Hernia de Amyand. Reporte de caso y revisión de la literatura actual
Amyand's hernia, case report and review of current literature
DOI:
https://doi.org/10.15446/cr.v7n2.87728Palabras clave:
Apendicitis, Hernia inguinal, Apéndice (es)Appendicitis, Appendix, Inguinal, Hernia, Amyand’s, Hernia (en)
Descargas
Introducción. La hernia de Amyand es una condición clínica infrecuente que agrupa a dos patologías quirúrgicas habituales: apendicitis aguda y hernia inguinal; en esta entidad el apéndice vermiforme se encuentra en el interior del saco de una hernia inguinal. Su diagnóstico preoperatorio es difícil, por lo que debe tenerse en cuenta en casos de hernia inguinal antes de que se presente un proceso inflamatorio, el cual puede traer más complicaciones; además, aunque no existe un consenso para el manejo según las clasificaciones actuales, estas sirven de guía para una resolución quirúrgica oportuna.
Presentación del caso. Hombre de 57 años procedente de la costa sur de Ecuador, quien consultó al servicio de emergencias de una institución de segundo nivel de atención por un cuadro clínico de 24 horas de evolución que inició con la aparición de una masa dolorosa e irreductible en la región inguinal derecha asociada a hiporexia. El paciente fue diagnosticado con hernia inguinal incarcerada y se le practicó una hernioplastia inguinal derecha en la que se encontró el apéndice y el ciego dentro del saco herniario; durante este procedimiento también se realizó apendicectomía y hernioplastia con técnica de Lichtenstein. El paciente fue dado de alta en buenas condiciones y en controles posteriores, a los 8 y 15 días de la cirugía, no presentó complicaciones.
Conclusiones. La hernia de Amyand es una entidad cada vez más frecuente que tiene un difícil diagnóstico preoperatorio debido a su cuadro clínico inespecífico. Ante la sospecha de esta patología se deben realizar estudios de imagenología que ayuden a su visualización y orienten, junto con las clasificaciones actuales de este tipo de hernias, un manejo individualizado y temprano.
Introduction: Amyand's hernia (appendix trapped within an inguinal hernia) is a rare clinical condition that groups two common surgical diseases: acute appendicitis and inguinal hernia. Its preoperative diagnosis is difficult, so it should be considered in cases of inguinal hernia before an inflammatory process occurs in the appendix to avoid complications. Although there is no consensus on its treatment, current classifications serve as a guide for a timely surgical resolution.
Case presentation: A 57-year-old male patient from the southern coast of Ecuador consulted the emergency department of a secondary level health care institution due to a 24-hour history of painful and irreducible mass in the right inguinal region associated with hyporexia. The patient was diagnosed with incarcerated inguinal hernia and underwent a right inguinal hernioplasty, during which the appendix and cecum were found inside the hernia sac. Hernioplasty and appendectomy were performed using the Lichtenstein technique. The patient was discharged in good conditions and did not have any complications at 8- and 15-day follow-up.
Conclusions: Amyand's hernia is increasingly reported. It is difficult to diagnose preoperatively due to its nonspecific symptoms. When suspected, imaging studies help its visualization and guide an individualized and early treatment, together with the current classifications of this type of hernias.
https://doi.org/10.15446/cr.v7n2.87728
Amyand’s hernia, case report and review of current literature
Keywords: Appendicitis; Appendix; Inguinal, Hernia; Amyand’s, Hernia.
Palabras clave: Apendicitis; Hernia inguinal; Apéndice.
Received: 28/05/2020 Accepted: 07/11/2020
Corresponding author
Edison Fernando Angamarca-Angamarca.
Servicio de trauma y emergencias, Departamento de Cirugía, Hospital, Hospital UTPL Santa Inés.
Loja. -Ecuador.
Email: edifer-711@hotmail.com.
Tamara Cristina Matute-Sánchez
Hospital UTPL Santa Inés - Hospitalization Service
- Loja - Ecuador.
Edison Fernando Angamarca-Angamarca
Hospital UTPL Santa Inés - Department of Surgery - Trauma and Emergency Service
- Loja - Ecuador.
Cesar Arévalo-Wazhima
Hospital Teófilo Dávila - Emergency Service
- Machala - Ecuador.
Resumen
Introducción. La hernia de Amyand es una condición clínica infrecuente que agrupa a dos patologías quirúrgicas habituales: apendicitis aguda y hernia inguinal; en esta entidad el apéndice vermiforme se encuentra en el interior del saco de una hernia inguinal. Su diagnóstico preoperatorio es difícil, por lo que debe tenerse en cuenta en casos de hernia inguinal antes de que se presente un proceso inflamatorio, el cual puede traer más complicaciones; además, aunque no existe un consenso para el manejo según las clasificaciones actuales, estas sirven de guía para una resolución quirúrgica oportuna.
Presentación del caso. Hombre de 57 años procedente de la costa sur de Ecuador, quien consultó al servicio de emergencias de una institución de segundo nivel de atención por un cuadro clínico de 24 horas de evolución que inició con la aparición de una masa dolorosa e irreductible en la región inguinal derecha asociada a hiporexia. El paciente fue diagnosticado con hernia inguinal incarcerada y se le practicó una hernioplastia inguinal derecha en la que se encontró el apéndice y el ciego dentro del saco herniario; durante este procedimiento también se realizó apendicectomía y hernioplastia con técnica de Lichtenstein. El paciente fue dado de alta en buenas condiciones y en controles posteriores, a los 8 y 15 días de la cirugía, no presentó complicaciones.
Conclusiones. La hernia de Amyand es una entidad cada vez más frecuente que tiene un difícil diagnóstico preoperatorio debido a su cuadro clínico inespecífico. Ante la sospecha de esta patología se deben realizar estudios de imagenología que ayuden a su visualización y orienten, junto con las clasificaciones actuales de este tipo de hernias, un manejo individualizado y temprano.
Abstract
Introduction: Amyand’s hernia (appendix trapped within an inguinal hernia) is a rare clinical condition that groups two common surgical diseases: acute appendicitis and inguinal hernia. Its preoperative diagnosis is difficult, so it should be considered in cases of inguinal hernia before an inflammatory process occurs in the appendix to avoid complications. Although there is no consensus on its treatment, current classifications serve as a guide for a timely surgical resolution.
Case presentation: A 57-year-old male patient from the southern coast of Ecuador consulted the emergency department of a secondary level health care institution due to a 24-hour history of painful and irreducible mass in the right inguinal region associated with hyporexia. The patient was diagnosed with incarcerated inguinal hernia and underwent a right inguinal hernioplasty, during which the appendix and cecum were found inside the hernia sac. Hernioplasty and appendectomy were performed using the Lichtenstein technique. The patient was discharged in good conditions and did not have any complications at 8- and 15-day follow-up.
Conclusions: Amyand’s hernia is increasingly reported. It is difficult to diagnose preoperatively due to its nonspecific symptoms. When suspected, imaging studies help its visualization and guide an individualized and early treatment, together with the current classifications of this type of hernias.
Introduction
Acute appendicitis and inguinal hernia are two very common conditions in the surgical field, both emergency and scheduled, with the lifetime risk of developing them being 7-8% (1-3) and 27% (4), respectively. However, it is a rare association that was first described in 1735 by Claudius Amyand in a 11-year-old boy, which is why this clinical condition is known as Amyand’s hernia (AH).
AH is more common in children and men because of the persistence of processus vaginalis, and its incidence is higher on the right side of the inguinal hernia due to its location in the right lower quadrant. This condition is difficult to diagnose and is usually done intraoperatively, but its pre-surgical identification is becoming more frequent due to a better understanding of its pathophysiology and the fact that imaging studies are carried out to confirm its presence in the event of a diagnostic suspicion.
The treatment of AH is surgical and based on the Losanoff and Banson classification (Table 1) (5-10). One of the therapeutic options, according to these authors, is incidental appendectomy in young people, although its performance is controversial, and even contraindicated in adults, when no signs of appendiceal inflammation are observed.
Table 1. Classification and surgical management of Amyand’s hernias according to Losanoff and Basson.
|
Type of hernia |
1 |
2 |
3 |
4 |
|
Features |
Normal Appendix |
Acute appendicitis located within an inguinal hernia |
Acute appendicitis with peritonitis or abdominal sepsis |
Acute appendicitis associated with other intra-abdominal disease |
|
Surgical management |
Hernia reduction (appendectomy in young patients) and mesh repair |
Appendectomy through hernia and hernia repair without mesh |
Laparotomy, appendectomy, and hernia repair without mesh |
Appendectomy and specific treatment of the associated disease as appropriate |
Source: Own elaboration based on Servide-Staffolani et al. (8) and Losanoff & Basson (10).
The following is the case of a patient with AH in whom treatment was partially implemented using hernia repair with mesh according to the Losanoff and Basson classification and in whom no complications occurred during postoperative follow-up.
Case presentation
A 57-year-old mestizo man from the southern coast of Ecuador, a longshoreman with a low socioeconomic status, consulted the emergency department of a secondary healthcare center due to a 24-hour history of painful and irreducible mass in the right inguinal region associated with general malaise and hyporexia. The patient did not report any known medical or surgical history.
Physical examination on admission revealed a 4x3cm inguinal mass with no color changes, painful on palpation and irreducible. Blood tests showed leukocytes of 10 000 with neutrophilia of 79%. Diagnostic imaging was not ordered because the symptoms were typical of an incarcerated right inguinal hernia and, consequently, therapeutic management would not change with or without an ultrasound or CT scan.
Based on the findings and on the resources available at the hospital, a conventional right inguinal hernioplasty was decided to avoid a major complication such as strangulation. During the procedure, a hernial ring of 1.5cm and a hernia sac of 6x7cm were found within the cecal appendix and cecum (Figure 1). An incidental appendectomy was performed and, since no contamination was found, a hernioplasty was performed using the Lichtenstein technique with a low-density polypropylene mesh. These procedures were performed on the same day of admission.
B

Figure 1. Amyand’s hernia. A) Hernia sac; B) Appendix (arrow)
Source: Document obtained during the study.
The patient progressed favorably and was discharged 24 hours after surgery. Medical check-ups were performed 8 and 15 days after the procedure and an adequate healing process was observed without complications.
Discussion
AH is defined as the presence of the cecal appendix within an inguinal hernia sac. This condition was first described in 1735 by the French surgeon Claudius Amyand after performing an appendectomy for perforated appendicitis in a 11-year-old patient with an incarcerated inguinal hernia (4,8,11-18). If the cecal appendix is located in a femoral hernia, it is called a De Garengeot’s hernia (19).
This type of hernia is an apparently rare condition in which two very common symptoms are associated: acute appendicitis and inguinal hernia. AH occurs in 0.1-1% of all inguinal hernias and in up to 0.3% of cases the appendix is inflamed (4,6,7,16,18,20-24). The mortality rate of this disease rises between 15% and 30% in cases of perforation due to subsequent sepsis (8,9,19).
It should be noted that there is a rise in the reports and papers on AH, showing an increase in the number of publications per year from 1985 to May 2020 (25), as shown in Figure 2, which was created based on the results of a search made in PubMed by entering the terms “Amyand, hernia,” regardless of the type of treatment and without a specific year range. Many of the publications found describe a pre-operative diagnosis established using imaging studies (5-9,14,17,19,
25-28).
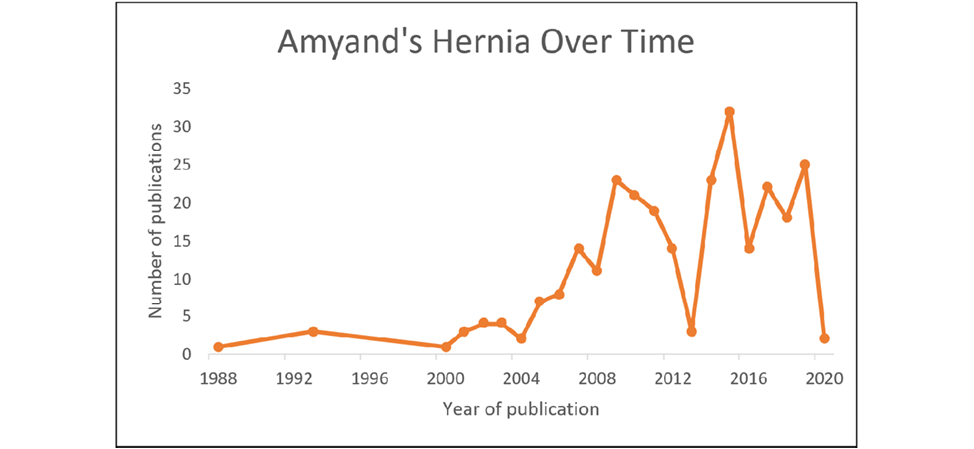
Figure 2. Number of publications on Amyand’s hernia available in PubMed, from 1985 to May 2020.
Source: Own elaboration.
The significant increase in the number of AH cases, added to the lifetime risk of developing inguinal hernia and appendicitis (27% and 7-8%, respectively) (1-4), obliges health professionals to consider this condition for differential diagnosis when evaluating an inguinal hernia, especially on the right side. However, its diagnosis is usually intraoperative, as in the case reported here.
AH occurs most often in childhood due to persistent processus vaginalis and the incidence of inguinal hernia in men. These hernias are also more frequent on the right side, as found in the reported patient, although it is not ruled out that they can occur on the left side due to mobile cecum, situs inversus, or malrotation (8,9,11,27,29).
The most frequent post-surgical complications of AH are infection, ranging from 5% to 50% (6,19,26), and hernia recurrence, neither of which was observed in the reported case.
Regarding pathophysiology, two situations may occur in AH. In the first, the appendix migrates into the hernia sac, where some authors state that a fibrous connection between the appendix (retrocecal) and the testicles added to the persistence of processus vaginalis favor the passage of the appendix into the inguinal canal and this would be the reason for the higher incidence of this condition in children and premature infants. In the second situation, the appendix becomes inflamed inside the hernia, and this may be secondary to the vascular involvement caused by the pressure of the hernial neck, triggering the inflammatory process and the subsequent bacterial proliferation (11,17,25,30), without ruling out luminal obstruction by fecaliths, ganglionic hypertrophy, parasites, or other causes.
Due to the presence of the inguinal ring, the inflammatory process of the appendix in AH may not extend into the abdominal cavity and may be limited to the inguinal canal, affecting the cecum or the base of the ring if they are also within the hernia sac (27).
As mentioned above, the diagnosis of AH is usually incidental during surgery since the symptoms are nonspecific and accompanied by lower abdominal tenderness and irreducible mass in the inguinal region, which are also symptoms of an incarcerated or strangulated inguinal hernia. Although laboratory findings are not specific, imaging studies, such as ultrasound and computed tomography (6,28), allow identifying the presence or absence of the appendix and deciding on the best approach.
Surgery is the treatment for AH and three conditions must be met before performing it: 1) it must be determined whether appendectomy is necessary, 2) the need to use prosthetic material to repair the continuity solution must be established, and 3) the best approach must be decided. Since there are so many variables, there is no general consensus on what the management of this disease should be, so Losanoff and Basson classified AH into four types with their corresponding treatment (Table 1).
When signs of inflammation are detected, an appendectomy is required; however, its use for prophylaxis is controversial when findings are incidental. Those in favor argue that if it is performed carefully avoiding contamination, morbidity and mortality, as well as the cost of future appendicitis, are reduced without increasing the anesthetic risk in young patients, although some experts do not recommend it in pediatric patients (31). On the other hand, those who oppose it claim that appendectomy transforms the procedure from a clean one to a contaminated one, which might result in infectious complications and recurrence (8,16,32).
The patient in the case reported here was diagnosed during hernioplasty with type 1 AH. Therefore, according to this classification, management included prophylactic appendectomy and hernia repair with a polypropylene mesh since there is a low probability of infection in these cases (11). The intervention was effective, and the patient’s progress was favorable in follow-up.
The satisfactory evolution of the patient reported here, as well as that of other cases mentioned in the literature, seems to be related to the use of a clean surgical technique when correcting the wall defect with a mesh after incidental appendectomy (5,16) or during the inflammatory phase, preventing contamination of the surrounding tissues because the appendix is manipulated to a minimum, the remnant appendix is isolated from the hernia sac with a good closure, and the procedure is accompanied by adequate antibiotic prophylaxis. It is worth mentioning that this technique has also reported good results in more advanced stages of appendicitis (6,8,21,32), although its performance is not usually indicated due to the high risk of infection it entails.
There is a modification or complement to the Losanoff and Basson classification known as the Rikki’s classification (33) (Table 2), in which incisional hernia is added and its management depends on the inflammatory status of the appendix.
Table 2. Modified Rikki’s classification.
|
Classification |
Features |
Surgical treatment |
|
1 |
Normal appendix |
Hernia reduction (appendectomy in young patients) and mesh repair |
|
2 |
Acute appendicitis within the sac |
Appendectomy through hernia and repair of hernia, without mesh |
|
3 |
Acute appendicitis with peritonitis or abdominal sepsis |
Laparotomy, appendectomy, and hernia repair, without mesh |
|
4 |
Acute appendicitis associated with other intra-abdominal disease |
Appendectomy and specific treatment of the associated disease as appropriate |
|
5a |
Normal appendix within an incisional hernia |
Appendectomy plus mesh herniorrhaphy |
|
5b |
Acute appendicitis within incisional hernia, without abdominal sepsis |
Appendectomy plus herniorrhaphy, without mesh |
|
6c |
Acute appendicitis within the incisional hernia, abdominal sepsis or secondary disease |
Same management as type 4. |
Source: Own elaboration based on Patoulias et al. (9), Villarreal et al. (11) and Desai et al. (29)
Both classifications mentioned above are an important guide to surgical management when AH is diagnosed intraoperatively, with herniotomy and laparotomy as access methods. However, due to clinical suspicion and the use of diagnostic imaging, pre-surgical diagnosis is becoming more common, allowing for intervention before complications with the appendix occur and even allowing a laparoscopic approach to the resolution of the hernia (9).
The first case of AH was described in 1999 by Vermillion et al. (34); since then, there has been an increase in the number of reported cases that have been resolved with this technique (17,30). For its part, the first preperitoneal mesh repair of a hernia of this type was carried out by Saggar et al. in 2004, as reported by Michalinos et al. (27)
Conclusions
AH is an apparently rare disease that is increasingly reported in the literature. It is difficult to diagnose preoperatively since it does not present with specific symptoms. Therefore, when it is suspected, imaging studies should be performed to help its visualization and guide, along with the current classifications, early individualized treatment of both appendicitis and hernia.
Ethical considerations
The patient signed an informed consent to treat and disclose his medical record for scientific and academic purposes.
Conflict of interest
None stated by the authors.
Funding
None stated by the authors.
Acknowledgments
None stated by the authors.
References
1.Bhangu A, Soreide K, Di Saverio S, Assarsson JH, Drake FT. Acute appendicitis: Modern understanding of pathogenesis, diagnosis, and management. Lancet. 2015;386(10000):1278-87. https://doi.org/f3jcx8.
2.Rafiq MS, Khan MM, Khan A, Jan H. Evaluation of postoperative antibiotics after non-perforated appendectomy. J Pak Med Assoc. 2015;65(8):815-7.
3.Daskalakis K, Juhlin C, Pahlman L. The use of pre- or postoperative antibiotics in surgery for appendicitis: A systematic review. Scand J Surg. 2014;103(1):14-20. https://doi.org/f24gvh.
4.Kromka W, Rau AS, Fox CJ. Amyand’s hernia with acute gangrenous appendicitis and cecal perforation: A case report and review of the literature. Int J Surg Case Rep. 2018;44:8-10. https://doi.org/gdw2.
5.Holmes K, Guinn JE. Amyand hernia repair with mesh and appendectomy. Surg Case Rep 2019;5(1):3-6.
6.Gómez-Sánchez J, García-Rubio J, Garde-Lecumberri C, Mirón-Pozo B. Hernia de Amyand. Reporte de un caso y revisión de la literatura. Actual Medica. 2018;103(804):95-7.
7.Mohaidin N, Ong SCL. Incidental discovery of Amyand’s hernia. BMJ Case Rep. 2018;2018:1-2. https://doi.org/gdw6.
8.Servide-Staffolani MJ, Perfecto-Valero A, Cervera-Aldama J, Anduaga-Peña MF, García-González J, Colina-Alonso A, et al. Controversias en el tratamiento de la hernia de Amyand. Rev Colomb Cirugía. 2018;33(1):107-10. https://doi.org/gdw7.
9.Patoulias D, Kalogirou M, Patoulias I. Amyand’s Hernia: an Up-to-Date Review of the Literature. Acta medica (Hradec Kral. 2017;60(3):131-4. https://doi.org/gdw8.
10.Losanoff JE, Basson MD. Amyand hernia: A classification to improve management. Hernia. 2008;12(3):325-6. https://doi.org/bfqdqs.
11.Villarreal R, Luna-Jaspe C, Cabrera LF, Vinck E. Hernia de Amyand encarcelada, revisión de la literatura y reporte de un caso en una institución de tercer nivel en Bogotá. Rev Colomb Cirugía. 2016;31(4):283-8.
12.Córdova A, Viscido G, Picón-Molina H, Palencia R, Doniquian A. Hernia de Amyand: comunicación de dos casos reparados con técnica de Rutkow-Robbins. Rev Hispanoam Hernia. 2014;2(3):111-4. https://doi.org/f2r9wb.
13.Nicola M, Mora G, Stock R, Vallejos R, Robles M, Tapia C, et al. Hernia de Amyand : presentación de un caso y revisión de la literatura. Rev Chil Cirugía. 2007;59(2):142-4. https://doi.org/fwrzb2.
14.Tsang WK, Lee KL, Tam KF, Lee SF. Acute appendicitis complicating amyand’s hernia: Imaging features and literature review. Hong Kong Med J. 2014;20(3):255-7. https://doi.org/gdxc.
15.Hiatt JR, Hiatt N. Amyand´s Hernia. N Engl J Med. 1988;318(21):1402. https://doi.org/cv4bm7
16.Benavides-de la Rosa DF, López-de Cenarruzabeitia Í, Moreno-Racionero F, Merino-Peñacoba LM, Beltrán-de Heredia J. A propósito de un caso: hernia de Amyand, diagnóstico a considerar en un procedimiento de rutina. Rev Esp. Enferm. Dig. 2015;107(11):708-9.
17.Ivashchuk G, Cesmebasi A, Sorenson EP, Tubbs SR, Loukas M. Amyand’s hernia: A review. Med Sci Monit. 2014;20:140-6. https://doi.org/f5rfhb.
18.García-Cano E, Martínez-Gasperin J, Rosales-Pelaez C, Hernández-Zamora V, Montiel-Jarquín J, Franco-Cravio F. Hernia de Amyand y apendicitis complicada; presentación de un caso y elección de tratamiento quirúrgico. Cir Cir. 2016;84(1):54-7. https://doi.org/f3hb8h.
19.Agirre-Etxabe L, Prieto-Calvo M, García-Etxebarría A, García-Gomzález J, Sarriugarte-Lasarte A, Colina-Alonso A. Hernia de Amyand (tipo 2 de Losanoff) diagnosticada preoperatoriamente y tratada mediante hernioplastia con malla biológica. Rev Hispanoam Hernia. 2014;2(4):169-72. https://doi.org/f2scff.
20.Mebis W, Hoste P, Jager T. Amyand’s Hernia. J Belgian Soc Radiol. 2018;102(1):8. https://doi.org/gdxn.
21.Chiang CC, Liu PH, Chou CP, Liu CH, Tsai MJ. Incarcerated Amyand´s hernia. Ci Ji Yi Xue Za Zhi. 2017;29(2):129-30.
22.Bhatti SI, Hashmi MU, Tariq U, Bhatti HI, Parkash J, Fatima Z. Amyand’s Hernia: A Rare Surgical Pathology of the Appendix. Cureus. 2018;10(6):e2827. https://doi.org/gdxp.
23.Ortega-León LH, Ramírez-Tapia D, Dieguez-Jiménez CM, Cruz-Melgar LM, García-Puig MA, Chávez-Gómez A, et al. Hernia de Amyand : Presentación de un caso y revisión de la bibliografía. Rev Médica del Hosp Gen México. 2011;74(2):98-100.
24.Vidal-González P, Contreras R, Sánchez G, Flores LM, Kunz W, Menéndez AL, et al. Hernia de Amyand. Cir Gen. 2005;27:328-9.
25.Burgess PL, Brockmeyer JR, Johnson EK. Amyand hernia repaired with Bio-A: A case report and review. J Surg Educ. 2011;68(1):62-6. https://doi.org/b3bwwm.
26.Manzanares-Campillo M, Muñoz-Atienza V, Sánchez-García S, García-Santos E, Ruescas-García F, Martín Fernández J. Hernia de Amyand: presentación de dos casos y revisión de la bibliografía. Cir Cir. 2014;84(2):195-9.
27.Michalinos A, Moris D, Vernadakis S. Amyand’s hernia: A review. Am J Surg. 2014;207(6):989-95. https://doi.org/gdxs.
28.Guler I, Alkan E, Nayman A, Tolu I. Amyand’s Hernia: Ultrasonography Findings. J Emerg Med. 2016;50(1):e15-7. https://doi.org/f747tf.
29.Desai G, Suhani, Pande P, Thomas S. Amyand´s Hernia: Our Experience and Review of Literature. Arq Bras Cir Dig. 2017;30(4):287-8. https://doi.org/gdxt.
30.Angamarca E, Mendieta-Bermeo EG, Merchán-Peñafiel P, Matute-Sánchez T. Caso Clínico: Hernia de Amyand, Resolución Laparoscópica. Rev Médica Hosp del José Carrasco Arteaga. 2016;8(2):205-8. https://doi.org/gdxv.
31.Cigsar EB, Karadag CA, Dokucu AI. Amyand’s hernia: 11 years of experience. J Pediatr Surg. 2016;51(8):1327-9. https://doi.org/f839vr.
32.Sancho-Muriel J, Torregrosa-Gallud A, García-Pastor P, López-Rubio M, Argüelles BG, Bueno-Lledó JA. Hernia de Amyand: presentación de tres casos y revisión bibliográfica. Rev Hispanoam Hernia. 2015;4(3):2-6. https://doi.org/f3g34p.
33.Singal R, Gupta S. “Amyand’s Hernia” Pathophysiology, Role of Investigations and Treatment. Maedica (Buchar). 2011;6(4):321-7.
34.Vermillion JM, Abernathy SW, Snyder SK. Laparoscopic reduction of Amyand’s hernia. Hernia. 1999;3(3):159-60. https://doi.org/bggw4p.
Referencias
Bhangu A, Soreide K, Di Saverio S, Assarsson JH, Drake FT. Acute appendicitis: Modern understanding of pathogenesis, diagnosis, and management. Lancet. 2015;386(10000):1278-87. https://doi.org/f3jcx8.
Rafiq MS, Khan MM, Khan A, Jan H. Evaluation of postoperative antibiotics after non-perforated appendectomy. J Pak Med Assoc. 2015;65(8):815-7.
Daskalakis K, Juhlin C, Pahlman L. The use of pre- or postoperative antibiotics in surgery for appendicitis: A systematic review. Scand J Surg. 2014;103(1):14-20. https://doi.org/f24gvh.
Kromka W, Rau AS, Fox CJ. Amyand’s hernia with acute gangrenous appendicitis and cecal perforation: A case report and review of the literature. Int J Surg Case Rep. 2018;44:8-10. https://doi.org/gdw2.
Holmes K, Guinn JE. Amyand hernia repair with mesh and appendectomy. Surg Case Rep 2019;5(1):3-6. DOI: https://doi.org/10.1186/s40792-019-0600-2
Gómez-Sánchez J, García-Rubio J, Garde-Lecumberri C, Mirón-Pozo B. Hernia de Amyand. Reporte de un caso y revisión de la literatura. Actual Medica. 2018;103(804):95-7. DOI: https://doi.org/10.15568/am.2018.804.cc02
Mohaidin N, Ong SCL. Incidental discovery of Amyand’s hernia. BMJ Case Rep. 2018;2018:1-2. https://doi.org/gdw6.
Servide-Staffolani MJ, Perfecto-Valero A, Cervera-Aldama J, Anduaga-Peña MF, García-González J, Colina-Alonso A, et al. Controversias en el tratamiento de la hernia de Amyand. Rev Colomb Cirugía. 2018;33(1):107-10. https://doi.org/gdw7.
Patoulias D, Kalogirou M, Patoulias I. Amyand’s Hernia: an Up-to-Date Review of the Literature. Acta medica (Hradec Kral. 2017;60(3):131-4. https://doi.org/gdw8.
Losanoff JE, Basson MD. Amyand hernia: A classification to improve management. Hernia. 2008;12(3):325-6. https://doi.org/bfqdqs.
Villarreal R, Luna-Jaspe C, Cabrera LF, Vinck E. Hernia de Amyand encarcelada, revisión de la literatura y reporte de un caso en una institución de tercer nivel en Bogotá. Rev Colomb Cirugía. 2016;31(4):283-8.
Córdova A, Viscido G, Picón-Molina H, Palencia R, Doniquian A. Hernia de Amyand: comunicación de dos casos reparados con técnica de Rutkow-Robbins. Rev Hispanoam Hernia. 2014;2(3):111-4. https://doi.org/f2r9wb.
Nicola M, Mora G, Stock R, Vallejos R, Robles M, Tapia C, et al. Hernia de Amyand : presentación de un caso y revisión de la literatura. Rev Chil Cirugía. 2007;59(2):142-4. https://doi.org/fwrzb2.
Tsang WK, Lee KL, Tam KF, Lee SF. Acute appendicitis complicating amyand’s hernia: Imaging features and literature review. Hong Kong Med J. 2014;20(3):255-7. https://doi.org/gdxc.
Hiatt JR, Hiatt N. Amyand´s Hernia. N Engl J Med. 1988;318(21):1402. https://doi.org/cv4bm7
Benavides-de la Rosa DF, López-de Cenarruzabeitia Í, Moreno-Racionero F, Merino-Peñacoba LM, Beltrán-de Heredia J. A propósito de un caso: hernia de Amyand, diagnóstico a considerar en un procedimiento de rutina. Rev Esp. Enferm. Dig. 2015;107(11):708-9.
Ivashchuk G, Cesmebasi A, Sorenson EP, Tubbs SR, Loukas M. Amyand’s hernia: A review. Med Sci Monit. 2014;20:140-6. https://doi.org/f5rfhb.
García-Cano E, Martínez-Gasperin J, Rosales-Pelaez C, Hernández-Zamora V, Montiel-Jarquín J, Franco-Cravio F. Hernia de Amyand y apendicitis complicada; presentación de un caso y elección de tratamiento quirúrgico. Cir Cir. 2016;84(1):54-7. https://doi.org/f3hb8h.
Agirre-Etxabe L, Prieto-Calvo M, García-Etxebarría A, García-Gomzález J, Sarriugarte-Lasarte A, Colina-Alonso A. Hernia de Amyand (tipo 2 de Losanoff) diagnosticada preoperatoriamente y tratada mediante hernioplastia con malla biológica. Rev Hispanoam Hernia. 2014;2(4):169-72. https://doi.org/f2scff.
Mebis W, Hoste P, Jager T. Amyand’s Hernia. J Belgian Soc Radiol. 2018;102(1):8. https://doi.org/gdxn.
Chiang CC, Liu PH, Chou CP, Liu CH, Tsai MJ. Incarcerated Amyand´s hernia. Ci Ji Yi Xue Za Zhi. 2017;29(2):129-30.
Bhatti SI, Hashmi MU, Tariq U, Bhatti HI, Parkash J, Fatima Z. Amyand’s Hernia: A Rare Surgical Pathology of the Appendix. Cureus. 2018;10(6):e2827. https://doi.org/gdxp.
Ortega-León LH, Ramírez-Tapia D, Dieguez-Jiménez CM, Cruz-Melgar LM, García-Puig MA, Chávez-Gómez A, et al. Hernia de Amyand : Presentación de un caso y revisión de la bibliografía. Rev Médica del Hosp Gen México. 2011;74(2):98-100.
Vidal-González P, Contreras R, Sánchez G, Flores LM, Kunz W, Menéndez AL, et al. Hernia de Amyand. Cir Gen. 2005;27:328-9.
Burgess PL, Brockmeyer JR, Johnson EK. Amyand hernia repaired with Bio-A: A case report and review. J Surg Educ. 2011;68(1):62-6. https://doi.org/b3bwwm.
Manzanares-Campillo M, Muñoz-Atienza V, Sánchez-García S, García-Santos E, Ruescas-García F, Martín Fernández J. Hernia de Amyand: presentación de dos casos y revisión de la bibliografía. Cir Cir. 2014;84(2):195-9.
Michalinos A, Moris D, Vernadakis S. Amyand’s hernia: A review. Am J Surg. 2014;207(6):989-95. https://doi.org/gdxs.
Guler I, Alkan E, Nayman A, Tolu I. Amyand’s Hernia: Ultrasonography Findings. J Emerg Med. 2016;50(1):e15-7. https://doi.org/f747tf.
Desai G, Suhani, Pande P, Thomas S. Amyand´s Hernia: Our Experience and Review of Literature. Arq Bras Cir Dig. 2017;30(4):287-8. https://doi.org/gdxt.
Angamarca E, Mendieta-Bermeo EG, Merchán-Peñafiel P, Matute-Sánchez T. Caso Clínico: Hernia de Amyand, Resolución Laparoscópica. Rev Médica Hosp del José Carrasco Arteaga. 2016;8(2):205-8. https://doi.org/gdxv.
Cigsar EB, Karadag CA, Dokucu AI. Amyand’s hernia: 11 years of experience. J Pediatr Surg. 2016;51(8):1327-9. https://doi.org/f839vr.
Sancho-Muriel J, Torregrosa-Gallud A, García-Pastor P, López-Rubio M, Argüelles BG, Bueno-Lledó JA. Hernia de Amyand: presentación de tres casos y revisión bibliográfica. Rev Hispanoam Hernia. 2015;4(3):2-6. https://doi.org/f3g34p.
Singal R, Gupta S. “Amyand’s Hernia” Pathophysiology, Role of Investigations and Treatment. Maedica (Buchar). 2011;6(4):321-7.
Vermillion JM, Abernathy SW, Snyder SK. Laparoscopic reduction of Amyand’s hernia. Hernia. 1999;3(3):159-60. https://doi.org/bggw4p.
Cómo citar
APA
ACM
ACS
ABNT
Chicago
Harvard
IEEE
MLA
Turabian
Vancouver
Descargar cita
CrossRef Cited-by
1. Leonor Murça da Silva Balo, Rafael Antônio Vicente Lacerda, Damião Maquina Mariti, Joaquim Lima Quibuco, Yunior Collazo Velazco. (2025). Left-Sided Amyand’s Hernia Managed Without Appendectomy: A Case Report of a Rare Diagnosis. Cureus, https://doi.org/10.7759/cureus.82559.
Dimensions
PlumX
Visitas a la página del resumen del artículo
Descargas
Licencia
Derechos de autor 2021 Case reports

Esta obra está bajo una licencia internacional Creative Commons Atribución 4.0.
Los autores al someter sus manuscritos conservarán sus derechos de autor. La revista tiene el derecho del uso, reproducción, transmisión, distribución y publicación en cualquier forma o medio. Los autores no podrán permitir o autorizar el uso de la contribución sin el consentimiento escrito de la revista.
El Formulario de Divulgación Uniforme para posibles Conflictos de Interés y los oficios de cesión de derechos y de responsabilidad deben ser entregados junto con el original.
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as conservarán sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cual estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons 4.0 que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los autores/as podrán adoptar otros acuerdos de licencia no exclusiva de distribución de la versión de la obra publicada (p. ej.: depositarla en un archivo telemático institucional o publicarla en un volumen monográfico) siempre que se indique la publicación inicial en esta revista.
Se permite y recomienda a los autores/as difundir su obra a través de Internet (p. ej.: en archivos telemáticos institucionales o en su página web) antes y durante el proceso de envío, lo cual puede producir intercambios interesantes y aumentar las citas de la obra publicada. (Véase El efecto del acceso abierto).