Reporte de un caso de síndrome de Sagliker, una complicación de la enfermedad renal crónica que debe ser reconocida y prevenida
Sagliker syndrome, a complication of chronic kidney disease that must be recognized and prevented: case report
DOI:
https://doi.org/10.15446/cr.v9n1.94227Palabras clave:
Hiperparatiroidismo secundario, Insuficiencia renal crónica, Anomalías maxilofaciales, Anomalías musculoesqueléticas (es)Hyperparathyroidism, Secondary, Kidney Failure, Chronic, Maxillofacial Abnormalities, Musculoskeletal Abnormalities (en)
Descargas
Resumen
Introducción. Durante las últimas dos décadas se ha descrito una población, hasta ahora pequeña, de pacientes con enfermedad renal crónica que presentan cambios físicos y comportamentales. En estos pacientes, que particularmente son de bajo nivel socioeconómico y tienen una pobre red de apoyo familiar, las deformidades óseas se relacionan con presencia de hiperparatiroidismo secundario con un consecuente compromiso osteomuscular. El conjunto de estos cambios se define como síndrome de Sagliker (SS). El presente reporte constituye el segundo caso de esta naturaleza publicado en Colombia.
Presentación del caso. Hombre de 35 años con enfermedad renal crónica terminal en hemodiálisis, quien desarrolló hiperparatiroidismo secundario que generó alteraciones en el metabolismo mineral óseo. Este compromiso produjo limitación funcional y deformidad facial y corporal debido a múltiples fracturas patológicas y a la aparición de tumores pardos. Las características físicas, así como los hallazgos en estudios de imagen y laboratorios, permitieron llegar al diagnóstico de SS.
Conclusión. El SS es una enfermedad rara de la que aún existe un conocimiento limitado; sin embargo, la detección temprana de compromiso renal y un manejo integral y oportuno pueden prevenir las complicaciones y el deterioro en la calidad de vida de los pacientes con esta condición.
Abstract
Introduction: Over the last two decades, a small population of patients with chronic kidney disease who present with physical and behavioral changes has been described. In these patients, who usually have a low socioeconomic status and a poor family support network, bone deformities are related to the presence of secondary hyperparathyroidism and consequent musculoskeletal involvement. These changes together are known as Sagliker syndrome (SS). The present report is the second case of this nature published in Colombia.
Case presentation: A 35-year-old man with end-stage chronic kidney disease on hemodialysis developed secondary hyperparathyroidism, which generated alterations in bone mineral metabolism. This resulted in functional limitation and facial and body deformity due to multiple pathologic fractures and the appearance of brown tumors. These physical characteristics, as well as the findings on imaging and laboratory studies, led to the diagnosis of SS.
Conclusion: SS is a rare disease about which knowledge is still limited. Early detection of kidney involvement and timely comprehensive management of the disease can prevent complications and deterioration in the quality of life of these patients.
https://doi.org/10.15446/cr.v9n1.94227
Sagliker syndrome, a complication of chronic kidney disease that must be recognized and prevented: case report
Keywords: Hyperparathyroidism, Secondary; Kidney Failure, Chronic;
Maxillofacial Abnormalities; Musculoskeletal Abnormalities.
Palabras clave: Hiperparatiroidismo secundario; Insuficiencia renal crónica;
Anomalías maxilofaciales; Anomalías musculoesqueléticas.
Andrés Felipe Mejía-Cardona
Wilfredo Antonio Rivera-Martínez
Universidad Libre de Colombia
- Faculty of Medicine -
Department of Internal Medicine
- Cali - Colombia.
Luis Alfonso Valderrama-Cometa
Clínica Imbanaco
- Department of Nephrology -
Cali - Colombia.
Corresponding author
Andrés Felipe Mejía-Cardona. Facultad de Medicina, Universidad Libre de Colombia. Cali. Colombia.
Email: andres.f.mejia@hotmail.com
Received: 10/03/2021 Accepted: 22/06/2021
Resumen
Introducción. Durante las últimas dos décadas se ha descrito una población, hasta ahora pequeña, de pacientes con enfermedad renal crónica que presentan cambios físicos y comportamentales. En estos pacientes, que particularmente son de bajo nivel socioeconómico y tienen una pobre red de apoyo familiar, las deformidades óseas se relacionan con presencia de hiperparatiroidismo secundario con un consecuente compromiso osteomuscular. El conjunto de estos cambios se define como síndrome de Sagliker (SS). El presente reporte constituye el segundo caso de esta naturaleza publicado en Colombia.
Presentación del caso. Hombre de 35 años con enfermedad renal crónica terminal en hemodiálisis, quien desarrolló hiperparatiroidismo secundario que generó alteraciones en el metabolismo mineral óseo. Este compromiso produjo limitación funcional y deformidad facial y corporal debido a múltiples fracturas patológicas y a la aparición de tumores pardos. Las características físicas, así como los hallazgos en estudios de imagen y laboratorios, permitieron llegar al diagnóstico de SS.
Conclusión. El SS es una enfermedad rara de la que aún existe un conocimiento limitado; sin embargo, la detección temprana de compromiso renal y un manejo integral y oportuno pueden prevenir las complicaciones y el deterioro en la calidad de vida de los pacientes con esta condición.
Abstract
Introduction: Over the last two decades, a small population of patients with chronic kidney disease who present with physical and behavioral changes has been described. In these patients, who usually have a low socioeconomic status and a poor family support network, bone deformities are related to the presence of secondary hyperparathyroidism and consequent musculoskeletal involvement. These changes together are known as Sagliker syndrome (SS). The present report is the second case of this nature published in Colombia.
Case presentation: A 35-year-old man with end-stage chronic kidney disease on hemodialysis developed secondary hyperparathyroidism, which generated alterations in bone mineral metabolism. This resulted in functional limitation and facial and body deformity due to multiple pathologic fractures and the appearance of brown tumors. These physical characteristics, as well as the findings on imaging and laboratory studies, led to the diagnosis of SS.
Conclusion: SS is a rare disease about which knowledge is still limited. Early detection of kidney involvement and timely comprehensive management of the disease can prevent complications and deterioration in the quality of life of these patients.
Introduction
Secondary hyperparathyroidism (SH) is a serious complication that can occur in stages 3, 4 and 5 of chronic kidney disease (CKD) (1). Biochemical changes associated with this condition are progressive and are initially characterized by elevated levels of fibroblast growth factor 23 (FGF23) and serum phosphorus (>4.5 mg/dL), concomitant decreased calcium levels (<8.5 mg/dL), and vitamin D deficiency (1-4). Finally, there is an increase in the concentrations of intact parathyroid hormone (iPTH) and, as a result of this variation, severe changes are produced in bone structures, mainly in long bones, vertebral bones, skull and facial bones; occasionally, brown tumors appear, which are lesions caused by a rapid osteoclastic activity (4,5).
Sagliker syndrome (SS) is a group of craniofacial and skeletal alterations associated with SH. It was first described in 2004 by Sagliker et al. (6) in a study involving 25 patients from different hemodialysis centers in Turkey who had CKD, SH, and facial deformities as a pathognomonic feature, further defining it as a very severe and almost untreatable condition (6). Anatomical changes in SS are manifested to varying degrees in the face and range from benign soft tissue hyperplasia to severe abnormalities of the skull, maxilla, jaw, and teeth. The phenotype of these patients also includes short stature; fingertip lesions; deformity of knees and scapulae; hearing loss; and severe neurological and psychological problems, including depression and cognitive impairment (2,7).
It has been established that the development of SS in patients with CKD is an indication of uncontrolled SH and that changes in physical appearance and musculoskeletal function caused by it are not reversible, even after kidney transplant, thus potentially affecting patients’ mental health and quality of life. Therefore, more care is needed in the management of SH, especially in early stages, in order to prevent the development of such sequelae (8).
The following is a description of the second known case of SS in Colombia.
Case presentation
A 35-year-old man from Cali (Colombia), mestizo, with a low socioeconomic status and fragmented family nucleus, consulted the emergency department of a quaternary care center in Cali after falling from his own height, which caused him pain and functional limitation in his left arm, leading to the identification of some deformities. His medical records revealed that he had been suffering from chronic bone pain for two years, primarily in his ribs, left knee, and hip, causing him difficulty walking and requiring the use of crutches for mobility.
The patient had a history of CKD stage 5D of unidentified origin and was on hemodialysis (HD) 3 times a week since 2011. He also suffered from arterial hypertension since the age of 25 years and had a history of moderate-severe hearing loss for 6 years. No hematuria was reported. At the age of 32, he required osteosynthesis due to a fracture of the left hip caused by a fall from a motorcycle, which also caused a gait disorder.
On admission, there was evidence of a deformity in the middle third of the left arm with circumscribed hematoma and limitation of proximal mobility. An X-ray of the left humerus showed two traces of fracture, one at the junction of the neck and humeral head, and the other in the middle third of the diaphysis (Figure 1).

Figure 1. X-ray of the left humerus showing a slightly oblique fracture in the middle third of the humeral diaphysis and a radiolucent image in the same location, as well as a fracture at the junction of the neck and the humeral head.
Source: Image obtained while conducting the study.
On the same day of admission, the patient was assessed by the orthopedics department, which, given the suspicion of a pathological fracture secondary to bone mineral disease due to CKD, requested additional studies. The long bone x-ray, performed on the second day of hospital stay, showed alteration of bone density, generalized thickening of the cortical bone, a radiolucent image in the diaphysis of the left tibia, and similar diffuse images in the upper, middle and lower third of the right tibia due to a bone infiltrative process. Small lesions of lower density with slight thickening of the cortical bone were observed in the skull.
The patient was evaluated by the nephrology service on the fifth day of hospitalization. During his physical examination, coarse facies, collapse of the nasal dorsum, symmetrical protrusion of the maxillary and mandibular bones, malocclusion, tumors on the floor of the mouth, irregular teeth, short neck, and increase in the anterosuperior diameter of the thorax were found. These alterations were the result of the physical changes that the patient started to exhibit 5 years earlier (Figure 2).
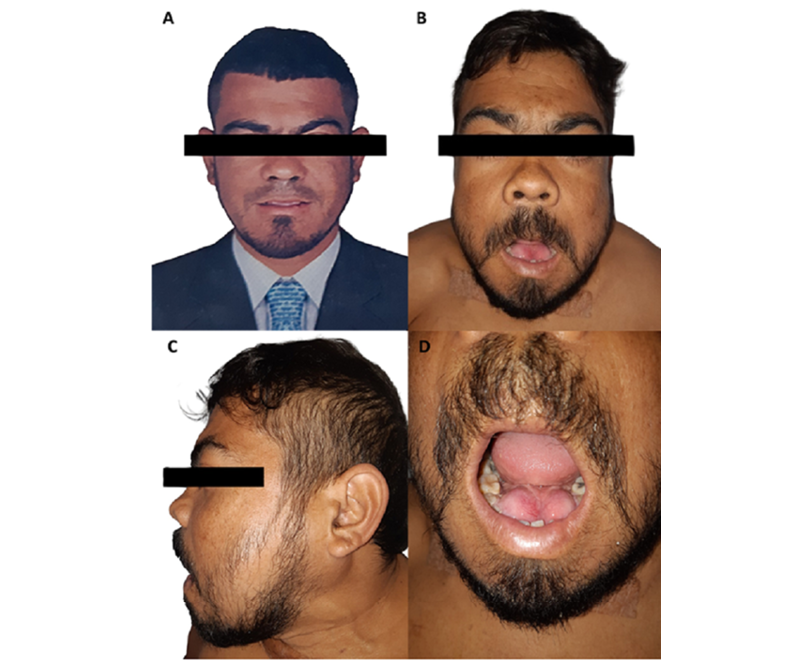
Figure 2. A) Physical appearance of the patient five years earlier; B) and C) Physical appearance of the patient at present; D) Tumors on the floor of the mouth.
Source: Images obtained while conducting the study.
Laboratory studies performed on the sixth day of hospitalization showed normocytic and normochromic anemia in blood count; elevated levels of iPTH (3899 pg/mL), alkaline phosphatase (1.305 U/I), potassium (5.9 mmol/L) and phosphorus (6.5 mg/dL), as well as ionic calcium (1.16 mmol/L) and thyroid profile in normal ranges.
On the 10th day of hospital stay, a parathyroid scan was requested, which showed a focal deposit of activity adjacent to the right lower pole of the thyroid gland, a 17mm nodular lesion of soft tissue density compatible with parathyroid adenoma, and multiple osteolytic lesions involving the mandible, both jaws, ribs, sternum, humerus, cervical spine and thorax; some of them were brown tumors (Figure 3).
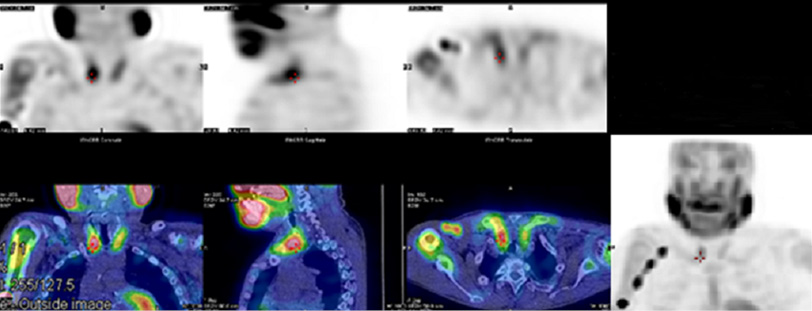
Figure 3. Parathyroid scintigraphy.
Source: Image obtained while conducting the study.
Given the findings and the history of terminal CKD on hemodialysis, SH, moderate-severe hypoacusis, pathological fractures and phenotypic changes, the nephrology service made the diagnosis of SS. In order to avoid the progression of bone deformities and reduce the risk of fractures caused by this disease, on the 15th day of hospitalization the patient underwent a parathyroidectomy leaving a remnant of the left lower parathyroid. Surgical findings included enlarged glands. Histopathology reported parathyroid hyperplasia.
In the immediate postoperative period, the patient developed hungry bone syndrome (HBS), requiring management in the intensive care unit (ICU) with intravenous calcium gluconate infusion at a dose of 50mg of elemental calcium per hour for 10 days. Despite this treatment, after 2 days in the ICU, hypocalcemia persisted with ionic calcium levels at 0.5 mmol/L, so oral calcium was added (calcium carbonate 1 200 mg/day), the infusion of elemental calcium was increased to 250 mg/h, and calcitriol was started at a dose of 0.5 mcg/day (active metabolite of vitamin D). With this treatment regimen, ionic calcium levels >1mmol/L were achieved on postoperative day 10.
The patient did not present tetany or arrhythmia, and after being stabilized, intravenous calcium infusion was suspended and he was transferred to the hospital ward, where he exhibited inappropriate behaviors characterized by aggressiveness, emotional lability, poor introspection of his illness, and poor adherence to in-hospital treatment. Consequently, he was assessed by the psychiatry service, which diagnosed sleep disorder, anxiety and impulsivity associated with cluster B personality disorders, and indicated hypnotic therapy with trazodone 50mg at night until his discharge.
The patient was discharged after 32 days of hospital stay with adequate tolerance and response to therapeutic measures. Outpatient follow-up tests showed that calcium, phosphorus and iPTH levels remained normal.
Discussion
SS is considered to be the result of undertreatment of SH in the early stages of CKD. This syndrome is usually reported in developing countries, where people lack access to necessary medical services and do not receive timely treatment for kidney failure and related complications (1,9). The exact cause of this condition is unknown, since not all patients with CKD and severe hyperparathyroidism develop it (10).
In 2012, Yildiz et al. (11) published a study in which they evaluated 23 patients with SS from different countries, as well as their first-degree blood relatives. In this evaluation, the investigators performed several studies in search of a probable etiology or a clearer predisposing factor, but did not find alterations in growth hormone, sex hormones or thyroid hormone, nor did they find alterations in hemoglobin electrophoresis or chromosomal abnormalities in cytogenetic studies, or in exons 2 and 3 of the CaSR gene. However, they found some mutations in the GNAS1 gene located on chromosome 20q13 in 40% of the patients and concluded that the findings of these mutations should be considered in the origin of SS. These mutations have also been associated with hereditary bone dystrophies (achondroplasias, such as McCune-Albright syndrome) (11).
Later, in 2015, Demirhan et al. (10) published a study in which, like Yildiz et al. (11), they included 23 patients from different parts of the world and their first-degree relatives. In their study, Demirhan et al. (10) performed cytogenetic and gene analyses for the calcium-sensitive receptor, for the GNAS1 and FGF-23 genes, and for fibroblast growth factor receptor 3, finding multiple genetic alterations that led them to conclude that patients with SS, despite having no resemblance to patients with hereditary bone dysplasia, could be located in between as a combination of CKD-related osteodystrophy and hereditary bone dysplasia.
The studies performed on the patient reported in this case did not reveal any endocrine disorders, and there was no family history that would allow the identification of a specific inheritance pattern. Thus, it was not possible to establish a specific causal agent in this subject, since the natural history of his disease began with a bone mineral disorder derived from his CKD on hemodialysis.
Regarding its clinical presentation, extraosseous clinical manifestations have been frequently documented. In a study performed in 10 patients with SS of multifactorial origin, Erkan et al. (7) reported hearing loss in 60% of the cases, this being one of the most important manifestations in the clinical presentation of the patient reported in the present study. Similarly, Ozenli et al. (12) conducted a study with 26 patients [13 with CKD and SS (study group) and 13 with CKD (control group)], in which they found a higher prevalence of mental illness in the study group (6.2% vs. 23.1%), mostly depressive disorder. In the present case, the patient had frequent episodes of agitation and anxiety, a sleep disorder, and cluster B personality disorders.
Early diagnosis of SS is of great importance, as it can help slow the progression of its consequences by modifying the risk factors that cause it, including anemia, hypocalcemia, hyperphosphatemia, vitamin D deficiency, and SH. However, once all its manifestations have been established, little can be done to improve the patients’ situation, as almost none of the bone changes are reversible (13).
The main causes of SS are poor management of CKD and SH in the presence of a genetic predisposition given by an associated mutation. Thus, if the bone mineral disease is not treated in a timely manner, it is very likely to progress to SS, which could be considered more common in individuals with limited resources and social constraints for access to available therapies, as described in some reports (8). That relationship was evident in the present case, which also shows how these social risk factors had an impact on the progression of the condition.
In a series of five cases, Mejía-Pineda et al. (9) described how parathyroidectomy improves the biochemical profile in phosphorus, calcium and hormone levels, and alleviates the depressive disorder suffered by these patients prior to the surgical procedure, so it has been suggested that this intervention is indicated in cases of SS. Nevertheless, since it has not been established whether iPTH production decreases or the progression of facial and body deformities is limited in cases presenting with this complication, the need for intervention is not clear in all patients (9).
HBS should be taken into account as a serious postoperative complication, mainly related to the magnitude of SH and the severity of bone involvement (elevated alkaline phosphatase, bone pain and radiological alterations). This condition is characterized by a decrease in bone resorption induced by iPTH while osteoblastic activity persists, producing an increase in bone uptake of calcium, phosphorus and magnesium, leading to severe hypocalcemia and its complications (14). HBS was detected and treated promptly in the present case, but despite preventive management with calcium infusion, severe hypocalcemia was documented without neurological repercussions, although the patient responded adequately to treatment adjustment. A patient with SS meets all the predictors or risk factors for the development of HBS, so recognizing it if it presents in the immediate postoperative period is essential to treat it early.
It is very likely that there are many undetected SS patients, particularly in developing countries, where SH therapy is not optimal, but it is also possible in developed countries, where no restrictions on therapy exist, but poor adherence to treatment may occur. A global incidence for SS has not been reported so far, although it was established to be approximately 0.5% in Turkey due to the detection of 25 patients with this condition in a population of 5 000 patients in hemodialysis centers (6).
The late diagnosis in the present case was a limitation that prevented a better clinical response to treatment by the patient, resulting in irreversible changes that were not amenable to intervention. In addition, neuropsychiatric alterations contributed to the lack of adherence to therapeutic measures, a factor that was also associated with a delay in the recovery process.
Conclusion
SS is a very rare condition that can and should be prevented, so it is necessary to objectively identify the risk factors, whether psychosocial, environmental or genetic, taking into account that it appears to be a multifactorial entity and does not develop in all patients in the same way. In this sense, it is necessary to continue providing data on this disorder, which considerably affects the quality of life of those who suffer from it and also increases the morbidity and mortality of patients with CKD.
Ethical considerations
This article was prepared after obtaining the patient’s informed consent to treat and disclose his medical history for scientific and academic purposes.
Conflicts of interest
None stated by the authors.
Funding
None stated by the authors.
Acknowledgments
None stated by the authors.
References
1.Sagliker Y, Acharya V, Ling Z, Golea O, Sabry A, Eyupoglu K, et al. International Study on Sagliker Syndrome and Uglifying Human Face Appearence in Severe and Late Secondary Hyperparathyroidism in Chronic Kidney Disease Patients. J Ren Nutr. 2008;18(1):114-7. https://doi.org/dffc2p.
2.Uzel A, Uzel I, Sagliker Y, Yildiz I, Halvaci I, Paylar N, et al. Cephalometric Evaluation of Patients With Sagliker Syndrome: Uglifying Human Face Appearance in Severe and Late Secondary Hyperparathyroidism in Chronic Renal Failure Patients. J Ren Nutr. 2006;16(3):229-32. https://doi.org/d9ffrq.
3.Fordham CC, Williams TF. Brown Tumor and Secondary Hyperparathyroidism. N Engl J Med. 1963;269(3):129-31. https://doi.org/bm8zks.
4.Hou YC, Lu CL, Lu KC. Mineral bone disorders in chronic kidney disease. Nephrology. 2018;23(4):88-94. https://doi.org/gftd3b.
5.Queiroz IV, Queiroz SP, Medeiros R, Ribeiro RB, Crusoé-Rebello IM, Leão JC. Brown tumor of secondary hyperparathyroidism: surgical approach and clinical outcome. Oral Maxillofac Surg. 2016;20(4):435-9. https://doi.org/kcx8.
6.Sagliker Y, Balal M, Sagliker-Ozkaynak P, Paydas S, Sagliker C, Sabit Sagliker H, et al. Sagliker syndrome: Uglifying human face appearance in late and severe secondary hyperparathyroidism in chronic renal failure. Semin Nephrol.2004;24(5):449-55. https://doi.org/fjhtb6.
7.Erkan AN, Sagliker Y, Yildiz I, Ozluoglu L. Audiological Findings in Chronic Kidney Disease Patients With Sagliker Syndrome. J Ren Nutr. 2010;20(5):S56-8. https://doi.org/bpgsxt.
8.Mohebi-Nejad A, Gatmiri SM, Abooturabi SM, Hemayati R, Mahdavi-Mazdeh M. Diagnosis and treatment of Sagliker syndrome: a case series from Iran. Iran J Kidney Dis. 2014;8(1):76-80.
9.Mejía-Pineda A, Aguilera ML, Meléndez HJ, Lemus JA, Peñalonzo MA. Sagliker syndrome in patients with secondary hyperparathyroidism and chronic renal failure: Case report. Int J Surg Case Rep. 2015;8C:127-30. https://doi.org/kcx3.
10. Demirhan O, Arslan A, Sagliker Y, Akbal E, Ergun S, Bayraktar R, et al. Gene mutations in chronic kidney disease patients with secondary hyperparathyroidism and sagliker syndrome. J Ren Nutr. 2015;25(2):176-86. https://doi.org/f627qp
11. Yildiz I, Sagliker Y, Demirhan O, Tunc E, Inandiklioglu N, Tasdemir D, et al. International Evaluation of Unrecognizably Uglifying Human Faces in Late and Severe Secondary Hyperparathyroidism in Chronic Kidney Disease. Sagliker Syndrome. A Unique Catastrophic Entity, Cytogenetic Studies for Chromosomal Abnormalities, Calcium-Sensing Receptor Gene and GNAS1 Mutations. Striking and Promising Missense Mutations on the GNAS1 Gene Exons 1, 4, 10, 4. J Ren Nutr. 2012;22(1):157-61. https://doi.org/fx4kv9.
12. Ozenli Y, Giray S, Sagliker Y, Adam SM. A Controlled Study of Psychiatric Manifestations and Electroencephalography Findings in Chronic Kidney Disease Patients With Sagliker Syndrome. J Ren Nutr. 2010;20(Suppl 5):S51-5. https://doi.org/b8pt3g.
13. Padilla-Ochoa GR, Chávez-Iñiguez JS, Magaña-Urzúa JA, Plata-Florenzano JE. Síndrome de Sagliker: presentación de dos casos y revisión de la literatura. Nefrol Latinoam. 2018;15(1). https://doi.org/kczb.
14. Crucelegui MS, Rosa-Diez G, Serra D, Ortiz MI, Diehl M. Síndrome de hueso hambriento asociado al hiperparatiroidismo secundario en la enfermedad renal crónica. Actual. Osteol. 2014;10(1)11-19.
Referencias
References
Sagliker Y, Acharya V, Ling Z, Golea O, Sabry A, Eyupoglu K, et al. International Study on Sagliker Syndrome and Uglifying Human Face Appearence in Severe and Late Secondary Hyperparathyroidism in Chronic Kidney Disease Patients. J Ren Nutr. 2008;18(1):114-7. https://doi.org/dffc2p.
Uzel A, Uzel I, Sagliker Y, Yildiz I, Halvaci I, Paylar N, et al. Cephalometric Evaluation of Patients With Sagliker Syndrome: Uglifying Human Face Appearance in Severe and Late Secondary Hyperparathyroidism in Chronic Renal Failure Patients. J Ren Nutr. 2006;16(3):229-32. https://doi.org/d9ffrq.
Fordham CC, Williams TF. Brown Tumor and Secondary Hyperparathyroidism. N Engl J Med. 1963;269(3):129-31. https://doi.org/bm8zks.
Hou YC, Lu CL, Lu KC. Mineral bone disorders in chronic kidney disease. Nephrology. 2018;23(4):88-94. https://doi.org/gftd3b.
Queiroz IV, Queiroz SP, Medeiros R, Ribeiro RB, Crusoé-Rebello IM, Leão JC. Brown tumor of secondary hyperparathyroidism: surgical approach and clinical outcome. Oral Maxillofac Surg. 2016;20(4):435-9. https://doi.org/kcx8.
Sagliker Y, Balal M, Sagliker-Ozkaynak P, Paydas S, Sagliker C, Sabit Sagliker H, et al. Sagliker syndrome: Uglifying human face appearance in late and severe secondary hyperparathyroidism in chronic renal failure. Semin Nephrol.2004;24(5):449-55. https://doi.org/fjhtb6.
Erkan AN, Sagliker Y, Yildiz I, Ozluoglu L. Audiological Findings in Chronic Kidney Disease Patients With Sagliker Syndrome. J Ren Nutr. 2010;20(5):S56-8. https://doi.org/bpgsxt.
Mohebi-Nejad A, Gatmiri SM, Abooturabi SM, Hemayati R, Mahdavi-Mazdeh M. Diagnosis and treatment of Sagliker syndrome: a case series from Iran. Iran J Kidney Dis. 2014;8(1):76-80.
Mejía-Pineda A, Aguilera ML, Meléndez HJ, Lemus JA, Peñalonzo MA. Sagliker syndrome in patients with secondary hyperparathyroidism and chronic renal failure: Case report. Int J Surg Case Rep. 2015;8C:127-30. https://doi.org/kcx3.
Demirhan O, Arslan A, Sagliker Y, Akbal E, Ergun S, Bayraktar R, et al. Gene mutations in chronic kidney disease patients with secondary hyperparathyroidism and sagliker syndrome. J Ren Nutr. 2015;25(2):176-86. https://doi.org/f627qp
Yildiz I, Sagliker Y, Demirhan O, Tunc E, Inandiklioglu N, Tasdemir D, et al. International Evaluation of Unrecognizably Uglifying Human Faces in Late and Severe Secondary Hyperparathyroidism in Chronic Kidney Disease. Sagliker Syndrome. A Unique Catastrophic Entity, Cytogenetic Studies for Chromosomal Abnormalities, Calcium-Sensing Receptor Gene and GNAS1 Mutations. Striking and Promising Missense Mutations on the GNAS1 Gene Exons 1, 4, 10, 4. J Ren Nutr. 2012;22(1):157-61. https://doi.org/fx4kv9.
Ozenli Y, Giray S, Sagliker Y, Adam SM. A Controlled Study of Psychiatric Manifestations and Electroencephalography Findings in Chronic Kidney Disease Patients With Sagliker Syndrome. J Ren Nutr. 2010;20(Suppl 5):S51-5. https://doi.org/b8pt3g.
Padilla-Ochoa GR, Chávez-Iñiguez JS, Magaña-Urzúa JA, Plata-Florenzano JE. Síndrome de Sagliker: presentación de dos casos y revisión de la literatura. Nefrol Latinoam. 2018;15(1). https://doi.org/kczb.
Crucelegui MS, Rosa-Diez G, Serra D, Ortiz MI, Diehl M. Síndrome de hueso hambriento asociado al hiperparatiroidismo secundario en la enfermedad renal crónica. Actual. Osteol. 2014;10(1)11-19.
Cómo citar
APA
ACM
ACS
ABNT
Chicago
Harvard
IEEE
MLA
Turabian
Vancouver
Descargar cita
CrossRef Cited-by
1. Mario Manuel Morantes Salazar, Jenny Carolina Salazar Florez, Nathalia Jacome-Pérez, William Darío Arenas Borda, Camilo Andrés Lara Rodríguez. (2026). Severe Manifestation of Hyperparathyroidism With Sagliker Syndrome: A Case Report. Cureus, https://doi.org/10.7759/cureus.101753.
Dimensions
PlumX
Visitas a la página del resumen del artículo
Descargas
Licencia
Derechos de autor 2023 Case reports

Esta obra está bajo una licencia internacional Creative Commons Atribución 4.0.
Los autores al someter sus manuscritos conservarán sus derechos de autor. La revista tiene el derecho del uso, reproducción, transmisión, distribución y publicación en cualquier forma o medio. Los autores no podrán permitir o autorizar el uso de la contribución sin el consentimiento escrito de la revista.
El Formulario de Divulgación Uniforme para posibles Conflictos de Interés y los oficios de cesión de derechos y de responsabilidad deben ser entregados junto con el original.
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as conservarán sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cual estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons 4.0 que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los autores/as podrán adoptar otros acuerdos de licencia no exclusiva de distribución de la versión de la obra publicada (p. ej.: depositarla en un archivo telemático institucional o publicarla en un volumen monográfico) siempre que se indique la publicación inicial en esta revista.
Se permite y recomienda a los autores/as difundir su obra a través de Internet (p. ej.: en archivos telemáticos institucionales o en su página web) antes y durante el proceso de envío, lo cual puede producir intercambios interesantes y aumentar las citas de la obra publicada. (Véase El efecto del acceso abierto).