Adult Onset Still´s Disease (AOSD): A rare condition with a classic presentation. Case Report
Enfermedad de Still del adulto: una patología rara con clínica típica. Reporte de un caso
DOI:
https://doi.org/10.15446/cr.v6n2.83482Palabras clave:
Still’s Disease Adult-Onset, Fever of Unknown Origin, Arthralgia, Exanthema (en)Enfermedad de Still del adulto, Fiebre de origen desconocido, Artralgia, Exantema (es)
Descargas
Introduction: Adult Onset Still´s Disease (AOSD) is a rare systemic inflammatory disease of unclear etiology, with low incidence and prevalence among the general population. AOSD is a common cause of fever of unknown origin (FUO) in up to 20% of cases. Due to the scarce knowledge about this disease and its diagnosis, it is usually unrecognized in the differential diagnoses, worsening the prognosis and increasing complications in some patients.
Case presentation: This is the case of a 32-year-old female patient with prolonged febrile illness, who did not respond to the antimicrobial treatments previously established. She was diagnosed with AOSD according to the Yamaguchi criteria after an extensive exclusion process. She was treated with first-line treatment with corticosteroids, achieving satisfactory results.
Conclusions: The diagnosis of AOSD is an exhaustive process. Regardless of the availability of cutting-edge diagnostic tools, the medical history of the patient and an adequate physical examination are the most important aspects to consider.
Introducción. La enfermedad de Still del adulto (ESA) es una enfermedad inflamatoria sistémica de baja incidencia y prevalencia en población general y cuya etiología aún no es clara. La ESA puede causar fiebre de origen desconocido hasta en el 20% de los casos, pero suele pasar inadvertida dentro de los diagnósticos diferenciales iniciales debido a su desconocimiento, lo que empeora el pronóstico y aumenta las complicaciones en los pacientes.
Presentación del caso. Paciente femenina de 32 años con síndrome febril prolongado que no respondía a tratamientos antimicrobianos instaurados previamente y en quien, finalmente, se diagnosticó ESA aplicando los criterios clasificatorios de Yamaguchi. La mujer recibió tratamiento de primera línea con corticosteroides y obtuvo buenos resultados.
Conclusiones. La ESA requiere un exhaustivo proceso para su diagnóstico, en el cual, a pesar de la disponibilidad de herramientas diagnósticas avanzadas, la verificación de la historia clínica y la realización de un adecuado examen físico son los aspectos más importantes a tener en cuenta.
https://doi.org/10.15446/cr.v6n2.83482
Adult Onset Still’s Disease (AOSD): A rare condition with a classic clinical presentation. Case Report
Keywords: Still’s Disease, Adult-Onset; Fever of Unknown Origin; Arthralgia; Exanthema.
Palabras clave: Enfermedad de Still del adulto; Fiebre de origen desconocido; Artralgia; Exantema.
Andrés Eduardo Prieto-Torres
Clínica Medifaca - Internal Medicine Service - Facatativá, Cundinamarca - Colombia.
Wilson Suárez-Molina
Clínica Medifaca - Internal Medicine Service - Facatativá, Cundinamarca - Colombia.
Hospital Militar Central -
Internal Medicine Service
- Bogotá D.C. - Colombia.
Jaime Iván Pantoja-Agreda
Clínica Medifaca - Internal Medicine Service -
Facatativá, Cundinamarca - Colombia.
Corresponding author
Andrés Eduardo Prieto-Torres.
Internal Medicine Service,
Clínica Medifaca. Facatativá,
Cundinamarca. Colombia.
Email: aeprietot@unal.edu.co
Received: 12/11/2019 Accepted: 24/01/2020
Resumen
Introducción. La enfermedad de Still del adulto (ESA) es una enfermedad inflamatoria sistémica de baja incidencia y prevalencia en población general y cuya etiología aún no es clara. La ESA puede causar fiebre de origen desconocido hasta en el 20% de los casos, pero suele pasar inadvertida dentro de los diagnósticos diferenciales iniciales debido a su desconocimiento, lo que empeora el pronóstico y aumenta las complicaciones en los pacientes.
Presentación del caso. Paciente femenina de 32 años con síndrome febril prolongado que no respondía a tratamientos antimicrobianos instaurados previamente y en quien, finalmente, se diagnosticó ESA aplicando los criterios clasificatorios de Yamaguchi. La mujer recibió tratamiento de primera línea con corticosteroides y obtuvo buenos resultados.
Conclusiones. La ESA requiere un exhaustivo proceso para su diagnóstico, en el cual, a pesar de la disponibilidad de herramientas diagnósticas avanzadas, la verificación de la historia clínica y la realización de un adecuado examen físico son los aspectos más importantes a tener en cuenta.
Abstract
Introduction: Adult Onset Still´s Disease (AOSD) is a rare systemic inflammatory disease of unclear etiology, with low incidence and prevalence among the general population. AOSD is a common cause of fever of unknown origin (FUO) in up to 20% of cases. Due to the scarce knowledge about this disease and its diagnosis, it is usually unrecognized in the differential diagnoses, worsening the prognosis and increasing complications in some patients.
Case presentation: This is the case of a 32-year-old female patient with prolonged febrile illness, who did not respond to the antimicrobial treatments previously established. She was diagnosed with AOSD according to the Yamaguchi criteria after an extensive exclusion process. She was treated with first-line treatment with corticosteroids, achieving satisfactory results
Conclusions: The diagnosis of AOSD is an exhaustive process. Regardless of the availability of cutting-edge diagnostic tools, the medical history of the patient and an adequate physical examination are the most important aspects to consider.
Introduction
Adult Onset Still’s disease (AOSD) is a rare inflammatory disease of unclear origin. Its incidence and prevalence vary according to the geographical area: 0.16 to 0.4 cases per 100 000 population and 1 to 34 cases per 1 000 000 population, respectively. (1) This is a disorder that affects men and women alike. (2,3)
Although the pathogenesis of AOSD is not entirely clear, it has been suggested that it is an uncontrolled inflammatory response in the form of a “cytokine storm” that occurs when individuals with non-inherited genetic susceptibility associated with different genes of human leukocyte antigen and polymorphisms in genes coding for interleukin 18 (IL-18) and macrophage migration inducer are subjected to a trigger or “second hit” such as viruses, bacteria, and hematological, or solid tumors. Such a response would cause the multi-systemic symptoms associated with the disease. It should be noted that, even though this is one of the most widely disseminated hypotheses, it is still debated. (4,5)
AOSD is a little known disease that is not included in the initial differential diagnosis of the febrile illness, leading to a delay in the diagnosis, the initiation of unnecessary pharmacological treatments that may cause adverse effects, and costly complementary studies that are not useful or comfortable for the patient.
This disease is characterized by a triad of fever, evanescent maculopapular exanthema and arthralgia:
- Fever is generally high (>39°C), with a double quotidian pattern, and usually increases in the evening and at night. This clinical sign tends to resolve on its own or rapidly with antipyretics and precedes the onset or exacerbation of other systemic symptoms. (6,7)
- The exanthema typically described in the literature is an evanescent salmon-pink maculopapular rash, occasionally pruritic, predominantly on the trunk and proximal parts of the limbs. Atypical presentations with urticarial exanthema or with persistent erythematous plaques and papules have also been described. (8)
- Multiple joints may be initially involved, predominantly the knees, ankles, and wrists, with subsequent progression to small joints.
Other manifestations of AOSD include odynophagia, splenomegaly, lymphadenopathy, and hepatomegaly. (7,9)
Macrophage activation syndrome is the complication most associated with AOSD, followed by disseminated intravascular coagulation, thrombotic thrombocytopenic purpura, and diffuse alveolar hemorrhage. Other less known complications with isolated case reports are serositis, pericardial effusion, pleural effusion, abdominal pain, pulmonary involvement, myocarditis, (10) and neurological and kidney complications.
Multiple criteria lead to the diagnosis of this disease; however, the Yamaguchi criteria are the most sensitive. To diagnose AOSD, five or more criteria must be met, and two of them must be major. The greatest limitation to the application of the Yamaguchi criteria is the need to rule out infectious processes, neoplasms and systemic rheumatological or inflammatory pathologies that produce the same symptoms. Other criteria for the diagnosis of AOSD are the Fautrel and Cush criteria, which are less known and barely used (Table 1). Currently, the course and treatment of the disease are determined based on whether the patient has a predominant systemic pattern or a joint pattern. (11)
Table 1. Classification criteria for Adult Onset Still’s Disease.
|
Yamaguchi criteria |
Fautrel criteria |
Cush criteria |
|
Major criteria: 1. Fever >39 °C, lasting 1 week or longer. 2. Arthralgia or arthritis, lasting 2 weeks or longer. 3. Typical rash. 4. Leukocytosis >10 000/mm3 con PMN >80%. |
Major criteria: 1. Fever >39°C. 2. Arthralgia. 3. Transient erythema. 4. Odinophagy. 5. PMN >80%. 6. Glycosylated ferritin <20%. |
Double score: 1. Daily recurring fever >39°C. 2. Transient erythema. 3. Leukocytosis >12 000/mm3 and ESR >40 mm/hour. 4. Negative rheumatoid factor and anti-nuclear antibodies. 5. Carpal ankylosis. |
|
Minor criteria: 1. Sore throat. 2. Lymphadenopathy. 3. Splenomegaly. 4. Abnormal liver function tests. 5. Negative tests for antinuclear antibody and rheumatoid factor. |
Minor criteria: 1. Leukocytosis >10 000/mm3. 2. Maculopapular rash. |
Simple score: 1. Onset <35 years old. 2. Arthritis. 3. Sore throat. 4. Reticuloendothelial system involvement. 5. Serositis. 6. Cervical or tarsal ankylosis |
|
Exclusion criteria: Infections, malignancies, other rheumatic or inflammatory diseases. |
It does not require the exclusion of other pathologies. |
Probable: 10 points after 12 weeks of observation. Definitive: 10 points after 6 months of follow-up. |
PMN: polymorphonuclear cells; ESR: erythrocyte sedimentation rate.
Source: Elaboration based on Giacomelli et al. (1) y Li et al. (2)
The first-line treatment for AOSD involves anti-inflammatory drugs and steroids. In 60% of the cases, the disease is controlled with glucocorticoids, and patients who do not respond to this therapy may be treated with disease modifying drugs, including methotrexate, which is the one with more evidence. (1) Biologic response modifiers are recommended in cases where the first or second line of treatment does not work, or in patients with contraindications to the use of these drugs. When the pattern is systemic, medications are initiated to control IL-1B (anakinra, canakinumab, or rilonacept) and IL-18 (tadekinig); if the condition has a predominantly joint pattern, anti-IL-6 (tocilizumab) and anti-TNF (etanercept) therapy should be initiated.
Case presentation
This is the case of a 32 year-old female patient with no relevant medical history, mestizo, single, with complete high school education, head of household, mother to two adolescents, worker in a flower farm, from a rural area of a municipality of Cundinamarca (Colombia) located at
2 580 m.a.s.l. The patient was admitted to the hospital after being referred from a primary care center because of a 15-day history of prolonged febrile illness without a clear description of the pattern. She presented migratory polyarthralgias, predominantly in wrists and ankles, and intermittent pruritic salmon-pink macular exanthema mainly in the trunk, upper limbs and proximal part of lower limbs; according to the patient, the exanthema appeared after experiencing febrile peaks, myalgias and intense odynophagia.
The patient had been previously treated with a single dose of intramuscular benzathine penicillin for suspected tonsillopharyngitis caused by Streptococcus pyogenes. Moreover, five days before being admitted, she was hospitalized and treated with antibacterial spectrum of ampicillin/sulbactam for suspected urinary tract infection; since she did not respond to the treatment and the fever peaks and leukocytosis persisted, she was transferred to be assessed by the internal medicine service.
No fever or changes in vital signs were reported in the initial physical examination. There were no signs of an inflammatory process in the tonsils, but painless and mobile posterior cervical lymphadenopathies were palpated, and pink exanthemas that disappeared under pressure were observed on thighs and forearms. Upon admission, studies were initiated for fever of unknown origin (FUO), antimicrobial and antipyretic management was suspended, and analysis was oriented towards neoplastic, inflammatory, rheumatological and infectious causes that could explain the symptoms referred by the patient.
Initial laboratory tests showed a hemogram with a marked increase in the leukocyte count (25 750 leukocytes/mm3) and predominance of polymorphonuclear cells (93.5%). Moreover, the levels of C-reactive protein, aspartate aminotransferase and alanine aminotransferase were 25.4 mg/dl, 70.5 U/L and 228 U/L, respectively. A chest X-ray was taken, revealing an unclear image of retrocardiac alveolar infiltrate (Figure 1). Based on this initial profile, and since the patient completely denied any respiratory or urinary symptoms, additional blood chemistry tests and a thoracoabdominal CT scan were ordered to rule out solid tumors and lymph node involvement.
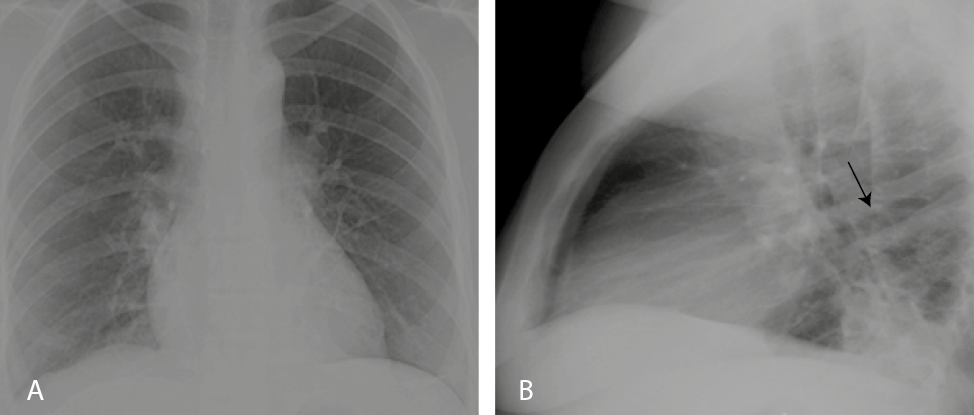
Figure 1. Chest X-ray on patient’s admission. A) anteroposterior plane without evidence of relevant alterations; B) lateral plane with segmental atelectasis.
Source: Document obtained during the study.
During hospitalization, the patient presented with feverish peaks >39°C at around dusk and at night, which made the limb exanthema more noticeable and responded quickly to management with non-steroidal anti-inflammatory drugs. Additional tests ruled out infections by human immunodeficiency virus, syphilis, hepatitis B and hepatitis C; the thick blood smear was negative for hemoparasites, the globular sedimentation rate was established at 48 mm/hour, lactate dehydrogenase was 431.7 U/L, and the peripheral blood smear did not report alterations in red cells or platelets, but indicated elevated white blood cell count with neutrophilic predominance.
Based on the reported management that the patient received prior to her arrival at the hospital, diagnostic suspicion began to shift towards AOSD or, less likely, acute rheumatic fever. Tests for antinuclear antibodies, rheumatoid factor, and antistreptolysin were negative, as were blood cultures for aerobic or anaerobic bacterial growth. An echocardiogram was performed, ruling out subclinical carditis, which was described in the 2015 revision of the Jones criteria for rheumatic fever. (12,13)
Given the persistence of the febrile peaks and considering the CT scan results, antimicrobial treatment was restarted using antipseudomonal penicillins; however, the patient continued experiencing febrile peaks and elevated leukocyte count in control hemograms. Days later, the official report of the chest tomography ruled out infectious processes but described bilateral pleural effusions with underlying passive segmental atelectasis (Figure 2A). The abdominal CT scan report documented mild nonspecific edema of the gallbladder walls and a small amount of free fluid in the posterior pouch and iliac fossae (Figure 2B); the official report ruled out infectious and neoplastic processes at the thoraco-abdominal level, so antibiotic therapy was suspended.
Finally, based on the elevated serum ferritin values (1650 ng/mL) and following the Yamaguchi criteria, AOSD was diagnosed and first-line management with oral prednisolone at a dose of 0.8 mg/kg/day was initiated. After 72 hours, the patient’s condition improved, no new febrile peaks were observed, and her arthralgias were controlled. She was subsequently discharged with steroid treatment, calcium supplementation due to the known effect of corticosteroids on ion metabolism, and orders for outpatient follow-up by the internal medicine service.
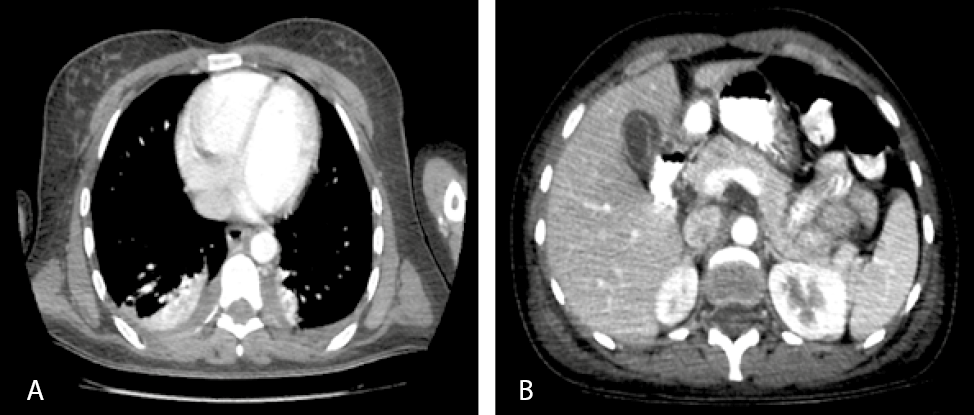
Figure 2. CT scans. A) Axial plane of the lungs showing pleural effusion associated with atelectasis; B) Axial plane of the abdomen with evidence of an inflammatory process in the gallbladder that is not associated with calculi.
Source: Document obtained during the study.
At the time of preparation of this case report, the patient’s progress had been monitored by telephone, and she reported no worsening of symptoms or adverse reactions.
Discussion
AOSD is a rare inflammatory disorder whose incidence and prevalence have not been reported in Colombia. This is an understudied disease that is generally not considered in the initial differential approach to patients with prolonged febrile syndrome given the limited knowledge of its clinical manifestations and treatment, even though it is a common documented cause of FUO.
The case presented here illustrates, precisely, the typical diagnostic triad of the disease: febrile peaks, posterior exacerbated exanthema, and joint involvement in the appendicular skeleton, in addition to the characteristic serological biomarkers. Furthermore, as a novelty, the patient presented with an inflammatory process in the gallbladder, which was not associated with calculi and had not been previously reported; this is an incidental finding that serves as a precedent for follow-up in future cases related to this pathology. This case is an example of the procedure and diagnostic method used for this disease, which is within the group of pathologies to be ruled out in the diagnosis of FUO according to the definition originally proposed by Petersdorf and Beeson, cited by Cunha et al. (14)
Regarding the available literature on AOSD, there are multiple articles worldwide on new findings concerning its pathogenesis, course, clinical markers, and treatment. (15,16) In Latin America, mainly in Brazil, Argentina, Chile, and Peru, there are a large number of case reports about its typical and atypical characteristics, and its more common complications. (17-20) Specifically in Colombia, updated literature is scarce, and there are only two retrospective studies on case series that analyze the response to monotherapy and combined treatment, (21,22) namely, a review article on its history and pathophysiology (23) and a case report that briefly describes the diagnostic process. (24) It should be noted that there is an additional report of a Colombian case published abroad. (18)
This case report attempts to provide more detailed and meticulous information about the diagnosis of AOSD by exposing the complexity of this process and highlighting common errors in the interventions performed on patients. Similarly, it stresses the importance of considering this pathology as a possible cause of the febrile syndrome and the fact that it is not necessary to carry out specialized laboratory tests to make the initial approach to the patient; in fact, a good anamnesis could lead to the suspicion of this disease and prevent the indiscriminate use of antibiotics or other types of interventions.
The authors consider that the publication of this typical case of AOSD contributes to the description of the classic characteristics that guide the diagnosis of the disease and to enrich the Colombian and world literature on the subject, since there are still large gaps in terms of diagnostic tools for this disease in which further research is needed.
Conclusion
Although a wide variety of laboratory tests and advanced imaging are available today, the patient’s medical history and a detailed physical examination remain the cornerstone of AOSD diagnosis, making it a challenge to physicians. In this sense, the case presented here demonstrates the difficulty of its diagnosis and the importance of its early recognition to avoid complications and improve the prognosis of patients.
Patient’s perspective
The patient had trouble during her hospital stay due to the length of her stay and uncertainty about her diagnosis. In addition, the woman had concerns about her financial responsibilities as a stay-at-home mother and anxiety about being away from her children, so she required support from the psychology service in order to cope with her condition and the hospital management.
Ethical considerations
This case report was approved by the Ethics Committee of Clínica Medifaca, with the patient’s informed consent. The institution where the diagnosis and follow-up were made is part of the Medilaser complex.
Conflicts of interest
None stated by the authors.
Funding
None stated by the authors.
Acknowledgements
To the medical research group that reviewed and endorsed this document.
References
1.Giacomelli R, Ruscitti P, Shoenfeld Y. A comprehensive review on adult onset Still’s disease. J Autoimmun. 2018;93:24-36. http://doi.org/dvd5.
2.Li S, Zheng S, Tang S, Pan Y, Zhang S, Fang H, et al. Autoinflammatory Pathogenesis and Targeted Therapy for Adult-Onset Still’s Disease. Clin Rev Allerg Immunol. 2020;58(1). http://doi.org/dvd7.
3.Sfriso P, Bindoli S, Galozzi P. Adult-Onset Still’s Disease: Molecular Pathophysiology and Therapeutic Advances. Drugs. 2018;78(12):1187-95. http://doi.org/gd5549.
4.Ruscitti P, Giacomelli R. Pathogenesis of adult onset still’s disease: current understanding and new insights. Expert Rev Clin Immunol. 2018;14(11):965-76. http://doi.org/dvd8.
5.Gerfaud-Valentin M, Jamilloux Y, Iwaz J, Sève P. Adult-onset Still’s disease. Autoimmun Rev. 2004;13(7):708-22. http://doi.org/c8ht.
6.Agha-Abbaslou M, Bensaci AM, Dike O, Poznansky MC, Hyat A. Adult-Onset Still’s Disease: Still a Serious Health Problem (a Case Report and Literature Review). Am J Med Case Rep. 2017;18:119-24. http://doi.org/f9pcwx.
7.Colafrancesco S, Priori R, Valesini G. Presentation and diagnosis of adult-onset Still’s disease: the implications of current and emerging markers in overcoming the diagnostic challenge. Expert Rev Clin Immunol. 2015;11(6):749-61. http://doi.org/f7mmrj.
8.Díaz P, Hidalgo-Parra I, Benavidez V, Caetano M, Reppel J, Aloise I. Enfermedad de Still del Adulto: diagnóstico a partir de las manifestaciones cutáneas. Med Cutan Iber Lat AM. 2015;43(3):196-8.
9.Narváez-García F, Pascual M, López-de Recalde M, Juarez P, Morales-Ivorra I, Notario J, et al. Adult-onset Still’s disease with atypical cutaneous manifestations. Medicine (Baltimore). 2017;96(11):e6318. http://doi.org/f9vf5f.
10.Peralta-Vargas CE, Vasquez-Kunze S. Miopericarditis en enfermedad de Still del adulto. Reporte de un caso. Rev Med Hered. 2018;19
(4):167.
11.Narváez J. Enfermedad de Still del adulto. Med Clin (Barc). 2018;150(9):348-53. http://doi.org/dvd9.
12.Karthikeyan G, Guilherme L. Acute rheumatic fever. Lancet. 2018;392(10142):161-74. http://doi.org/ggtnvq.
13.Szczygielska I, Hernik E, Kotodziejczyk B, Gazda A, Maslinska M, Gietka P. Rheumatic fever - new diagnostic criteria. Rheumatologia. 2018;56(1):37-41. http://doi.org/ggtnzq.
14.Cunha BA, Lortholary O, Cunha CB. Fever of Unknown Origin: A Clinical Approach. Am J Med. 2015;128(10):1138e1-e15. http://doi.org/f3jbfm.
15.Mitrovic S, Fautrel B. New Markers for Adult-Onset Still’s Disease. Joint Bone Spine. 2018;85(3):285-93. http://doi.org/gdq4zm.
16.Feist E, Mitrovic S, Fautrel B. Mechanisms, biomarkers and targets for adult-onset Still’s disease. Nat Rev Rheumatol. 2018;14(10):603-18. http://doi.org/gfb4p3.
17.Balcázar R, Garate G, Brigante A, Gómez G, Hogrefe J, Yucra D, Hamaui A, Duvinsky D. Manifestación atípica de enfermedad de Still. Reporte de un caso. Rev Arg Reumatol. 2018;29(2):54-6.
18.Posada-López AF, Yepes-Gaviria V, Aguirre-Henao HD, Quevedo-Cámera ML. Enfermedad de Still del adulto asociado a compromiso pulmonar. Rev Arg Reumatol. 2014;25(2):42-6.
19.Suárez.Ale H, Solís-Torres S. Enfermedad de Still del Adulto asociada a endocarditis marántica: Reporte clínico y revisión de la literatura. Rev Soc Peru Med Interna. 2015;28 (1):18-24.
20.Peruilh-Bagolini L, Tapia-Tudela G, Petit-Breuilh V, Valenzuela F, Carreño L. Enfermedad de Still del adulto, a propósito de un caso: Un desafío diagnóstico. Rev Chil Dermatol. 2016;32(4):197-201. http://doi.org/dvfb.
21.Muriel ÁJ, Rueda JM, González-Buriticá H, Castaño O. Una patología poco frecuente: la enfermedad de Still del adulto. Experiencia clínica con 17 casos. Rev Colomb Reumatol. 2016;23(2):126-30. http://doi.org/c8hz.
22.Panqueva U, Ramírez LA, Restrepo JF, Rondón F, Mora S, Valle R, et al. Enfermedad de Still del adulto: estudio de cohorte. Rev Col Reumatol. 2009;16(4):336-41. http://doi.org/f2mbbp.
23.Iglesias A, Panqueva U, Toro C, Mejía J, Rondón F, Restrepo JF, et al. Enfermedad de Still: Una perspectiva histórica y una revisión actual. Rev Colomb Reumatol. 2008;15(3):
197-206
24.Quilindo C, Morales K, Guerrero A. Enfermedad de Still, un diagnóstico diferencial importante: Reporte de un Caso. RFS Revista Facultad de Salud. 2017;9(1):21-5. http://doi.org/dvfc.
Referencias
Giacomelli R, Ruscitti P, Shoenfeld Y. A comprehensive review on adult onset Still’s disease. J Autoimmun. 2018;93:24-36. http://doi.org/dvd5.
Li S, Zheng S, Tang S, Pan Y, Zhang S, Fang H, et al. Autoinflammatory Pathogenesis and Targeted Therapy for Adult-Onset Still’s Disease. Clin Rev Allerg Immunol. 2020;58(1). http://doi.org/dvd7.
Sfriso P, Bindoli S, Galozzi P. Adult-Onset Still’s Disease: Molecular Pathophysiology and Therapeutic Advances. Drugs. 2018;78(12):1187-95. http://doi.org/gd5549.
Ruscitti P, Giacomelli R. Pathogenesis of adult onset still’s disease: current understanding and new insights. Expert Rev Clin Immunol. 2018;14(11):965-76. http://doi.org/dvd8.
Gerfaud-Valentin M, Jamilloux Y, Iwaz J, Sève P. Adult-onset Still’s disease. Autoimmun Rev. 2004;13(7):708-22. http://doi.org/c8ht.
Agha-Abbaslou M, Bensaci AM, Dike O, Poznansky MC, Hyat A. Adult-Onset Still’s Disease: Still a Serious Health Problem (a Case Report and Literature Review). Am J Med Case Rep. 2017;18:119-24. http://doi.org/f9pcwx.
Colafrancesco S, Priori R, Valesini G. Presentation and diagnosis of adult-onset Still’s disease: the implications of current and emerging markers in overcoming the diagnostic challenge. Expert Rev Clin Immunol. 2015;11(6):749-61. http://doi.org/f7mmrj.
Díaz P, Hidalgo-Parra I, Benavidez V, Caetano M, Reppel J, Aloise I. Enfermedad de Still del Adulto: diagnóstico a partir de las manifestaciones cutáneas. Med Cutan Iber Lat AM. 2015;43(3):196-8.
Narváez-García F, Pascual M, López-de Recalde M, Juarez P, Morales-Ivorra I, Notario J, et al. Adult-onset Still’s disease with atypical cutaneous manifestations. Medicine (Baltimore). 2017;96(11):e6318. http://doi.org/f9vf5f.
Peralta-Vargas CE, Vasquez-Kunze S. Miopericarditis en enfermedad de Still del adulto. Reporte de un caso. Rev Med Hered. 2018;19 (4):167.
Narváez J. Enfermedad de Still del adulto. Med Clin (Barc). 2018;150(9):348-53. http://doi.org/dvd9.
Karthikeyan G, Guilherme L. Acute rheumatic fever. Lancet. 2018;392(10142):161-74. http://doi.org/ggtnvq.
Szczygielska I, Hernik E, Kotodziejczyk B, Gazda A, Maslinska M, Gietka P. Rheumatic fever - new diagnostic criteria. Rheumatologia. 2018;56(1):37-41. http://doi.org/ggtnzq.
Cunha BA, Lortholary O, Cunha CB. Fever of Unknown Origin: A Clinical Approach. Am J Med. 2015;128(10):1138e1-e15. http://doi.org/f3jbfm.
Mitrovic S, Fautrel B. New Markers for Adult-Onset Still’s Disease. Joint Bone Spine. 2018;85(3):285-93. http://doi.org/gdq4zm.
Feist E, Mitrovic S, Fautrel B. Mechanisms, biomarkers and targets for adult-onset Still’s disease. Nat Rev Rheumatol. 2018;14(10):603-18. http://doi.org/gfb4p3.
Balcázar R, Garate G, Brigante A, Gómez G, Hogrefe J, Yucra D, Hamaui A, Duvinsky D. Manifestación atípica de enfermedad de Still. Reporte de un caso. Rev Arg Reumatol. 2018;29(2):54-6.
Posada-López AF, Yepes-Gaviria V, Aguirre-Henao HD, Quevedo-Cámera ML. Enfermedad de Still del adulto asociado a compromiso pulmonar. Rev Arg Reumatol. 2014;25(2):42-6.
Suárez.Ale H, Solís-Torres S. Enfermedad de Still del Adulto asociada a endocarditis marántica: Reporte clínico y revisión de la literatura. Rev Soc Peru Med Interna. 2015;28 (1):18-24.
Peruilh-Bagolini L, Tapia-Tudela G, Petit-Breuilh V, Valenzuela F, Carreño L. Enfermedad de Still del adulto, a propósito de un caso: Un desafío diagnóstico. Rev Chil Dermatol. 2016;32(4):197-201. http://doi.org/dvfb.
Muriel ÁJ, Rueda JM, González-Buriticá H, Castaño O. Una patología poco frecuente: la enfermedad de Still del adulto. Experiencia clínica con 17 casos. Rev Colomb Reumatol. 2016;23(2):126-30. http://doi.org/c8hz.
Panqueva U, Ramírez LA, Restrepo JF, Rondón F, Mora S, Valle R, et al. Enfermedad de Still del adulto: estudio de cohorte. Rev Col Reumatol. 2009;16(4):336-41. http://doi.org/f2mbbp.
Iglesias A, Panqueva U, Toro C, Mejía J, Rondón F, Restrepo JF, et al. Enfermedad de Still: Una perspectiva histórica y una revisión actual. Rev Colomb Reumatol. 2008;15(3):197-206.
Quilindo C, Morales K, Guerrero A. Enfermedad de Still, un diagnóstico diferencial importante: Reporte de un Caso. RFS Revista Facultad de Salud. 2017;9(1):21-5. http://doi.org/dvfc.
Cómo citar
APA
ACM
ACS
ABNT
Chicago
Harvard
IEEE
MLA
Turabian
Vancouver
Descargar cita
CrossRef Cited-by
1. Viviana López-Ramírez, Pedro Quevedo, Vanessa Cadavid-González, Gabriel Quiñones-Ossa. (2023). Myopericarditis: A rare initial manifestation of adult-onset Still’s disease. Case report. Revista Colombiana de Reumatología (English Edition), 30(2), p.176. https://doi.org/10.1016/j.rcreue.2021.06.006.
2. Moisés Casarrubias-Ramírez. (2020). Fever of unknown origin. A changing clinical spectrum and a diagnostic challenge. Case reports, 6(2), p.89. https://doi.org/10.15446/cr.v6n2.87649.
3. Andrea Bran Ordóñez, Juan Emmanuel Guevara Mejía, Yoell David Bautista Esquivel, Abraham García Kutzbach. (2023). Descripción clínica de pacientes con enfermedad de Still del adulto, serie de casos en un centro reumatológico guatemalteco. Global Rheumatology, https://doi.org/10.46856/grp.10.e173.
4. Viviana López-Ramírez, Pedro Quevedo, Vanessa Cadavid-González, Gabriel Quiñones-Ossa. (2023). Miopericarditis, una manifestación inicial poco común de la enfermedad de Still del adulto. Reporte de caso. Revista Colombiana de Reumatología, 30(2), p.176. https://doi.org/10.1016/j.rcreu.2021.06.007.
Dimensions
PlumX
Visitas a la página del resumen del artículo
Descargas
Licencia
Derechos de autor 2020 Case Reports

Esta obra está bajo una licencia internacional Creative Commons Atribución 4.0.
Los autores al someter sus manuscritos conservarán sus derechos de autor. La revista tiene el derecho del uso, reproducción, transmisión, distribución y publicación en cualquier forma o medio. Los autores no podrán permitir o autorizar el uso de la contribución sin el consentimiento escrito de la revista.
El Formulario de Divulgación Uniforme para posibles Conflictos de Interés y los oficios de cesión de derechos y de responsabilidad deben ser entregados junto con el original.
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as conservarán sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cual estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons 4.0 que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los autores/as podrán adoptar otros acuerdos de licencia no exclusiva de distribución de la versión de la obra publicada (p. ej.: depositarla en un archivo telemático institucional o publicarla en un volumen monográfico) siempre que se indique la publicación inicial en esta revista.
Se permite y recomienda a los autores/as difundir su obra a través de Internet (p. ej.: en archivos telemáticos institucionales o en su página web) antes y durante el proceso de envío, lo cual puede producir intercambios interesantes y aumentar las citas de la obra publicada. (Véase El efecto del acceso abierto).