Linfoma extranodal nasal de células T/NK. Reporte de Caso
Extranodal NK/T-cell lymphoma, nasal type: Case report
DOI:
https://doi.org/10.15446/cr.v7n1.85915Palabras clave:
Linfoma, Celulitis, Sinusitis, Linfocitos T, Herpesvirus Humano 4 (es)Lymphoma, Cellulitis, Sinusitis, T-Lymphocytes, Herpesvirus 4, Human (en)
Descargas
Introducción. El linfoma extranodal nasal de células T/natural killer (ENKL) es un linfoma no Hodgkin altamente agresivo y de etiología desconocida. Sus manifestaciones clínicas suelen ser obstrucción nasal, epistaxis y signos inflamatorios; sin embargo, el diagnóstico puede llegar a ser difícil, requiriendo histopatología e inmunohistoquímica para su detección. Como tratamiento se han propuesto radioterapia y quimioterapia, según el estadio de la enfermedad.
Presentación del caso. Paciente masculino de 44 años de edad, previamente sano, quien asistió al servicio de consulta externa por cuadro clínico de 2 meses de evolución consistente en síntomas de obstrucción y secreción nasal, edema y eritema facial. Se realizó diagnóstico inicial de celulitis facial, pero dado que no hubo mejoría con el tratamiento antibiótico, el sujeto fue remitido al servicio de urgencias de una institución de mayor complejidad, donde se le practicaron imágenes complementarias que mostraron una masa en la cavidad nasal derecha; mediante análisis histopatológico se estableció que se trataba de un ENKL, por lo que se indicó radioterapia; sin embargo, a consecuencia del estadio avanzado de dicha patología, el paciente falleció.
Conclusión. El diagnóstico oportuno de ENKL es crucial para mejorar la expectativa de vida de quienes lo padecen; sin embargo, puede representar un reto clínico debido a su presentación inespecífica.
Introduction: Extranodal NK/T-cell lymphoma, nasal type (ENKL), is a highly aggressive non-Hodgkin's lymphoma of unknown etiology. Clinical manifestations are usually nasal obstruction, epistaxis, and inflammatory signs. Diagnosis can be difficult to achieve and requires histopathology and immunohistochemistry studies. Radiotherapy and chemotherapy have been proposed as treatment, depending on the stage of the disease.
Case presentation: A 44-year-old male patient, previously healthy, attended the outpatient service due to clinical nasal obstruction, secretion, edema, and facial erythema for 2 months. Facial cellulitis was initially diagnosed, but since there was no improvement with antibiotic treatment, the patient was referred to the emergency department of a higher complexity center, where complementary imaging showed a mass in the right nasal cavity. A histopathological analysis established that it was an ENKL, so radiotherapy was indicated; however, as a result of the advanced stage of this neoplasm, the patient died.
Conclusion: Timely diagnosis of ENKL is crucial to improve life expectancy. Nevertheless, it may represent a clinical challenge due to its nonspecific presentation.
https://doi.org/10.15446/cr.v7n1.85915
Extranodal NK/T-cell lymphoma, nasal type: Case report
Keywords: Lymphoma; Cellulitis; Sinusitis; Herpesvirus 4, Human; T lymphocytes.
Palabras clave: Linfoma; Celulitis; Sinusitis; Herpesvirus Humano 4; Linfocitos T.
María Fernanda Ochoa-Ariza
Universidad Autónoma de Bucaramanga
- Faculty of Health Sciences - Medical Program - Bucaramanga - Colombia.
Clínica La Riviera - Outpatient Surgery Service
- Bucaramanga - Colombia.
Marly Esperanza Camargo-Lozada
Universidad Nacional de Colombia -
Bogotá Campus - Faculty of Medicine -
Bogotá, D.C. - Colombia.
Clínica Chicamocha - Inpatient Service -
Bucaramanga - Colombia.
Silvia Juliana García-Guevara
Universidad Autónoma de Bucaramanga
- Faculty of Health Sciences - Medical Program - Bucaramanga - Colombia.
Viviana Catalina Jiménez-Andrade
Universidad Industrial de Santander -
Faculty of Health Sciences - Medical Program - Bucaramanga - Colombia.
Marlon Adrián Laguado-Nieto
Universidad Autónoma de Bucaramanga
- Faculty of Health Sciences - Medical Program - Bucaramanga - Colombia.
Clínica FOSCAL - Intensive Care Unit Service - Colombia.
Corresponding author
Viviana Catalina Jiménez-Andrade.
Facultad de Ciencias de la Salud,
Universidad Industrial de Santander.
Bucaramanga. Colombia.
Email: andradeviviana94@gmail.com.
Received: 27/03/2020 Accepted: 28/05/2020
Resumen
Introducción. El linfoma extranodal nasal de células T/natural killer (ENKL) es un linfoma no Hodgkin altamente agresivo y de etiología desconocida. Sus manifestaciones clínicas suelen ser obstrucción nasal, epistaxis y signos inflamatorios; sin embargo, el diagnóstico puede llegar a ser difícil, requiriendo histopatología e inmunohistoquímica para su detección. Como tratamiento se han propuesto radioterapia y quimioterapia, según el estadio de la enfermedad.
Presentación del caso. Paciente masculino de 44 años de edad, previamente sano, quien asistió al servicio de consulta externa por cuadro clínico de 2 meses de evolución consistente en síntomas de obstrucción y secreción nasal, edema y eritema facial. Se realizó diagnóstico inicial de celulitis facial, pero dado que no hubo mejoría con el tratamiento antibiótico, el suejto fue remitido al servicio de urgencias de una institución de mayor complejidad, donde se le practicaron imágenes complementarias que mostraron una masa en la cavidad nasal derecha; mediante análisis histopatológico se estableció que se trataba de un ENKL, por lo que se indicó radioterapia; sin embargo, a consecuencia del estadio avanzado de dicha patología, el paciente falleció.
Conclusión. El diagnóstico oportuno de ENKL es crucial para mejorar la expectativa de vida de quienes lo padecen; sin embargo, puede representar un reto clínico debido a su presentación inespecífica.
Abstract
Introduction: Extranodal NK/T-cell lymphoma, nasal type (ENKL), is a highly aggressive non-Hodgkin’s lymphoma of unknown etiology. Clinical manifestations are usually nasal obstruction, epistaxis, and inflammatory signs. Diagnosis can be difficult to achieve and requires histopathology and immunohistochemistry studies. Radiotherapy and chemotherapy have been proposed as treatment, depending on the stage of the disease.
Case presentation: A 44-year-old male patient, previously healthy, attended the outpatient service due to clinical nasal obstruction, secretion, edema, and facial erythema for 2 months. Facial cellulitis was initially diagnosed, but since there was no improvement with antibiotic treatment, the patient was referred to the emergency department of a higher complexity center, where complementary imaging showed a mass in the right nasal cavity. A histopathological analysis established that it was an ENKL, so radiotherapy was indicated; however, as a result of the advanced stage of this neoplasm, the patient died.
Conclusion: Timely diagnosis of ENKL is crucial to improve life expectancy. Nevertheless, it may represent a clinical challenge due to its nonspecific presentation.
Introduction
Lymphomas account for 3-5% of malignant tumors, and non-Hodgkin’s lymphomas (NHL) account for 60% of all lymphomas (1). Extranodal natural killer (NK)/T-cell lymphoma, nasal type (ENKL), is a type of non-Hodgkin lymphoma that accounts for about 75% of nasal lymphomas. It is commonly found in immunocompetent people and is considered a rare neoplasm (2).
Its prevalence in the US is about 1.5%, while in Asia and Latin America, it reaches up to 8%. Mexico, Guatemala, and Peru are the countries with the most reports of this disease in Latin America. However, it should be noted that there are still no statistical data to establish a relationship between the geographical location of patients and the development of this type of tumor (1,3).
In Colombia, between 12 and 15 new cases of ENKL occur every year, with a male-to-female ratio ranging from 2:1 to 3:1 and predominance in the regions of Antioquia, Bogotá, and Valle del Cauca. It has an aggressive course, and its prognosis is severe, with an average survival rate between 6 and 25 months (4).
Although the etiology of this disease is unknown, some authors consider Epstein-Barr virus as an oncogenic factor because this infection causes neoplastic transformation of natural killer (NK) cells. Moreover, this herpesvirus has been found in almost all patients with ENKL and persists in studies in people with poor response to treatment (3-5).
The standard technique for identifying tissues with lesions containing Epstein-Barr virus is molecular detection of ribonucleic acid (RNA) by in situ hybridization, which identifies the non-coding nuclear RNA produced by the virus in the latent phase of its infection cycle. In addition, immunohistochemistry techniques are available to identify virus proteins such as LMP1 and LMP2A (6).
80% of ENKL present in the nostrils, paranasal sinuses, and upper aerodigestive tract, but sometimes it may occur in the skin, gastrointestinal tract, testicles, kidney, and, to a lesser extent, in the eyes or orbital cavities (1). Batra et al. (7) state that regional lymph nodes are only involved until the tumor spreads.
The initial signs and symptoms of ENKL are usually localized in the nasal region and include nasal obstruction and chronic rhinorrhoea, with nasal septum perforation (up to 40% of cases) and edema of the soft or hard palate caused by the formation of a deep necrotic ulceration in this area, which destroys the tissues of the palate and, occasionally, may generate oronasal communication (1,8). B symptoms (fever, weight loss, night sweats, and anemia) are occasionally reported and are usually detected in advanced stages (9).
NK cells are a lineage of lymphocytes that are part of the innate immune response mediated by molecules of the major histocompatibility complex class I. They have cytolytic functions in settings such as viral diseases or neoplasms (10,11).
Histopathological diagnosis of ENKL may be difficult to achieve due to extensive tissue necrosis. Thus, multiple biopsies are often required (4), showing large pleomorphic cell imaging with angiocentric distribution of tumor cells and angiodestruction. It is worth mentioning that the latter simulates a vascular inflammatory process with histiocytic proliferation and that it is induced by neoplastic cells that invade the vascular walls of normal tissue with generalized necrosis due to the resulting thrombosis (12).
Case presentation
A 44-year-old male patient, mestizo, resident in the municipality of San Joaquín, Santander (Colombia), from a lower-income household and a farmer, attended consultation due to a 2-month history of mucinous nasal secretion associated with edema around he eyes and on the right side of the face, feeling of fullness in the right ear, nasal tamponade, and odynophagia. The patient, who stated that he had no previous respiratory infection events or relevant exposures or history, was initially assessed by the outpatient service and prescribed with two antibiotic regimens (amoxicillin and amoxicillin-clavulanate) without improvement. For this reason, he was referred to the emergency department of a tertiary care center in Bucaramanga, Colombia.
Physical examination on admission to the emergency department revealed periorbital edema and right hemiface edema, preserved eye movements and erythema associated with posterior pharyngeal drip. Lab test results showed pancytopenia (Table 1).
Table 1. Blood count on admission and on the fifth day of antimicrobial treatment.
|
Test |
21/05/2018 |
26/05/2018 |
|
Hemoglobin |
10.3 g/dL (12-16 g/dL) |
9.2 g/dL (12-16 g/dL) |
|
Hematocrit |
30.8% (37-47%) |
26.6% (37-47%) |
|
Complete white blood cell count |
1.5 10^3/ul (5.10 10^3/ul) |
1.560 10^3/ul (5.10 10^3/ul) |
|
Neutrophils |
75.6% (50-62%) |
77.9% (50-62%) |
|
Absolute neutrophil count |
1.130 |
1.215 |
|
Lymphocytes (%) |
18.3% (25-40%) |
8.16% (25-40%) |
|
Monocytes % |
5.12% (3-7%) |
11.6% (3-7%) |
|
Mean corpuscular hemoglobin |
27.1 pg (26-34pg) |
27.1 pg (26-34pg) |
|
Mean corpuscular volume |
81.3fL (82-98fL) |
80.1fL (82-98fL) |
|
Platelets |
59.000 10^3/uL (150-500 10^3/uL) |
55.800 10^3/uL (150-500 10^3/uL) |
Source: Own elaboration.
The first diagnosis was facial and periorbital cellulitis, which were treated with an in-hospital antibiotics: ampicillin/intravenous sulbactam 3g (IV) every 6 hours plus clindamycin 600mg IV every 6 hours. Due to the persistence of the symptoms, a computed tomography (CT) scan of paranasal sinuses was performed, finding a soft tissue mass in the right nasal cavity with extension to nasopharynx and ethmoidal air cells. Based on the results of the CT scan, benign neoplasm and polyposis were suspected (Figure 1). The patient was assessed by the Otolaryngology Service, which ordered a fiberoptic nasolaryngoscopy, finding a polypoidal lesion in the right nasal fossa.
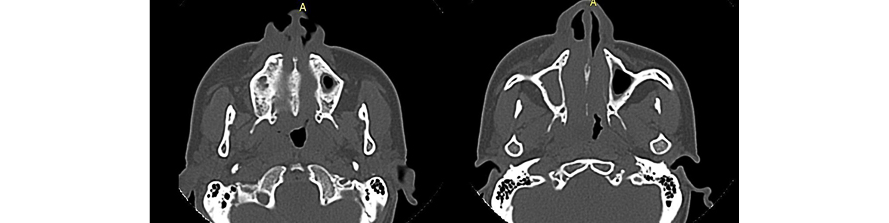
Figure 1. Computed tomography scan, axial plane, of paranasal sinuses, showing the nasopharynx and maxillary sinus, with evidence of mass in the right nasal cavity and areas of bone erosion into the nasal septum.
Source: Document obtained during the course of the study.
On the fifth day of in-hospital antibiotic treatment, the patient reported exacerbation of odynophagia and persistence of inflammatory signs on the right side of the face and subsequent purulent discharge. A new blood count was performed, revealing persistence of pancytopenia (Table 1). Therefore, it was decided to escalate antibiotic therapy to 4.5g piperacillin/tazobactam IV every six hours and perform a CT scan of the neck that reported thickening of the pharyngeal mucosa with inflammatory changes and possible tumor lesion. The patient was again assessed by the Otolaryngology Service, which found a partially necrotizing polypoid lesion with abundant secretions. At this point, the proposed treatment was posterior-to-anterior ethmoidectomy plus maxillectomy to eradicate the infectious focus.
Once the antibiotic therapy was completed, the patient was taken to surgery. Tissue samples were obtained for histopathological study. While awaiting the pathology report, the patient presented ophthalmoplegia, so a possible orbital cellulitis was considered, Consequently, the antibiotic regimen was switched to ceftriaxone plus vancomycin. Furthermore, a CT scan of the orbital cavities was requested (Figure 2), which showed preseptal cellulitis of the right orbit with displacement and compression of ocular structures that led to suspect a highly malignant neoplasm (nasal adenocarcinoma versus lymphoma).
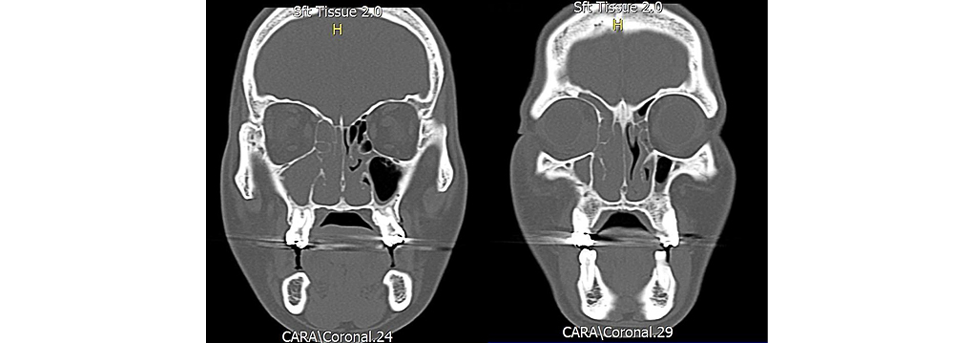
Figure 2. Computed tomography, axial plane, of orbital cavities showing infiltrative lesion of the right orbit.
Source: Document obtained during the course of the study.
Finally, the pathology report concluded that the patient had a high-grade lymphoproliferative syndrome. Immunohistochemistry, morphology and immunophenotype studies were compatible with ENKL, CD3, CD4, CD5, CD7 and CD8 were positive, and aberrant expression was established in BCL2, CD56 and CD30. The patient was referred to the radiation oncology department, which started radiation therapy on the affected area (only 22 of the 25 sessions prescribed were completed). The progression of the disease in the parafaryngeal space during treatment caused severe mechanical dysphagia that required a gastrostomy to ensure the patient’s feeding route.
Due to the advanced stage of his disease, the outpatient hematology and oncology service indicated initiation of chemotherapy. However, the patient was unable to receive such treatment due to significant body weight loss and icteric syndrome associated with signs of systemic inflammatory response with suspected abdominal sepsis secondary to non-obstructive intrahepatic cholestasis and pseudomembranous colitis. Despite antibiotic coverage (4.5g piperacillin-tazobactam IV every 6 hours and 500mg metronidazole every 8 hours due to gastrostomy), the patient had a torpid course and died.
Discussion
T/NK cell lymphomas, formerly known as lethal midline granulomas, are neoplasms derived from mature T and NK cells; of these, ENKL is more common in Asian and Latin American populations (3).
The first clinical manifestations of ENKL are usually local and the most common symptoms include epistaxis, mass sensation, nasal obstruction, and face pain and swelling (5); the latter two were observed in the reported patient. Soft or hard palate edema may also occur, which occasionally progress to deep necrotic ulceration, as in this case.
Since the clinical course of ENKL varies depending on the stage of the disease, it is common that differential diagnoses, such as acute or chronic sinusitis, are considered early in the disease, as well as infectious processes of fungal etiology (fungal rhinosinusitis) with multiple treatments without improvement. Regarding disease progression, other differential diagnoses to consider in the presence of B symptoms include squamous cell carcinoma and nasopharyngeal non-keratinizing carcinoma, which are clinically similar to ENKL (only in immunohistochemistry), lymphomatoid granulomatosis, which is caused by B cells, and diffuse B-cell lymphoma in elderly patients, which has no regular involvement in the sinus or nasal areacv (3,5,12).
ENKL diagnosis is usually histological. Studies reveal angiodestruction with zonal necrosis, cell biomarkers such as CD2 and expression of CD3 and CD56 in the cytoplasm and cytotoxic proteins in the azurophilic granules of tumor cells (13-15), as in the present case, where the pathology service reported the presence of a high-grade lymphoproliferative syndrome and immunohistochemistry with morphology and immunophenotype compatible with ENKL, in addition to positive CD3, CD4, CD5, CD7 and CD8.
The prognosis of ENKL is based on different parameters, but the International Prognostic Index is used to determine the probability of therapeutic success and survival of patients (16). Factors such as being older than 60 years, having T-cell phenotype lymphoma, having B symptoms, and identifying a high-grade tumor contribute to patients’ worse prognosis. Survival rates at 5 years are reported in 25% of tumors that predominate in the nasal cavity; this time is shorter than in patients with tumors that only involve the paranasal sinuses (1).
Treatment of ENKL should include radiation therapy, especially in early stages, and should be supplemented with advanced-stage chemotherapy, as together they offer better disease-free survival rates. Recent evidence shows that NK cells express high concentrations of
P-glycoprotein, which confers resistance to anthracycline-based chemotherapy. This has led to propose new regimens based on the use of L-asparaginase (17,18).
New problems have arisen as a result of this change in the treatment of ENKL patients. Other indices have been proposed in addition to the use of L-asparaginase-based treatments, such as the Prognostic Index of Natural Killer Lymphoma, which is intended specifically for patients treated with non-anthracycline chemotherapy regimens (19,20).
Although the clinical signs in this case are consistent with the literature, one of the most significant limitations was the lack of an early diagnosis to determine a treatment that improved the disease’s prognosis. Furthermore, due to the patient’s progressive clinical deterioration, it was not possible to supplement radiation therapy with chemotherapy sessions, which could have slowed the lymphoma’s progression.
Conclusion
ENKL is an aggressive, rapidly progressive infiltrative neoplasm that usually appears in the nasal cavity and perinasal regions but may also appear anywhere in the body. Its timely diagnosis is crucial to improving life expectancy; however, it may pose a clinical challenge due to its nonspecific presentation, often mistaken for multiple diseases. The presentation of this case aims to encourage health care professionals to consider this entity as a differential diagnosis in similar cases.
Ethical considerations
The patient’s authorization was obtained by means of an informed consent form for the preparation of this case report.
Conflicts of interest
None stated by the authors.
Funding
None stated by the authors.
Acknowledgments
None stated by the authors.
References
1.Neves MC, Lessa MM, Voegels RL, Butugan O. Primary non-Hodgkin’s lymphoma of the frontal sinus: Case report and review of the literature. Ear Nose Throat J. 2005;84(1):47-51. https://doi.org/fvb2.
2.Gourin CG, Johnson JT, Selvaggi K. Nasal T-cell lymphoma: Case report and review of diagnostic features. Ear Nose Throat J. 2001;80(7):458-60. https://doi.org/fvb3.
3.Herrera-Ariza JLA, Villamor-Rojas P. Linfoma de células T / Natural Killer extranodal, tipo nasal Extranodal Natural Killer. Acta Otorrinolaringol. Cir. Cabeza Cuello. 2015;43(3):216-21.
4.Metgud RS, Doshi JJ, Gaurkhede S, Dongre R, Karle R. Extranodal NK/T-cell lymphoma, nasal type (angiocentric T-cell lymphoma): A review about the terminology. J Oral Maxillofac Pathol. 2011;15(1):96-100. https://doi.org/cx2ww8.
5.Castro JI, Jiménez MJ, Herrera S. Linfoma nasal de células T/NK (granuloma letal de la línea media), una neoplasia agresiva. Reporte de un caso. Rev. Otorrinolaringol. Cir. Cabeza Cuello. 2018;78(2):197-201. https://doi.org/fvb6.
6.Mate JL, Navarro JT, Hernández A, Ausina V. Síndromes linfoproliferativos asociados al Virus de Epstein-Barr. Madrid: Sociedad Española de Enfermedades Infecciosas y Microbiología Clínica; 2003.
7.Batra P, Shah N, Mathur S. Midline lethal granuloma--a clinical enigma. Indian J Dent Res. 2003;14(3):174-83.
8.Califano L, Zupi A, Maremonti P, De Rosa G. Sinonasal lymphoma presenting as a lethal midline granuloma: Case report. J Oral Maxillofac Surg. 1998;56(5):667-71. https://doi.org/ct27dr.
9.Ratech H Burke JS, Blayney DW, Sheibani K, Rappaport H. A clinicopathologic study of malignant lymphomas of the nose, paranasal sinuses, and hard palate, including cases of lethal midline granuloma. Cancer. 1989;64(12):2525-31. https://doi.org/dkgsnd .
10.Cerwenka A, Lanier LL. Natural killer cell memory in infection, inflammation and cancer. Nat Rev Immunol. 2016;16(2):112-23. https://doi.org/f78kzs.
11.Sun JC, Lanier LL. NK cell development, homeostasis and function: Parallels with CD8 + T cells. Nat Rev Immunol. 2011;11(10):645-57. https://doi.org/dfvj6k.
12.Suzuki R. Leukemia and Lymphoma of Natural Killer Cells. J Clin Exp Hematop. 2005 https://doi.org/b9675f.
13.Tse E, Kwong YL. The diagnosis and management of NK/T-cell lymphomas. J Hematol Oncol. 2017;10(1):85. https://doi.org/fvb7.
14.Tse E, Kwong YL. Diagnosis and management of extranodal NK/T cell lymphoma nasal type. Expert Rev Hematol. 2016;9(9):861-71. https://doi.org/fvb8.
15.Lima M. Aggressive mature natural killer cell neoplasms: from epidemiology to diagnosis. Orphanet J Rare Dis. 2013;8(1):95. https://doi.org/fvb9.
16.International Non-Hodgkin’s Lymphoma Prognostic Factors Project. A Predictive Model for Aggressive Non-Hodgkin’s Lymphoma. N Engl J Med. 1993;329(14):987-94. https://doi.org/bjq2mx.
17.Yamaguchi M, Suzuki R, Kim SJ, Ko YH, Oguchi M, Asano N, et al. Early disease progression in patients with localized natural killer/T-cell lymphoma treated with concurrent chemoradiotherapy. Cancer Sci. 2018;109(6):2056-62.
https://doi.org/gdf853.
18.Yamaguchi M, Suzuki R, Oguchi M. Advances in the treatment of extranodal NK/T-cell lymphoma, nasal type. Blood. 2018;131(23):2528-40. https://doi.org/gdpgkw.
19.Kim SJ, Yoon DH, Jaccard A, Chng WJ, Lim ST, Hong H, et al. A prognostic index for natural killer cell lymphoma after non-anthracycline-based treatment: A multicentre, retrospective analysis. Lancet Oncol. 2016;17(3):389-400. https://doi.org/f8cxss.
20.Saavedra-Ramírez JD. Linfoma nasal de células t/natural killer extranodal refractario mal diagnosticado, tratado de manera exitosa: Informe de caso. Case Repn Oncol. 2017;10(3):1092-7. https://doi.org/fvcb.
Referencias
Neves MC, Lessa MM, Voegels RL, Butugan O. Primary non-Hodgkin’s lymphoma of the fontal sinus: Case report and review of the literature. Ear Nose Throat J. 2005;84(1):47-51. https://doi.org/fvb2.
Gourin CG, Johnson JT, Selvaggi K. Nasal T-cell lymphoma: Case report and review of diagnostic features. Ear Nose Throat J. 2001;80(7):458-60. https://doi.org/fvb3.
Herrera-Ariza JLA, Villamor-Rojas P. Linfoma de células T / Natural Killer extranodal, tipo nasal Extranodal Natural Killer. Acta Otorrinolaringol. Cir. Cabeza Cuello. 2015;43(3):216-21.
Metgud RS, Doshi JJ, Gaurkhede S, Dongre R, Karle R. Extranodal NK/T-cell lymphoma, nasal type (angiocentric T-cell lymphoma): A review about the terminology. J Oral Maxillofac Pathol. 2011;15(1):96-100. https://doi.org/cx2ww8.
Castro JI, Jiménez MJ, Herrera S. Linfoma nasal de células T/NK (granuloma letal de la línea media), una neoplasia agresiva. Reporte de un caso. Rev. Otorrinolaringol. Cir. Cabeza Cuello. 2018;78(2):197-201. https://doi.org/fvb6.
Mate JL, Navarro JT, Hernández A, Ausina V. Síndromes linfoproliferativos asociados al Virus de Epstein-Barr. Madrid:Sociedad Española de Enfermedades Infecciosas y Microbiología Clínica; 2003.
Batra P, Shah N, Mathur S. Midline lethal granuloma--a clinical enigma. Indian J Dent Res. 2003;14(3):174-83.
Califano L, Zupi A, Maremonti P, De Rosa G. Sinonasal lymphoma presenting as a lethal midline granuloma: Case report. J Oral Maxillofac Surg. 1998;56(5):667-71. https://doi.org/ct27dr.
Ratech H Burke JS, Blayney DW, Sheibani K, Rappaport H. A clinicopathologic study of malignant lymphomas of the nose, paranasal sinuses, and hard palate, including cases of lethal midline granuloma. Cancer. 1989;64(12):2525-31. https://doi.org/dkgsnd .
Cerwenka A, Lanier LL. Natural killer cell memory in infection, inflammation and cancer. Nat Rev Immunol. 2016;16(2):112-23. https://doi.org/f78kzs.
Sun JC, Lanier LL. NK cell development, homeostasis and function: Parallels with CD8 + T cells. Nat Rev Immunol. 2011;11(10):645-57. https://doi.org/dfvj6k.
Suzuki R. Leukemia and Lymphoma of Natural Killer Cells. J Clin Exp Hematop. 2005 https://doi.org/b9675f.
Tse E, Kwong YL. The diagnosis and management of NK/T-cell lymphomas. J Hematol Oncol. 2017;10(1):85. https://doi.org/fvb7.
Tse E, Kwong YL. Diagnosis and management of extranodal NK/T cell lymphoma nasal type. Expert Rev Hematol. 2016;9(9):861-71. https://doi.org/fvb8.
Lima M. Aggressive mature natural killer cell neoplasms: from epidemiology to diagnosis. Orphanet J Rare Dis. 2013;8(1):95. https://doi.org/fvb9.
International Non-Hodgkin’s Lymphoma Prognostic Factors Project. A Predictive Model for Aggressive Non-Hodgkin’s Lymphoma. N Engl J Med. 1993;329(14):987-94. https://doi.org/bjq2mx.
Yamaguchi M, Suzuki R, Kim SJ, Ko YH, Oguchi M, Asano N, et al. Early disease progression in patients with localized natural killer/T-cell lymphoma treated with concurrent chemoradiotherapy. Cancer Sci. 2018;109(6):2056-62. https://doi.org/gdf853.
Yamaguchi M, Suzuki R, Oguchi M. Advances in the treatment of extranodal NK/T-cell lymphoma, nasal type. Blood. 2018;131(23):2528-40. https://doi.org/gdpgkw.
Kim SJ, Yoon DH, Jaccard A, Chng WJ, Lim ST, Hong H, et al. A prognostic index for natural killer cell lymphoma after non-anthracycline-based treatment: A multicentre, retrospective analysis. Lancet Oncol. 2016;17(3):389-400. https://doi.org/f8cxss.
Saavedra-Ramírez JD. Linfoma nasal de células t/natural killer extranodal refractario mal diagnosticado, tratado de manera exitosa: Informe de caso. Case Repn Oncol. 017;10(3):1092-7. https://doi.org/fvcb.
Cómo citar
APA
ACM
ACS
ABNT
Chicago
Harvard
IEEE
MLA
Turabian
Vancouver
Descargar cita
Licencia
Derechos de autor 2021 Case reports

Esta obra está bajo una licencia internacional Creative Commons Atribución 4.0.
Los autores al someter sus manuscritos conservarán sus derechos de autor. La revista tiene el derecho del uso, reproducción, transmisión, distribución y publicación en cualquier forma o medio. Los autores no podrán permitir o autorizar el uso de la contribución sin el consentimiento escrito de la revista.
El Formulario de Divulgación Uniforme para posibles Conflictos de Interés y los oficios de cesión de derechos y de responsabilidad deben ser entregados junto con el original.
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as conservarán sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cual estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons 4.0 que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los autores/as podrán adoptar otros acuerdos de licencia no exclusiva de distribución de la versión de la obra publicada (p. ej.: depositarla en un archivo telemático institucional o publicarla en un volumen monográfico) siempre que se indique la publicación inicial en esta revista.
Se permite y recomienda a los autores/as difundir su obra a través de Internet (p. ej.: en archivos telemáticos institucionales o en su página web) antes y durante el proceso de envío, lo cual puede producir intercambios interesantes y aumentar las citas de la obra publicada. (Véase El efecto del acceso abierto).


























