https://doi.org/ggmphc. DOI: https://doi.org/10.1002/art.41120
Brito-Zerón P, Kostov B, Bosch X, Acar-Denizli N, Ramos-Casals M, Stone JH. Therapeutic approach to IgG4-related disease: A systematic review. Medicine (Baltimore). 2016;95(26):e4002. https://doi.org/jzc9. DOI: https://doi.org/10.1097/MD.0000000000004002
Martínez-Valle F, Orozco-Gálvez O, Fernández-Codina A. Update in ethiopathogeny, diagnosis and treatment of the IgG4 related disease. Med Clin (Barc). 2018;151(1):18-25. https://doi.org/jzdc. DOI: https://doi.org/10.1016/j.medcle.2018.05.005
Zhang W, Stone JH. Management of IgG4-related disease. Lancet Rheumatol. 2019;1(1):e55-65. https://doi.org/ggmphd. DOI: https://doi.org/10.1016/S2665-9913(19)30017-7
Maritati F, Peyronel F, Vaglio A. IgG4-related disease: a clinical perspective. Rheumatology (Oxford). 2020;59(Suppl 3):iii123-31. https://doi.org/gq336f. DOI: https://doi.org/10.1093/rheumatology/kez667
How to Cite
APA
ACM
ACS
ABNT
Chicago
Harvard
IEEE
MLA
Turabian
Vancouver
Download Citation
License

This work is licensed under a Creative Commons Attribution 4.0 International License.
The authors, when submitting their manuscripts, accept to transfer to Case reports the copyright of the published articles. The publisher has the right of use, reproduction, transmission, distribution and publication in any form or medium. The authors cannot allow or authorize the use of the contribution without the written consent of the journal.
Uniform Disclosure Form for possible Conflicts of Interest, the assignment of rights and responsibility must be delivered together with the original.
Those authors who have publications with this journal accept the following terms:
The authors will keep their copyright and guarantee the journal the right of first publication of their work, which will be simultaneously subject to the Creative Commons Recognition License that allows third parties to share the work whenever its author is indicated and his first publication this journal
The authors may adopt other non-exclusive licensing agreements for the distribution of the published version of the work (eg, deposit it in an institutional telematic file or publish it in a monographic volume) whenever the initial publication in this journal is indicated.
Authors are allowed and advised to disseminate their work through the Internet (eg in institutional telematic files or on their website) before and during the submission process, which can produce interesting exchanges and increase citations of the published work. (See The effect of open access).