Folliculitis decalvans: a case report of satisfactory recovery after implementing isotretinoin therapy
Foliculitis decalvante. Reporte de un caso con recuperación satisfactoria mediante tratamiento con isotretinoina
Folliculitis decalvans: Um relato de caso em um trabalhador de saúde de 26 anos de idade
DOI:
https://doi.org/10.15446/cr.v8n1.88800Palabras clave:
Folliculitis, Hair Follicle, Isotretinoin, Cicatricial alopecia (en)Foliculitis, Isotretinoina, Folículo piloso, Alopecia (es)
Descargas
Introduction: Folliculitis decalvans is a rare skin disease characterized by the presence of painful papules and pustules with an underlying neutrophilic infiltrate, usually on the scalp. Its treatment is lengthy and challenging, and recurrence is relatively common. Although its etiology is unknown, several theories explaining its development have been proposed, including colonization by Staphylococcus aureus.
Case description: This is the case of a 26-year-old male healthcare worker who visited the outpatient service after experiencing a 4-year history of painful pustules on the scalp; initially these lesions were located in the occipital region, but then also started to appear in the temporal and parietal regions. After being treated for bacterial folliculitis and having several recurrences, a skin biopsy was performed, which allowed diagnosing him with folliculitis decalvans. Once the diagnosis was made, isotretinoin (20mg) treatment was implemented for a year and a half, achieving complete remission of the lesions.
Conclusion: Although this case has some limitations, such as the lack of histopathology images and some control laboratory tests, it clearly shows the difficulties faced when treating this type of skin disorders and presents an overview of the use of isotretinoin, evidencing that although this drug is well tolerated, possible adverse reactions from drug interactions with trimethoprim/sulfamethoxazole may arise. In addition, this case is of great importance since the possible presence of a familial cluster of folliculitis decalvans could be confirmed, if further genetic testing is performed.
Introducción. La folliculitis decalvans es una enfermedad dermatológica rara caracterizada por la presencia de pápulas y pústulas dolorosas que están acompañadas de un infiltrado de neutrófilos subyacente. Esta condición suele aparecer en el cuero cabelludo, su recurrencia es relativamente común y su tratamiento, largo y difícil. Aunque su etiología es desconocida, se han propuesto muchas teorías que intentan explicar su aparición, siendo la colonización por Staphylococcus aureus una de ellas.
Presentación del caso. Hombre de 26 años que se desempeñaba como trabajador de la salud y consultó por un cuadro clínico de 4 años de evolución caracterizado por la aparición de pústulas dolorosas en la región occipital, las cuales, posteriormente se extendieron a la región temporal y parietal. Después de tratarlo como una foliculitis infecciosa y tras múltiples recurrencias, se realizó una biopsia de las lesiones que permitió diagnosticarlo con folliculitis decalvans. Se instauró un tratamiento consistente de 20mg de isotretinoina al día por un año y medio, con el cual se logró la resolución de la folicutis. Sin embargo, dos años después tuvo un relapso, pero, según el paciente, esto pudo ocurrir por el consumo de derivados lácteos, ya que, según indicó, cuando suspende el consumo de esta clase de productos no aparecen más lesiones luego de 2-3 semanas..
Conclusión. Aunque este caso tiene algunas limitaciones como la ausencia de imágenes histopatológicas y algunos laboratorios de control, muestra las dificultades para tratar este tipo de condiciones dermatológicas y presenta un panorama del uso de la isotretinoina, ya que evidencia que este medicamento tiene una buena tolerancia, pero presenta interacciones medicamentosas adversas con la trimetoprima/sulfametoxazol. Además, este caso es de gran importancia, ya que, si se realizan más pruebas genéticas. podría confirmarse la posible presencia de un grupo familiar de foliculitis decalvante.
Descrição do caso: Um trabalhador de saúde masculino de 26 anos descreve uma história clínica de quatro anos de pústulas e pápulas de início insidioso, aparecendo inicialmente na região occipital e depois distribuindo para as regiões temporal e occipital. Após tratamento para outras condições infecciosas e sem várias recidivas, foi feita uma biópsia das lesões. Esta biópsia foi compatível com o diagnóstico de Folliculitis decalvans. Após a biópsia, ele foi tratado com Isotretinoína 20mg durante um ano e meio com remissão completa.
Discussão: Este caso expõe claramente as dificuldades de tratar este tipo de condições dermatológicas, requer paciência e uma grande quantidade de recursos. Este caso é importante, pois mostra sinais e sintomas comuns. Uma análise mais aprofundada do histórico genético e da condição imunológica do paciente pode ser aconselhável.
Conclusão: A foliculite decalvante é difícil de diagnosticar e tratar. Vários tratamentos podem ser necessários. A recorrência é sempre uma possibilidade.
https://doi.org/10.15446/cr.v8n1.88800
Folliculitis decalvans: a case report of satisfactory recovery after implementing isotretinoin therapY
Keywords: Folliculitis; Hair Follicle; Isotretinoin; Cicatricial alopecia.
Palabras clave: Foliculitis; Alopecia Folículo piloso; Isotretinoina.
Julián Felipe Porras-Villamil
Universidad Nacional de Colombia
- Bogotá Campus - Faculty of Medicine
- Master’s degree in Infections and Tropical Health
- Bogotá D.C. - Colombia.
Angela Catalina Hinestroza-Ruiz
Gabriela Andrea López-Moreno
Doris Juliana Parra-Sepúlveda
Universidad Nacional de Colombia
- Sede Bogotá - Faculty of Medicine
- Medical Program - Bogotá D.C. - Colombia.
Corresponding author
Julián Felipe Porras-Villamil.
Maestría en infecciones y salud en el trópico,
Facultad de Medicina, Universidad Nacional de Colombia. Bogotá D.C. Colombia. Email: jfporrasv@unal.edu.co
Received: 02/07/2020 Accepted: 23/12/2020
Abstract
Introduction: Folliculitis decalvans is a rare skin disease characterized by the presence of painful papules and pustules with an underlying neutrophilic infiltrate, usually on the scalp. Its treatment is lengthy and challenging, and recurrence is relatively common. Although its etiology is unknown, several theories explaining its development have been proposed, including colonization by Staphylococcus aureus.
Case description: This is the case of a 26-year-old male healthcare worker who visited the outpatient service after experiencing a 4-year history of painful pustules on the scalp; initially these lesions were located in the occipital region, but then also started to appear in the temporal and parietal regions. After being treated for bacterial folliculitis and having several recurrences, a skin biopsy was performed, which allowed diagnosing him with folliculitis decalvans. Once the diagnosis was made, isotretinoin (20mg) treatment was implemented for a year and a half, achieving complete remission of the lesions.
Conclusion: Although this case has some limitations, such as the lack of histopathology images and some control laboratory tests, it clearly shows the difficulties faced when treating this type of skin disorders and presents an overview of the use of isotretinoin, evidencing that although this drug is well tolerated, possible adverse reactions from drug interactions with trimethoprim/sulfamethoxazole may arise. In addition, this case is of great importance since the possible presence of a familial cluster of folliculitis decalvans could be confirmed, if further genetic testing is performed.
Resumen
Introducción. La folliculitis decalvans es una enfermedad dermatológica rara caracterizada por la presencia de pápulas y pústulas dolorosas que están acompañadas de un infiltrado de neutrófilos subyacente. Esta condición suele aparecer en el cuero cabelludo, su recurrencia es relativamente común y su tratamiento, largo y difícil. Aunque su etiología es desconocida, se han propuesto muchas teorías que intentan explicar su aparición, siendo la colonización por Staphylococcus aureus una de ellas.
Presentación del caso. Hombre de 26 años que se desempeñaba como trabajador de la salud y consultó por un cuadro clínico de 4 años de evolución caracterizado por la aparición de pústulas dolorosas en la región occipital, las cuales posteriormente se extendieron a la región temporal y parietal. Después de tratarlo como una foliculitis infecciosa y tras múltiples recurrencias, se realizó una biopsia de las lesiones que permitió diagnosticarlo con folliculitis decalvans. Se instauró un tratamiento consistente de 20mg de isotretinoina al día por un año y medio, con el cual se logró la resolución de la folicutis. Sin embargo, dos años después tuvo un relapso, pero, según el paciente, esto pudo ocurrir por el consumo de derivados lácteos, ya que, según indicó, cuando suspende el consumo de esta clase de productos no aparecen más lesiones luego de 2-3 semanas.
Conclusión. Aunque este caso tiene algunas limitaciones como la ausencia de imágenes histopatológicas y algunos laboratorios de control, muestra las dificultades para tratar este tipo de condiciones dermatológicas y presenta un panorama del uso de la isotretinoina, ya que evidencia que este medicamento tiene una buena tolerancia, pero presenta interacciones medicamentosas adversas con la trimetoprima/sulfametoxazol. Además, este caso es de gran importancia, ya que, si se realizan más pruebas genéticas, podría confirmarse la posible presencia de un grupo familiar de foliculitis decalvante.
Introduction
Folliculitis decalvans, also known as scarring alopecia, is a type of primary cicatricial alopecia (for a description of the different types of primary cicatricial alopecia see Table 1) (1). It is a rare skin disease characterized by the presence of inflammatory neutrophilic infiltrates and scarring that cause perifollicular papules and pustules, and it accounts for approximately 10 % of all primary cicatrizing alopecia cases (2,3). This condition was first described by Quinquaudin 1888 (3,4), but it was only until 1905 that it was named as folliculitis decalvans by Broqc et al. (5)
Table 1. Types of primary scarring alopecia.
|
Lymphocytic |
Neutrophilic |
|
Discoid lupus erythematosus |
Folliculitis decalvans |
|
Lichen planopilaris Classic With lichen planus and/or spinous lesions With frontal sclerosing alopecia |
Acne keloidalis nuchae |
|
Pseudopelade of Brocq Classic Non-specific scarring alopecia |
Tinea capitis |
|
Tufted folliculitis |
|
|
Follicular degeneration syndrome |
Acne necrotica |
|
Alopecia mucinosa |
Dissecting cellulitis of the scalp |
Source: Own elaboration based on (1).
It generally occurs in middle-aged adults, predominately males, and tends to be more frequent in people with dark skin. Although its etiology is unknown, it has been described that Staphylococcus aureus may be a contributing factor; (6-8) other possible causes include mechanisms involving superantigens or cytotoxins that bind to themajor histocompatibility complex class II (MHC II) molecules (9) and a genetic component, since several familial cases have been reported. (2,10,11)
Folliculitis decalvans management has proven to be a challenge since there is a wide range of treatment alternatives, including antibiotic therapy (tetracycline, trimethoprim/sulfamethoxazole, cephalosporins, ciprofloxacin, minocycline or clindamycin or clarithromycin plus rifampicin) (1,6,9), the use of topical antibiotics (for example erythromycin, mupirocin and clindamycin) (1), antifungals, retinoids, corticosteroids (topical or oral), phototherapy, and laser depilation. (1,7,12)
The occipital region and the vertex are usually the most affected areas in patients with this condition. Generally, folliculitis decalvans starts as a single lesion and then spreads in a centrifugal progression with the development of painful follicular papules and pustules. (2,5) As the disease progresses, a hardened erythematous plaque appears. (7) Follicular keratosis, erosions and hemorrhagic crusts are also observed. (5,13) Furthermore, some patients may experience spontaneous bleeding, pain, and a burning sensation. (5,6) Likewise, polytrichia (tufted hairs), that is, the presence of multiple hair shafts emerging from a single dilated hair follicle, may also be found in some cases. (5,6,9,14)
Dermatoscopy has been shown to be a useful procedure for diagnosing this skin condition. (15) In this regard, trichoscopy can be highly useful. In patients with folliculitis decalvans, the main finding during this examination is the presence of tufted hairs surrounded by perifollicular hyperplasia that may be arranged in a starburst pattern (starburst sign); other findings include the presence of yellowish tubular scaling and follicular pustules with emerging hair shafts in their midpoint. In addition, white and milky red areas lacking follicular openings are predominant in long-lasting lesions. (16,17)
Histopathologically, these lesions are first characterized y by the presence of neutrophilic infiltrates, and, as it progresses, the presence of neutrophilic, lymphocytic and histiocytic infiltrates. (18) At first, the location of the infiltrate is peri-infundibular, but it may affect the entire follicle. (18,19)
Other usual findings in patients with folliculitis decalvanas include the formation of abscesses and the presence of polythrichia and perifollicular fibrosis. (19) Infectious agents are rarely found and differential diagnoses include infectious folliculitis, follicular degeneration syndrome, and acne necrotica. (1) This paper reports the case of a young healthcare worker with folliculitis decalvans.
Case presentation
This is the case of a 26-year-old middle-class male healthcare worker of Hispanic origin, from Bogotá D.C., Colombia, who, in August 2017, visited the outpatient service of a tertiary care hospital due to a history of approximately 4 years of pustules and papules in the scalp.
According to the patient, he did not have any relevant history of disease or surgeries. He reported drinking alcohol occasionally but denied having used psychoactive substances; also, he did not have any known allergy. The patient had the following family history of disease: gastric cancer (paternal grandmother), breast cancer (half-sister), and diabetes mellitus type 2, hypertriglyceridemia, and high blood pressure in other relatives, both maternal and paternal.
The following findings were reported on the physical examination made during the outpatient appointment: blood pressure: 118/76; heart rate: 64 bpm; respiratory rate: 16 bpm; body temperature: 36.6°C; weight: 91kg, and height: 168cm. Likewise, several lesions (approximately 60) compatible with perifollicular papules and pustules were observed mainly on the scalp (in the vertex and the occipital, temporal, and parietal regions), while some others were located in the bordering area between the neck and the scalp.; there were no lesions in other regions different than the scalp, that is, the face, armpits, groin or buttocks. Regarding its mental health status, the patient reported feeling irritable and having a negative attitude due to the lack of sleep experienced as a result of the pain produced by the lesions. There were no other significant findings.
During the 2017 outpatient appointment, the patient reported the following sequence of events.
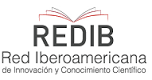
August 2015: The patient reported that he started suffering from individual and extremely painful and suppurating pustules since the second semester of 2015. In addition, according to the patient, each lesion had the same rapid evolution, described as follows: 1) development of painful erythema, 2) increase in the severity of erythema and swelling, 3) appearance of a pustule, and 4) spontaneous pustule rupture with blood and purulent fluid (pus) secretion. (Figure 1A). Most of the lesions appeared in the occipital region of the scalp. This situation persisted over time, but as there were very few lesions, he did not did not seek medical help. According to the patient, the appearance of the first lesions was caused by a prolonged and seriously stressful situation.
Figure 1. A) A pustule on the scalp, more specifically in the bordering area between the scalp and the neck. B) Site of the skin biopsy, near the vertex. C) Erythematous swelling secondary to the application of fusidic acid.
Source: Images obtained while conducting the study.
October 2016: After a trip to the Colombian Pacific region, the patient started to notice an increase in the number, distribution, and size of lesions. At first, he reported that 1 or 2 lesions would appear per week, but that as time passed this number increased to 30 or more per week. Also, not only the number of lesions appearing per week increased, but they started to appear in other regions of the scalp different than the occipital region, including the vertex an the temporal, and parietal regions. As a result of such an increase in the number of lesions and their wider distribution, e pain became almost unbearable, thus affecting his sleep habits and mood.
Late 2016: Given this situation, the patient scheduled a medical visit with a general physician who diagnosed him with bacterial folliculitis and started treatment consisting of doxycycline 200mg per os twice per day for 30 days, although he did not have a history of head shaving. In addition, the patient was referred to a dermatologist for further assessment, who agreed with continuing the initial antibiotic therapy for two more months, achieving the complete resolution of the existing lesions.
February 2017: Unfortunately, about two to three months after ending the doxycycline therapy, the lesions reappeared, so the patient scheduled another medical appointment with the same dermatologist and a new antibiotic treatment was started, this time consisting of oral trimethoprim/sulfamethoxazole 800mg/125mg twice a day for 15 days, topical mupirocin every 8 hours for 10 days and taking showers/baths with Kelual DS foaming gel (ciclopiroxolamine) and chlorhexidine 2 times per day for a month. As was the case with the initial suggested treatment, lesions disappeared, but they reappeared two to four months later.
June 2017: The patient reported that pain intensity and the number and size of lesions increased each time there was a relapse. Also, he said that some lesions were fusing together (3 to 5 at a time), and that he had observed alopecia in some areas. Likewise, he expressed having problems to sleep due to the pain caused by the lesions, as well as subsequent irritability and mood swings, which had a negative impact on his life both personally and the at the workplace. He also reported that his sister had started to experience similar signs and symptoms although less severely.
November 2017: Despite the reappearance of the lesions, no pharmacological treatment was prescribed by the dermatologist until a skin biopsy was performed, since folliculitis decalvans was suspected. The skin biopsy was performed using samples taken from two lesions (Figure 1B). Diagnosis was confirmed with biopsy report results (January 2018), in which the following findings were described: neutrophilic infiltrates, perifollicular fibrosis and polytrichia (no cultures were taken). Once the diagnosis was confirmed and routine laboratory tests were performed, that is, late January 2018, the patient was prescribed with oral isotretinoin therapy (20mg daily) for a year and a half due to his weight, as well as the use of topical fusidic acid 3 times per day for 2 weeks and taking baths with chlorhexidine 1 time per day for 1 month; he was also informed of some recommendations, such as stopping alcohol consumption altogether.
After treatment was started, the patient’s condition improved significantly as lesions and alopecia areas disappeared. However, he reported having an allergic reaction to fusidic acid, so its use was immediately suspended (Figure 1C). Approximately 4 months after the treatment was started, a new lesion appeared, but he opted for self-medication (a single dose of trimethoprim/sulfamethoxazole of 160/800mg), which caused a severe adverse reaction (fever, headache, and fatigue), so he suspended the use of this antibiotic; there were no more self-medication cases during the remaining of the treatment after it was finally completed. The results of the laboratory tests taken at different times (diagnosis and treatment over one year and a half), including those performed after the adverse reaction to trimethoprim/sulfamethoxazole occurred, are available in Table 2.
Table 2. Laboratory tests results of the patient.
|
Test |
13/01/2018 |
27/03/2018 |
17/06/2018† |
20/09/2018 |
09/07/2019 |
|
Creatinine urine test (mg/dL) |
0.85 |
0.83 |
No information |
No information |
0.73 |
|
Blood glucose test (mg/dL) |
92.00 |
92.30 |
99.00 |
no information |
99.26 |
|
Postprandial glucose test (mg/dL) |
No information |
No information |
115.03 |
no information |
No information |
|
Phosphatase alkaline test (U/L) |
No information |
86.10 |
No information |
87.50 |
No information |
|
Creatine phosphokinase (CPK) test (U/L) |
No information |
No information |
75.00Ŧ |
No information |
No information |
|
Lactic dehydrogenase test (U/L) |
No information |
No information |
161.30 |
No information |
No information |
|
Alanine Aminotransferase test (ALT) (U/L) |
21.60 |
25.90 |
41.40 * |
32.30 |
43.90 * |
|
Aspartate aminotransferase (AST) test(U/L) |
22.30 |
17.20 |
21.30 |
21.00 |
23.20 |
|
Total cholesterol test (mg/dL) |
191.50 |
No information |
196.50 |
179.10 |
172.3 |
|
High-Density Lipoprotein (HDL) Cholesterol Test (mg/dL) |
44.40 |
No information |
No information |
No information |
36.70 |
|
Low-density lipoprotein (LDL) test (mg/dL) |
125.08 |
No information |
No information |
No information |
110.15 * |
|
Triglycerides test (mg/dL) |
110.10 |
No information |
190.50 * |
209.00 ** |
130.39 |
|
Complete blood count |
Normal limits |
Normal limits |
No information |
No information |
Normal limits |
|
Urinalysis |
Normal limits |
No information |
No information |
No information |
Normal limits |
Comments:
* Outside normal reference values; slight increase in values.
** Outside normal reference values, significant increase in values.
† Prior to undergoing these tests, the patient self-medicated.
Ŧ There was no control CPK test, which is another limitation of the case presented here.
Source: own elaboration based on the data obtained from the patient’s medical record.
November 2019: Treatment was completed without any adverse effects. It should be noted that despite medical treatment was started relatively early and complete remission was achieved, there is always a possibility of relapse. A yearly timeline of the case is described in Table 3.
November 2021 (follow-up): The patient reported a mild relapse. However, lesions disappeared after he followed the recommendation of suspending the consumption of milk and other dairy products.
January 2022 (follow-up): According to the patient, lesions do not appear unless he consumes dairy products or derivatives, as they usually appear 2 to 3 days after he eats or drinks any of such products, but they disappear within 2 to 3 weeks after suspending said consumption. There was no sign of new lesions during this follow-up examination, and the patient claimed that he is doing his best to continue with a dairy-free diet.
Table 3. Timeline.
|
Year |
General |
Diagnosis |
Treatment |
Second treatment |
Relapse |
Comments |
Skin biopsy results |
|
2015 |
The first lesion appeared |
NA |
NA |
NA |
NA |
The patient did not report any travel |
N/A |
|
2016 |
Lesions continued to appear once or twice per week. After a trip to the Colombian Pacific region, the number and size of lesions appearing per week increased, as well as pain intensity |
NA |
NA |
NA |
NA |
The patient travelled to the Colombian Pacific Region (Guapi, Cauca) |
N/A |
|
Late 2016 |
The patient sought medical assistance |
Bacterial folliculitis |
Doxycycline 200mg po twice a day for 30 days, and then for 2 more months |
Trimethoprim sulfamethoxazole 800/125mg po twice a day for 15 days, topic mupirocin every 8 hours for 10 days, and 2 baths with Kelual DS and chlorhexidine 2 time per day for a month |
Yes, 2 to 3 months after completing each therapy |
N/A |
|
|
2017 - 2018 |
Patient continued attending follow-up visits with the Dermatology Service |
Folliculitis decalvans |
Isotretinoin 20mg po daily for 1 year and a half, topical fusidic acid and 3 times per day for 2 weeks and baths with chlorhexidine x times per day for 1 month |
NA |
NA |
Allergic reaction to fusidic acid, so it was suspended. Due to the appearance of a new single lesion the patient self- medicated with trimethoprim sulfamethoxazole 800/125mg; however, he experienced a severe adverse reaction and a slight increase in liver enzymes was evidenced. Isotretinoine is started. |
Yes, findings compatible with folliculitis decalvans |
|
2019 |
Complete remission |
Folliculitis decalvans |
|||||
|
2021 |
Mild relapse: smaller and sparser lesions |
Folliculitis decalvans |
No medication was started. The suspension of dairy products was ordered. |
N/A |
N/A |
N/A |
N/A |
|
2022 |
Remission. The patient is exercising and losing weight |
Folliculitis decalvans |
Dairy-free diet |
po: medication taken orally.
Source: own elaboration.
Discussion
Folliculitis decalvans is a rare type of primary cicatricial alopecia that mainly affects middle-aged males (18,19,20,21). In addition, although it has been described that S aureus infection might be a contributing factor, there is no clear evidence on its association with the occurrence of this disease (18,19,20,21). Most cases seem to be sporadic, and lesions mainly appear on the vertex. (20,21) Its diagnosis and treatment are a challenge since reaching a diagnosis may take several years and sometimes treatment needs to be extended due to folliculitis decalvans being refractory. (22)
In the case reported here, the information provided by the patient allowed the treating physician to make a rather fast diagnosis and start a timely treatment. The clinical manifestations of folliculitis decalvans described here are similar to what have been reported in other case reports (6,9). Likewise, as shown in other case reports (23), treatment with isotretinoin was successful in our case. Other therapeutic options include the use of biological drugs, (24,25) photodynamic therapy (20,21) and even YAG laser (26), especially in cases of recalcitrant folliculits decalvans.
Regarding prognostic factors for severe folliculitis decalvans, our patient presented with tufted hairs (polytrichia); besides it had an early onset (age < 25 years old) and had lasted several years. (20) As mentioned above, proper treatment of this condition has proven to be a challenge (1,7,12), as several therapies have been reported with a varying range of success; in this regard the main clinical characteristics of folliculitis decalvans, as well as some of the therapies described for its treatment (including doses) are available in Table 4. Other therapeutic alternatives include medical honey (27) and adipose tissue transplantation. (22) Primary scarring alopecia refers to a heterogeneous group of rare disorders in which hair follicles are destroyed irreversibly, (28) most of these disorders can be easily recognizable based on their clinical manifestations, however skin biopsies are useful for confirming the diagnosis. (29)
Table 4. Treatment options and main clinical characteristics of folliculitis decalvans and some other types of scarring alopecia.
|
Disease |
Clinical characteristics |
Treatment options |
|
Folliculitis decalvans |
It affects both men and women. |
Antimicrobial shampoo Isotretinoin Clarithromycin (4-8 weeks) Doxycycline (4-8 weeks) Clindamycin 300mg plus rifampicin 300mg for 6-12 weeks Dapsone 50mg for several years Removal of all tufted hair follicles to prevent recurrence. |
|
Intense granulocytic inflammation destroys the hair follicles and the skin of the scalp. |
||
|
Scarred and atrophic areas, together with severe inflammation are observed during physical inspections. |
||
|
Presence of tufted hairs (5-20), which act as a portal of entry for staphylococci. |
||
|
Perifolliculitis capitis abscedens et suffodiens |
It mainly affects men. |
Aspiration of nodules Injection of triamcinolone crystal suspension (10mg/mL) Systemic glucocorticoids (e.g., methylprednisolone) Isotretinoin |
|
Initial lesions are hemispherical, lividly inflamed, hairless, soft and fluctuant; they are located on the scalp. |
||
|
Bloody exudate is generally microbiologically sterile. In extreme cases the entire scalp is undermined by confluent inflammatory exudates. |
||
|
Lichen planopilaris |
A dense collection of T lymphocytes is found under the epidermal and follicular basal laminae. |
Class III or IV corticosteroids foams Retinoid actitretin Hydroxychloroquine |
|
Possible autoimmunity to unknown basement membrane antigen. Destruction of follicular stem cells. |
||
|
Physical inspection findings: small areas of alopecia with peripheral follicular hyperkeratosis. |
||
|
Hairs in the affected area seem to have a tight-fitting white collar. |
||
|
Lassueur-Graham-Little-Piccardi syndrome: characterized by the triad of patchy cicatricial alopecia of the scalp, nonscarring of the axilla and groin, and a follicular spinous papule on the body, scalp, or both. Dystrophic changes in fingernails and toenails. |
||
|
Frontal fibrosing alopecia (first described by Kosard) |
This disorder is considered a variant of lichen planopilaris |
Therapy analogous to that of lichen planus |
|
It almost exclusively affects elderly women; however, it can occur in men and women in the perimenopuse period. |
||
|
The loss of hair resembles the one observed in patients with androgenetic alopecia |
||
|
Perifollicular alopecia and hyperkeratosis can often be seen |
||
|
Often restricted to frontal regions |
||
|
Treatment options |
||
|
Option * |
Dosage or Combination |
|
|
Option 1 |
Doxycicline bid 100mg po per day for 3-6 months |
|
|
Option 2 |
Rifampicin 300 mg po for 3 months or Rifampicin and Cyndamicin 300mg bid for 10 weeks |
|
|
Option 3 |
Minocycline 100mg po per day for 3-6 months |
|
|
Option 4 |
Clarithromycin 250 mg bid × 3 months, acitretin 10 mg bid / qd × 1 month, rifampicin 300 mg bid × 1 month |
|
|
Option 5 |
Isotretinoin 0.2-0.5mg/kg po once a day for 6 months to a year |
|
|
Option 6 |
Cephalexin (500mg per os 3-4 times a day) + Intralesional triamcinolone + Clobetasol propionate lotion for 4 months to 4 years |
|
|
Option 7 |
Intralesional triamcinolone + clobetasol propionate lotion + (doxycycline 100mg bid, minocycline 100mg bid, or tetracycline 500mg bid) between 6 months to 4 years |
|
|
Option 8 |
Photodynamic therapy |
|
|
Option 9 |
Azithromycin 500mg po/day 3 times weekly for 3 months day |
|
|
Option 10 |
Dapsone 75-100mg po per day for 4-6 months |
|
bid: twice a day
po: medication taken orally
qd: every day
* There are many other therapeutic options available. Treatment of the disease is not clear, as it can last even years and there is not strong evidence supporting its implementation. (40)
Source: Own elaboration based on Powell et al. (6); Sillani et al. (9); Miguel-Gómez et al. (20); Tietze et al. (23); Trüeb (28); Wolff et al. (30); Stokmeier et al. (31); Bolz et al. (32); Kossard (33); Vaño-Galván et al. (34); Harries & Messenger (35); Le Cleach & Chosidow (36); Tan et al. (37); Miguel-Gomez et al. (21); Vaño-Galván et al. (2); Bunagan et al. (38); Aksoy et al. (39), and Rambhia et al. (40).
Although the use of isotretinoin is a valid therapeutic alternative for the treatment of folliculitis decalvans, it can cause several adverse effects on the skin and mucous membranes, as well as muscle and skeletal alterations; besides, its teratogenic effect may limit its usefulness. (22)
The management of folliculitis decalvans requires both patience and economic resources, for its treatment is lengthy, and the medications to be used may be expensive. In this regard, it has been estimated that a patient might spend as much as 80 sterling pounds per month ($99 USD) in medications and other products necessary for proper treatment. (20)
On the other hand, patients with this condition need to be aware of the importance of follow-up and their own responsibility in terms of adherence to treatment and the proper care of the lesions; for example, in the case of our patient, he was asked to completely stop drinking alcohol due to the metabolism of isotretinoin. Furthermore, patients must be informed that the possibility of relapse is always present, and that it may take years to achieve full remission (i.e., absence of folliculitis decalvans), or that even treatment will be needed the whole life; making this clear early is important because it may have a toll on the patient’s mental health. (20) Likewise, patients must be aware of the challenges of reaching a diagnosis, as folliculitis decalvans is not only a rare disorder, but there are also several differential diagnoses (Table 5).
Table 5. Differential diagnoses of scalp folliculitis.
|
Folliculitis and perifolliculitis |
|||||||
|
Infectious folliculitis or caused by infestations or Infections |
Non-infectious (folliculitis) |
Perifolliculitis |
|||||
|
Superficial (generally suppurating lesions) |
Deep (generally granulomatous lesions) |
Superficial (generally suppurative) |
Deep (generally granulomatous) |
Other possibilities (spongiotic folliculitis) |
Predominantly lymphocytic |
Predominantly granulomatous |
|
|
Fungi: Dermatophytes Pityrosporum Candida |
Demodicosis |
Acne vulgaris |
Acne vulgaris |
Pruritic folliculitis of pregnancy |
Keratosis pilaris atrophicans and Keratosis follicularis spinulosa decalvans |
Demodicosis |
Perioral dermatitis |
|
Bacteria: Bacteria (Impetigo of Bockhart) Secondary to Syphilis infection |
Favus and kerion |
Rosacea and perioral dermatitis |
Lupoid rosacea |
Fox-Fordyce disease |
Keratosis pilaris atrophicans |
Vitamin C deficiency |
Acneiform eruption secondary to syphilis |
|
Viruses: Herpes simplex virus Varicella zoster virus Molluscum contagiosum |
Tinea barbae |
Eosinophilic pustular folliculitis |
Acne conglobata |
Infundibulofolliculitis |
Lichen planopilaris |
Vitamin A deficiency |
|
|
Majocchi’s granuloma |
Toxic erythema of the newborn |
Keloidal acne of the neck |
Pityriasis rubra pilaris |
Lithium-induced folliculitis |
|||
|
Furuncle |
Follicular mucinosis |
Perforating folliculitis |
|||||
|
Carbuncle |
Mechanical and chemical traumas |
Toxicoderma: Halogens Lithium |
|||||
|
Sycosis |
Toxicoderma: Halogens Steroids |
Pseudofolliculitis |
|||||
|
Pustular acneiform Secondary syphilis |
Pseudofolliculitis |
||||||
Source: Own elaboration based on the paper by Lugovic-Mihic et al. (41), which in turn used information described by Camacho et al. (25)
One of the most important strengths of the case reported here is that the patient was referred to the dermatology service for conducting a comprehensive assessment consisting of a thorough clinical and physical examination and the performance of laboratory tests and a skin biopsy. On the other hand, this case has the following limitations: genetic and immunological aspects were not analyzed; the patient’s relatives were not assessed and tested and, therefore, it was not possible to confirm the presence of familiar cluster; there were no follow-up laboratory tests; and there were no photographs depicting the histopathological characteristics and clinical distribution of the lesions.
Conclusion
The case reported here clearly exposes the challenges that treating folliculitis decalvans and other types of primary cicatricial alopecia implies. In addition, this case is of great importance since, if further genetic testing is performed, the possible presence of a familial cluster of folliculitis decalvans could be confirmed. Furthermore, it was observed that although the patient had an adequate response to retinoid therapy, drug interactions must always be monitored to avoid the occurrence of adverse reactions, as happened when the patient self-medicated with trimethoprim sulfamethoxazole while taking isotretinoin, even though no adverse reactions were reported when such treatment was first implemented.
Ethical considerations
The patient signed a written informed consent form in which he agreed to the use of his clinical data and photographs for the publication of this case report. Data anonymity was ensured at all times.
Funding
None declared by the authors.
Conflict of interests
None declared by the authors.
1.Whiting DA. Cicatricial alopecia: clinico-pathological findings and treatment. Clin Dermatol. 2001;19(2):211-25. https://doi.org/brbth4.
2.Vañó-Galván S, Molina-Ruiz AM, Fernández-Crehuet P, Rodrigues-Barata A, Arias-Santiago S, Serrano-Falcón C, et al. Folliculitis decalvans: a multicentre review of 82 patients. J Eur Acad Dermatol Venereol. 2015;29(9):1750-7. https://doi.org/f8qkw9.
3.Olsen EA, Bergfeld WF, Cotsarelis G, Price VH, Shapiro J, Sinclair R, et al. Summary of North American Hair Research Society (NAHRS)-sponsored workshop on cicatricial alopecia, Duke university medical center, February 10 and 11, 2001. J Am Acad Dermatol. 2003;48(1):103-10. https://doi.org/bf2k5p.
4.Forman L. Folliculitis Decalvans (de Quinquad). J R Soc Med. 1943;36(6):295. https://doi.org/hfs9.
5.Otberg N, Kang H, Alzolibani AA, Shapiro J. Folliculitis decalvans. Dermatol Ther. 2008;21(4):238-44. https://doi.org/cxpbqd.
6.Powell JJ, Dawber RP, Gatter K. Folliculitis decalvans including tufted folliculitis: clinical, histological and therapeutic findings. Br J Dermatol. 1999;140(2):328-33. https://doi.org/d2w5bc.
7.Annessi G. Tufted folliculitis of the scalp: a distinctive clinicohistological variant of folliculitis decalvans. Br J Dermatol. 1998;138(5):799-805. https://doi.org/czj2q3.
8.Chandrawansa PH, Giam YC. Folliculitis decalvans-a retrospective study in a tertiary referred centre, over five years. Singapore Med J. 2003;44(2):84-7.
9.Sillani C, Bin Z, Ying Z, Zeming C, Jian Y, Xingqi Z. Effective treatment of folliculitis decalvans using selected antimicrobial agents. Int J Trichology. 2010;2(1):20-3. https://doi.org/frxqgr
10.Jaiswal AK, Vaishampayan S, Walia NS, Verma R. Folliculitis decalvans in a family. Indian J Dermatol Venereol Leprol. 2000;66(4):216-7.
11.Douwes KE, Landthaler M, Szeimies RM. Simultaneous occurrence of folliculitis decalvans capillitii in identical twins. Br J Dermatol. 2000;143(1):195-7. https://doi.org/fxf3hb.
12.Collier NJ, Allan D, Diaz-Pesantes F, Sheridan L, Allan E. Systemic photodynamic therapy in folliculitis decalvans. Clin Exp Dermatol. 2018;43(1):46-9. https://doi.org/hf5r.
13.Ross EK, Tan E, Shapiro J. Update on primary cicatricial alopecias. J Am Acad Dermatol. 2005;53(1):1-37. https://doi.org/dcm8sg.
14.Rudnicka L, Olszewska M, Rakowska A, Slowinska M. Trichoscopy update 2011. J Dermatol Case Rep. 2011;5(4):82-8. https://doi.org/dpjtvg.
15.Fabris MR, Melo CP, Melo DF. Folliculitis decalvans: the use of dermatoscopy as an auxiliary tool in clinical diagnosis. An Bras Dermatol. 2013;88(5):814-6. https://doi.org/gcbvdj.
16.Rakowska A, Stefanato C, Czuwara J, Olszewska M, Rudnicka L. Folliculitis Decalvans. In: Rudnicka L, Olszewska M, Rakowska A, editors. Atlas of Trichoscopy: Dermoscopy in Hair and Scalp Disease. London: Springer London; 2012. p. 319-29. https://doi.org/hf5s.
17.Inui S. Trichoscopy for common hair loss diseases: algorithmic method for diagnosis. J Dermatol. 2011;38(1):71-5. https://doi.org/dv3c65.
18.Chiarini C, Torchia D, Bianchi B, Volpi W, Caproni M, Fabbri P. Immunopathogenesis of folliculitis decalvans: clues in early lesions. Am J Clin Pathol. 2008;130(4):526-34. https://doi.org/c89hqh.
19.Brooke RC, Griffiths CE. Folliculitis decalvans. Clin Exp Dermatol. 2001;26(1):120-2. https://doi.org/dtppm8.
20.Miguel-Gómez L, Rodrigues-Barata AR, Molina-Ruiz A, Martorell-Calatayud A, Fernández-Crehuet P, Grimalt R, et al. Folliculitis decalvans: effectiveness of therapies and prognostic factors in a multicenter series of 60 patients with long-term follow-up. J Am Acad Dermatol. 2018;79(5):878-83. https://doi.org/gfhcjt.
21.Miguel-Gomez L, Vano-Galvan S, Perez-Garcia B, Carrillo-Gijon R, Jaen-Olasolo P. Treatment of folliculitis decalvans with photodynamic therapy: Results in 10 patients. J Am Acad Dermatol. 2015;72(6):1085-7. https://doi.org/f3gqdr.
22.Tedesco M. Adipose tissue transplant in recurrent folliculitis decalvans. Int J Immunopathol Pharmacol. 2018;32: 2058738418814688. https://doi.org/hf5v.
23.Tietze JK, Heppt MV, Von Preußen A, Wolf U, Ruzicka T, Wolff H, et al. Oral isotretinoin as the most effective treatment in folliculitis decalvans: a retrospective comparison of different treatment regimens in 28 patients. J Eur Acad Dermatol Venereol. 2015;29(9):1816-21. https://doi.org/f8qmt3.
24.Mihaljević N, von den Driesch P. Successful use of infliximab in a patient with recalcitrant folliculitis decalvans. J Deutsch Dermatol Ges. 2012;10(8):589-90. https://doi.org/hf5w.
25.Camacho F. Alopecias cicatriciales. En Tricología: Enfermedades del Folículo Pilosebáceo. 1996. Aula Medica Madrid.
26.Meesters AA, Van der Veen JP, Wolkerstorfer A. Long-term remission of folliculitis decalvans after treatment with the long-pulsed Nd:YAG laser. J Dermatolog Treat. 2014;25(2):167-8. https://doi.org/hf5x.
27.Yeh JE, Hartman RI, Xu J, Hoang M, Yasuda MR. Resolution of folliculitis decalvans with medical honey. Dermatol Online J. 2019;25(8):13030/qt07n6v0hs. https://doi.org/hf5z.
28.Trüeb R. [Cicatricial alopecias]. Hautarzt. 2013;64(11):810-9. https://doi.org/hf52.
29.Headington JT. Transverse microscopic anatomy of the human scalp: a basis for a morphometric approach to disorders of the hair follicle. Arch Dermatol. 1984;120(4):449-56. https://doi.org/dn4b97.
30.Wolff H, Fischer TW, Blume-Peytavi U. The diagnosis and treatment of hair and scalp diseases. Dtsch Ärztebl Int. 2016;113(21):377-86. https://doi.org/hf53.
31.Stockmeier M, Kunte C, Feldmann K, Messer G, Wolff H. Folliculitis decalvans-Behandlung mit einer systemischen Rifampicin-Clindamycin-Kombinationstherapie bei 17 Patienten. Akt Dermatol. 2001;27:361-3.
32.Bolz S, Jappe U, Hartschuh W. Successful treatment of perifolliculitis capitis abscedens et suffodiens with combined isotretinoin and dapsone. J Dtsch Dermatol Ges. 2008;6(1):44-7. https://doi.org/brqvgf
33.Kossard S. Postmenopausal frontal fibrosing alopecia: scarring alopecia in a pattern distribution. Arch Dermatol. 1994;130(6):770-4. https://doi.org/brzmrx.
34.Vañó-Galván S, Molina-Ruiz AM, Serrano-Falcón C, Arias-Santiago S, Rodrigues-Barata AR, Garnacho-Saucedo G, et al. Frontal fibrosing alopecia: a multicenter review of 355 patients. J Am Acad Dermatol. 2014;70(4):670-8. https://doi.org/f2q5f7.
35.Harries MJ, Messenger A. Treatment of frontal fibrosing alopecia and lichen planopilaris. J Eur Acad Dermatol Venereol. 2014;28(10):1404-5. https://doi.org/hf54.
36.Le Cleach L, Chosidow O. Clinical practice. Lichen planus. N Engl J Med. 2012;366(8):723-32. https://doi.org/gnz7w7.
37.an E, Martinka M, Ball N, Shapiro J. Primary cicatricial alopecias: clinicopathology of 112 cases. J Am Acad Dermatol. 2004;50(1):25-32. https://doi.org/d98scc.
38.Bunagan MJ, Banka N, Shapiro J. Retrospective review of folliculitis decalvans in 23 patients with course and treatment analysis of long-standing cases. J Cutan Med Surg. 2015;19(1):45-9. https://doi.org/f67rbq.
39.Aksoy B, Hapa A, Mutlu E. Isotretinoin treatment for folliculitis decalvans: a retrospective case-
series study. Int J Dermatol. 2018;57(2):250-3. https://doi.org/gcsxd5.
40.Rambhia PH, Conic RRZ, Murad A, Atanaskova-Mesinkovska N, Piliang M, Bergfeld W. Updates in therapeutics for folliculitis decalvans: A systematic review with evidence-based analysis. J Am Acad Dermatol. 2019;80(3):794-801. https://doi.org/hf56.
41.Lugović-Mihić L, Barisić F, Bulat V, Buljan M, Situm M, Bradić L, et al. Differential diagnosis of the scalp hair folliculitis. Acta Clin Croat. 2011;50(3):395-402.
Referencias
Whiting DA. Cicatricial alopecia: clinico-pathological findings and treatment. Clin Dermatol. 2001;19(2):211-25. https://doi.org/brbth4 .
Vañó‐Galván S, Molina‐Ruiz AM, Fernández‐Crehuet P, Rodrigues‐Barata A, Arias‐Santiago S, Serrano‐Falcón C, et al. Folliculitis decalvans: a multicentre review of 82 patients. J Eur Acad Dermatol Venereol. 2015;29(9):1750-7. https://doi.org/f8qkw9 .
Olsen EA, Bergfeld WF, Cotsarelis G, Price VH, Shapiro J, Sinclair R, et al. Summary of North American Hair Research Society (NAHRS)-sponsored workshop on cicatricial alopecia, Duke university medical center, February 10 and 11, 2001. J Am Acad Dermatol. 2003;48(1):103-10. https://doi.org/bf2k5p .
Forman L. Folliculitis Decalvans (de Quinquad). J R Soc Med. 1943;36(6):295. https://doi.org/hfs9 .
Otberg N, Kang H, Alzolibani AA, Shapiro J. Folliculitis decalvans. Dermatol Ther. 2008;21(4):238-44. https://doi.org/cxpbqd .
Powell JJ, Dawber RP, Gatter K. Folliculitis decalvans including tufted folliculitis: clinical, histological and therapeutic findings. Br J Dermatol. 1999;140(2):328-33. https://doi.org/d2w5bc .
Annessi G. Tufted folliculitis of the scalp: a distinctive clinicohistological variant of folliculitis decalvans. Br J Dermatol. 1998;138(5):799-805. https://doi.org/czj2q3 .
Chandrawansa PH, Giam YC. Folliculitis decalvans a retrospective study in a tertiary referred centre, over five years. Singapore Med J. 2003;44(2):84-7.
Sillani C, Bin Z, Ying Z, Zeming C, Jian Y, Xingqi Z. Effective treatment of folliculitis decalvans using selected antimicrobial agents. Int J Trichology. 2010;2(1):20-3. https://doi.org/frxqgr
Jaiswal AK, Vaishampayan S, Walia NS, Verma R. Folliculitis decalvans in a family. Indian J Dermatol Venereol Leprol. 2000;66(4):216-7.
Douwes KE, Landthaler M, Szeimies RM. Simultaneous occurrence of folliculitis decalvans capillitii in identical twins. Br J Dermatol. 2000;143(1):195-7. https://doi.org/fxf3hb .
Collier NJ, Allan D, Diaz-Pesantes F, Sheridan L, Allan E. Systemic photodynamic therapy in folliculitis decalvans. Clin Exp Dermatol. 2018;43(1):46-9. https://doi.org/hf5r .
Ross EK, Tan E, Shapiro J. Update on primary cicatricial alopecias. J Am Acad Dermatol. 2005;53(1):1-37. https://doi.org/dcm8sg .
Rudnicka L, Olszewska M, Rakowska A, Slowinska M. Trichoscopy update 2011. J Dermatol Case Rep. 2011;5(4):82-8. https://doi.org/dpjtvg .
Fabris MR, Melo CP, Melo DF. Folliculitis decalvans: the use of dermatoscopy as an auxiliary tool in clinical diagnosis. An Bras Dermatol. 2013;88(5):814-6. https://doi.org/gcbvdj .
Rakowska A, Stefanato C, Czuwara J, Olszewska M, Rudnicka L. Folliculitis Decalvans. In: Rudnicka L, Olszewska M, Rakowska A, editors. Atlas of Trichoscopy: Dermoscopy in Hair and Scalp Disease. London: Springer London; 2012. p. 319-29. https://doi.org/hf5s .
Inui S. Trichoscopy for common hair loss diseases: algorithmic method for diagnosis. J Dermatol. 2011;38(1):71-5. https://doi.org/dv3c65 .
Chiarini C, Torchia D, Bianchi B, Volpi W, Caproni M, Fabbri P. Immunopathogenesis of folliculitis decalvans: clues in early lesions. Am J Clin Pathol. 2008;130(4):526-34. https://doi.org/c89hqh .
Brooke RC, Griffiths CE. Folliculitis decalvans. Clin Exp Dermatol. 2001;26(1):120-2. https://doi.org/dtppm8 .
Miguel-Gómez L, Rodrigues-Barata AR, Molina-Ruiz A, Martorell-Calatayud A, Fernández-Crehuet P, Grimalt R, et al. Folliculitis decalvans: effectiveness of therapies and prognostic factors in a multicenter series of 60 patients with long-term follow-up. J Am Acad Dermatol. 2018;79(5):878-83. https://doi.org/gfhcjt .
Miguel-Gomez L, Vano-Galvan S, Perez-Garcia B, Carrillo-Gijon R, Jaen-Olasolo P. Treatment of folliculitis decalvans with photodynamic therapy: Results in 10 patients. J Am Acad Dermatol. 2015;72(6):1085-7. https://doi.org/f3gqdr .
Tedesco M. Adipose tissue transplant in recurrent folliculitis decalvans. Int J Immunopathol Pharmacol. 2018;32: 2058738418814688. https://doi.org/hf5v .
Tietze JK, Heppt MV, Von Preußen A, Wolf U, Ruzicka T, Wolff H, et al. Oral isotretinoin as the most effective treatment in folliculitis decalvans: a retrospective comparison of different treatment regimens in 28 patients. J Eur Acad Dermatol Venereol. 2015;29(9):1816-21. https://doi.org/f8qmt3 .
Mihaljević N, von den Driesch P. Successful use of infliximab in a patient with recalcitrant folliculitis decalvans. J Deutsch Dermatol Ges. 2012;10(8):589-90. https://doi.org/hf5w .
Camacho F. Alopecias cicatriciales. En Tricología: Enfermedades del Folículo Pilosebáceo. 1996. Aula Medica Madrid.
Meesters AA, Van der Veen JP, Wolkerstorfer A. Long-term remission of folliculitis decalvans after treatment with the long-pulsed Nd:YAG laser. J Dermatolog Treat. 2014;25(2):167-8. https://doi.org/hf5x .
Yeh JE, Hartman RI, Xu J, Hoang M, Yasuda MR. Resolution of folliculitis decalvans with medical honey. Dermatol Online J. 2019;25(8):13030/qt07n6v0hs. https://doi.org/hf5z .
Trüeb R. [Cicatricial alopecias]. Hautarzt. 2013;64(11):810-9. https://doi.org/hf52 .
Headington JT. Transverse microscopic anatomy of the human scalp: a basis for a morphometric approach to disorders of the hair follicle. Arch Dermatol. 1984;120(4):449-56. https://doi.org/dn4b97 .
Wolff H, Fischer TW, Blume-Peytavi U. The diagnosis and treatment of hair and scalp diseases. Dtsch Ärztebl Int. 2016;113(21):377-86. https://doi.org/hf53 .
Stockmeier M, Kunte C, Feldmann K, Messer G, Wolff H. Folliculitis decalvans-Behandlung mit einer systemischen Rifampicin-Clindamycin-Kombinationstherapie bei 17 Patienten. Akt Dermatol. 2001;27:361-3. DOI: https://doi.org/10.1055/s-2001-19129
Bolz S, Jappe U, Hartschuh W. Successful treatment of perifolliculitis capitis abscedens et suffodiens with combined isotretinoin and dapsone. J Dtsch Dermatol Ges. 2008;6(1):44-7. https://doi.org/brqvgf
Kossard S. Postmenopausal frontal fibrosing alopecia: scarring alopecia in a pattern distribution. Arch Dermatol. 1994;130(6):770-4. https://doi.org/brzmrx .
Vañó-Galván S, Molina-Ruiz AM, Serrano-Falcón C, Arias-Santiago S, Rodrigues-Barata AR, Garnacho-Saucedo G, et al. Frontal fibrosing alopecia: a multicenter review of 355 patients. J Am Acad Dermatol. 2014;70(4):670-8. https://doi.org/f2q5f7 .
Harries MJ, Messenger A. Treatment of frontal fibrosing alopecia and lichen planopilaris. J Eur Acad Dermatol Venereol. 2014;28(10):1404-5. https://doi.org/hf54 .
Le Cleach L, Chosidow O. Clinical practice. Lichen planus. N Engl J Med. 2012;366(8):723-32. https://doi.org/gnz7w7 .
Tan E, Martinka M, Ball N, Shapiro J. Primary cicatricial alopecias: clinicopathology of 112 cases. J Am Acad Dermatol. 2004;50(1):25-32. https://doi.org/d98scc .
Bunagan MJ, Banka N, Shapiro J. Retrospective review of folliculitis decalvans in 23 patients with course and treatment analysis of long-standing cases. J Cutan Med Surg. 2015;19(1):45-9. https://doi.org/f67rbq .
Aksoy B, Hapa A, Mutlu E. Isotretinoin treatment for folliculitis decalvans: a retrospective case‐series study. Int J Dermatol. 2018;57(2):250-3. https://doi.org/gcsxd5 .
Rambhia PH, Conic RRZ, Murad A, Atanaskova-Mesinkovska N, Piliang M, Bergfeld W. Updates in therapeutics for folliculitis decalvans: A systematic review with evidence-based analysis. J Am Acad Dermatol. 2019;80(3):794-801. https://doi.org/hf56 .
Lugović-Mihić L, Barisić F, Bulat V, Buljan M, Situm M, Bradić L, et al. Differential diagnosis of the scalp hair folliculitis. Acta Clin Croat. 2011;50(3):395-402.
Cómo citar
APA
ACM
ACS
ABNT
Chicago
Harvard
IEEE
MLA
Turabian
Vancouver
Descargar cita
Licencia
Derechos de autor 2022 Case reports

Esta obra está bajo una licencia internacional Creative Commons Atribución 4.0.
Los autores al someter sus manuscritos conservarán sus derechos de autor. La revista tiene el derecho del uso, reproducción, transmisión, distribución y publicación en cualquier forma o medio. Los autores no podrán permitir o autorizar el uso de la contribución sin el consentimiento escrito de la revista.
El Formulario de Divulgación Uniforme para posibles Conflictos de Interés y los oficios de cesión de derechos y de responsabilidad deben ser entregados junto con el original.
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as conservarán sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cual estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons 4.0 que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los autores/as podrán adoptar otros acuerdos de licencia no exclusiva de distribución de la versión de la obra publicada (p. ej.: depositarla en un archivo telemático institucional o publicarla en un volumen monográfico) siempre que se indique la publicación inicial en esta revista.
Se permite y recomienda a los autores/as difundir su obra a través de Internet (p. ej.: en archivos telemáticos institucionales o en su página web) antes y durante el proceso de envío, lo cual puede producir intercambios interesantes y aumentar las citas de la obra publicada. (Véase El efecto del acceso abierto).