Estenosis distal del conducto biliar común por coinfección de citomegalovirus y Cryptosporidium spp. en síndrome de inmunodeficiencia adquirida. Reporte de un caso
Distal common bile duct stricture due to cytomegalovirus and Cryptosporidium spp. coinfection in acquired immunodeficiency syndrome. Case report
DOI:
https://doi.org/10.15446/cr.v9n2.97067Palabras clave:
Síndrome de Inmunodeficiencia Adquirida, Infecciones Oportunistas Relacionadas con el SIDA, Infecciones por Citomegalovirus, Criptosporidiosis, Enfermedades de los Conductos Biliares, Colangiopancreatografia Retrógrada Endoscópica (es)Acquired Immunodeficiency Syndrome, AIDS-Related Opportunistic Infections, Cytomegalovirus Infections, Cryptosporidiosis, Bile Duct Diseases, Cholangiopancreatography, Endoscopic Retrograde (en)
Descargas
Resumen
Introducción. La colangiopatía por síndrome de inmunodeficiencia adquirida es infrecuente y presenta una alta morbilidad. La estenosis del conducto biliar común (colédoco) y la colangitis esclerosante secundaria son sus formas más comunes, generalmente causadas por infecciones oportunistas.
Presentación del caso. Hombre de 27 años diagnosticado con síndrome de inmunodeficiencia adquirida, sin terapia antirretroviral al momento de su ingreso, quien consultó a un hospital de tercer nivel de complejidad en la ciudad de Bogotá por dolor en hipocondrio derecho y diarrea crónica de tres semanas de evolución. Se realizó coprocultivo que fue positivo para ooquistes de Cryptosporidium spp. Las pruebas de fosfatasa alcalina y gamma-glutamil transferasa evidenciaron una elevación en los valores. Adicionalmente, se practicó una colangiografía por resonancia magnética que mostró dilatación de la vía biliar por estenosis distal del conducto biliar común. La colangiopancreatografía retrógrada endoscópica confirmó el hallazgo y descartó una colangitis esclerosante. Se realizó la inserción de un stent biliar (endoprótesis) y se solicitó biopsia de la ampolla de Vater que mostró estructuras citomegálicas con inclusiones intracelulares. El diagnóstico final fue colangitis por citomegalovirus y Cryptosporidium spp., por lo que se inició terapia antirretroviral y tratamiento antiviral (ganciclovir) con evolución satisfactoria.
Conclusiones. La colangiopatía es una de las causas de dolor abdominal en pacientes con síndrome de inmunodeficiencia adquirida. El citomegalovirus y el Cryptosporidium spp. son los agentes etiológicos más frecuentes. El manejo se basa en la resolución de la estenosis por vía endoscópica, la terapia antirretroviral y el tratamiento antimicrobiano dirigido.
Abstract
Introduction: Acquired immunodeficiency syndrome (AIDS) cholangiopathy is a rare disease with a high morbidity rate. Common bile duct stricture and secondary sclerosing cholangitis are its most common manifestations, usually caused by opportunistic infections.
Case presentation: A 27-year-old male patient diagnosed with AIDS, without antiretroviral therapy at the time of admission, consulted due to pain in the right hypochondrium and chronic diarrhea for three weeks. A stool culture was performed, showing a positive result for Cryptosporidium spp. oocysts. Due to the persistence of abdominal pain and elevation of alkaline phosphatase and GGT, a magnetic resonance cholangiopancreatography was performed, showing dilatation of the biliary tract due to distal stricture of the common bile duct. Endoscopic retrograde cholangiopancreatography confirmed the finding and ruled out biliary cholangitis. A biliary stent was placed endoscopically, and a biopsy of the papilla was requested, which showed cytomegalic structures with intracellular inclusions. A final diagnosis of cholangitis due to cytomegalovirus and Cryptosporidium spp. was made, and antiretroviral therapy and antiviral treatment (ganciclovir) was started with satisfactory results.
Conclusions: Cholangiopathy is one of the causes of abdominal pain in patients with acquired immunodeficiency syndrome. Cytomegalovirus and Cryptosporidium spp. are the most frequent etiological agents. Treatment is based on endoscopic management of the stricture, antimicrobial therapy, and targeted antiviral therapy.
https://doi.org/10.15446/cr.v9n2.97067
Distal common bile duct stricture due to cytomegalovirus and Cryptosporidium spp. coinfection in acquired immunodeficiency syndrome. Case report
Keywords: Acquired Immunodeficiency Syndrome; AIDS-Related Opportunistic Infections;
Cytomegalovirus Infections; Cryptosporidiosis; Bile Duct Diseases; Cholangiopancreatography, Endoscopic Retrograde.
Palabras clave: Síndrome de Inmunodeficiencia Adquirida; Infecciones Oportunistas
Relacionadas con el SIDA; Infecciones por Citomegalovirus; Criptosporidiosis; Enfermedades de los Conductos Biliares; Colangiopancreatografia Retrógrada Endoscópica.
Andrés Fernando Rodríguez-Gutiérrez
Sergio Andrés Vallejo-Ávila
Universidad Nacional de Colombia - Faculty of Medicine -
Department of Internal Medicine - Bogotá - Colombia
Hospital Universitario Nacional de Colombia
- Internal Medicine Service - Bogotá - Colombia
Sergio Andrés Remolina-Granados
Universidad Nacional de Colombia - Faculty of Medicine
- Department of Internal Medicine - Bogotá - Colombia
Hospital Universitario Nacional de Colombia
- Infectious Diseases Service - Bogotá - Colombia
Juan Manuel Viveros-Carreño
Universidad Nacional de Colombia - Faculty of Medicine
- Department of Diagnostic Imaging - Bogotá - Colombia
Diana Lucia Martínez-Baquero
Hospital Universitario Nacional de Colombia
- Internal Medicine Service - Bogotá - Colombia
Hospital Universitario Nacional de Colombia
- Pathology Service - Bogotá - Colombia
Corresponding author
Andrés Fernando Rodríguez-Gutiérrez.
Departamento de Medicina Interna, Facultad de Medicina, Universidad Nacional de Colombia. Bogotá. Colombia. E-mail: afrodriguezg@gmail.com
Received: 03/07/2021 Accepted: 30/08/2021
Resumen
Introducción. La colangiopatía por síndrome de inmunodeficiencia adquirida es infrecuente y presenta una alta morbilidad. La estenosis del conducto biliar común (colédoco) y la colangitis esclerosante secundaria son sus formas más comunes, generalmente causadas por infecciones oportunistas.
Presentación del caso. Hombre de 27 años diagnosticado con síndrome de inmunodeficiencia adquirida, sin terapia antirretroviral al momento de su ingreso, quien consultó a un hospital de tercer nivel de complejidad en la ciudad de Bogotá por dolor en hipocondrio derecho y diarrea crónica de tres semanas de evolución. Se realizó coprocultivo que fue positivo para ooquistes de Cryptosporidium spp. Las pruebas de fosfatasa alcalina y gamma-glutamil transferasa evidenciaron una elevación en los valores. Adicionalmente, se practicó una colangiografía por resonancia magnética que mostró dilatación de la vía biliar por estenosis distal del conducto biliar común. La colangiopancreatografía retrógrada endoscópica confirmó el hallazgo y descartó una colangitis esclerosante. Se realizó la inserción de un stent biliar (endoprótesis) y se solicitó biopsia de la ampolla de Vater que mostró estructuras citomegálicas con inclusiones intracelulares. El diagnóstico final fue colangitis por citomegalovirus y Cryptosporidium spp., por lo que se inició terapia antirretroviral y tratamiento antiviral (ganciclovir) con evolución satisfactoria.
Conclusión. La colangiopatía es una de las causas de dolor abdominal en pacientes con síndrome de inmunodeficiencia adquirida. El citomegalovirus y el Cryptosporidium spp. son los agentes etiológicos más frecuentes. El manejo se basa en la resolución de la estenosis por vía endoscópica, la terapia antirretroviral y el tratamiento antimicrobiano dirigido.
Abstract
Introduction: Acquired immunodeficiency syndrome (AIDS) cholangiopathy is a rare disease with a high morbidity rate. Common bile duct stricture and secondary sclerosing cholangitis are its most common manifestations, usually caused by opportunistic infections.
Case presentation: A 27-year-old male patient diagnosed with AIDS, without antiretroviral therapy at the time of admission, consulted due to pain in the right hypochondrium and chronic diarrhea for three weeks. A stool culture was performed, showing a positive result for Cryptosporidium spp. oocysts. Due to the persistence of abdominal pain and elevation of alkaline phosphatase and GGT, a magnetic resonance cholangiopancreatography was performed, showing dilatation of the biliary tract due to distal stricture of the common bile duct. Endoscopic retrograde cholangiopancreatography confirmed the finding and ruled out biliary cholangitis. A biliary stent was placed endoscopically, and a biopsy of the papilla was requested, which showed cytomegalic structures with intracellular inclusions. A final diagnosis of cholangitis due to cytomegalovirus and Cryptosporidium spp. was made, and antiretroviral therapy and antiviral treatment (ganciclovir) was started with satisfactory results.
Conclusions: Cholangiopathy is one of the causes of abdominal pain in patients with acquired immunodeficiency syndrome. Cytomegalovirus and Cryptosporidium spp. are the most frequent etiological agents. Treatment is based on endoscopic management of the stricture, antimicrobial therapy, and targeted antiviral therapy.
Introduction
Gallbladder and biliary tract involvement in patients with acquired immunodeficiency syndrome (AIDS) has been known since the beginning of the epidemic of this disease (1). Virtually all cases of cholangiopathy in patients with AIDS have an infectious etiology due to opportunistic microorganisms and are associated with low CD4+ T-lymphocyte counts (2,3). Cytomegalovirus (CMV) and Coccidia are the main etiological agents of cholangiopathy in AIDS patients (4-6).
Before the introduction of highly active antiretroviral therapy (HAART), cholangiopathy in AIDS patients had a survival of less than one year; however, HAART substantially improved survival time and is the primary treatment for this biliary syndrome (3). Other interventions include specific antimicrobial therapy (7,8) and bile duct decompression when common bile duct (CBD) stricture is present (3,9).
The following is the case of a patient with AIDS who presented with biliary dilatation due to distal stricture of the CBD caused by co-infection by CMV and Criptosporidium spp.
Case presentation
A 27-year-old Afro-Colombian man from a tropical region of Colombia consulted the emergency department of a tertiary care hospital in the city of Bogotá after experiencing moderate, non-radiating and intermittent abdominal pain in the right hypochondrium for 20 days, accompanied by vomiting and intolerance to food and medication. At the time of consultation, the patient presented symptoms of anorexia, asthenia, and adynamia. He also reported a fever of 39°C four days prior to admission and diarrhea (six stools per day) without blood or mucus, consistency 7 on the Bristol stool scale, for the last two months.
The patient had a history of HIV infection diagnosed six years earlier, with CD4+ lymphocyte count of 463 cells/µL and HIV viral load of 69 453 copies/mL at the time of diagnosis. In the first two years following his diagnosis, he received antiretroviral therapy with abacavir, lamivudine and zidovudine with proper virological response; however, due to health insurance problems, he lost his access to antiretroviral therapy. The patient reported having both insertive and receptive sex with men.
Two months prior to admission, he was diagnosed with cerebral toxoplasmosis that was treated with clindamycin, pyrimethamine and folinic acid (due to hypersensitivity to trimethoprim sulfamethoxazole). He was also diagnosed with hepatitis C, viral load of 110 112 copies/µL (in the process of genotyping to establish therapeutic strategy), and esophageal candidiasis under treatment with fluconazole. At the time of consultation, he was in the fourth week of treatment.
On admission physical examination, the following findings were recorded: heart rate of 140 bpm (tachycardia), respiratory rate of 15 rpm, and blood pressure of 100/60 mmHg. The patient was dehydrated, without fever and with dry mucous membranes. He reported abdominal pain on deep palpation of the right hypochondrium and flank, negative Murphy’s sign, and no signs of peritoneal irritation. On neurological examination, he was attentive, but showed symptoms of bradyphrenia and impaired speech rhythm and fluency. No motor deficit or alterations in sensitivity (normal reflexes) were found. During dermatologic examination, generalized hyperpigmentation was evident.
Laboratory tests requested on admission showed CD4+ lymphocyte count of 58 cells/µL (CD4+ percentage of 7%), CD4+/CD8+ ratio of 0.09, and HIV viral load of 1 896 000 copies/mL. A blood count revealed the following results: leukocytes 2370 cells/µL (leukopenia), neutrophils 1630 cells/µL, total lymphocytes 480 cells/µL, hemoglobin 11.5 g/dL, mean corpuscular volume 81 fL (normocytic anemia), and platelet count 97 000 cells/µL (thrombocytopenia). The creatinine test showed elevation due to acute kidney injury caused by hypovolemia (1.8 mg/dL), while potassium and sodium tests showed moderate hypokalemia (2.96 mmol/L) and hypovolemic hyponatremia (131 mmol/L). Considering these findings, an immunosuppressed patient with dehydration due to chronic diarrhea, acute kidney injury and pancytopenia was considered. The medical staff decided to initiate the etiological search for diarrhea, so a stool culture, consecutive stool tests with Kinyoun stain, and a colonoscopy were requested on the second day of admission. Treatment with Ringer’s lactate solution was indicated, and hypokalemia was corrected with intravenous substitution.
The stool culture showed results consistent with inflammatory diarrhea with 5 red blood cells/field and 10 leukocytes/field. With these results, it was decided to start bacterial coverage with ciprofloxacin (500 mg intravenous every 12 hours). Due to the prolonged use of clindamycin, in addition to the unavailability of tests for Clostridium difficile, empirical treatment with metronidazole (500 mg intravenous every 12 hours) was indicated. The stool examination was negative for common parasites, but the second sample with Kinyoun stain was positive for Cryptosporidium oocysts. In view of the acute renal injury, the use of nitazoxanide was not considered due to its low efficacy in immunosuppressed patients.
Under these conditions and taking into account that the patient was in week four of treatment for cerebral toxoplasmosis, it was decided to initiate antiretroviral therapy to treat cryptosporidiosis and to avoid interactions with future hepatitis C treatment. Dolutegravir (50 mg/day) and oral tenofovir/emtricitabine (200-300 mg/day) were chosen.
On the third day of hospitalization, a colonoscopy was performed, showing the ileocecal valve with edema, erythema, and erosions. The biopsy reported ulcerated mucosa with moderate inflammatory infiltrate of neutrophils with exocytosis, so ulcerative typhlitis was diagnosed.
On the fifth day of hospitalization, as a result of the treatment, the patient no longer had diarrhea and the renal injury resolved. However, abdominal pain in the right hypochondrium persisted, so on the eighth day of hospital stay, an abdominal ultrasound was requested, which showed slight dilatation of the intrahepatic bile duct, dilatation of the extrahepatic bile duct, and a 10 mm CBD all the way to the intrahepatic portion without intraluminal echogenic lesions (Figure 1).
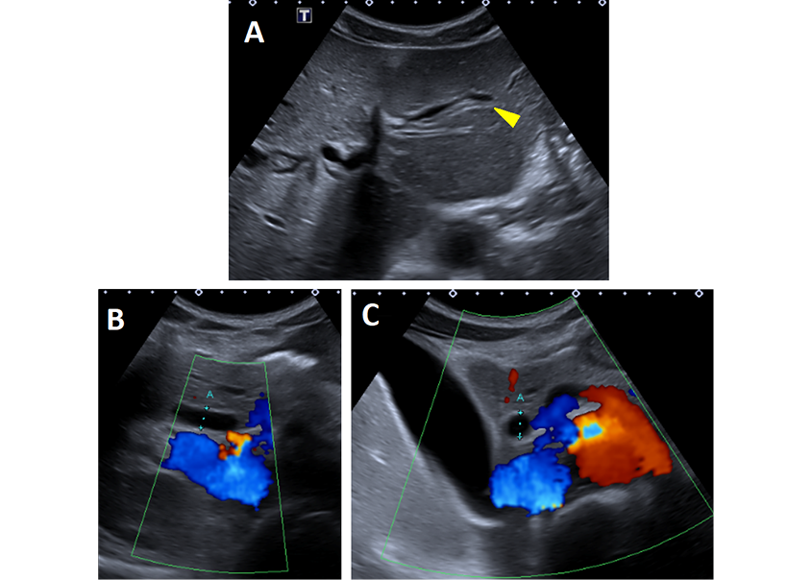
Figure 1. Abdominal ultrasound. (A) (B-mode) Axial plane of the liver showing dilatation of the intrahepatic biliary ducts (arrowhead, double barrel sign). Longitudinal (B) and transverse (C) color Doppler revealing dilatation of the CBD (blue dots) confirmed by the absence of flow on insonation.
Source: Images obtained while conducting the study.
On the other hand, based on the liver function tests performed on the second and eleventh days of hospitalization, a cholestatic pattern was observed, with elevated levels of alkaline phosphatase, gamma-glutamyl transferase (GGT) and transaminases, and normal levels of total bilirubin. The results of liver function tests one month prior to admission and on days 2 and 11 of hospitalization are presented in Table 1.
Table 1. Liver function tests of the patient.
|
Test |
1 month prior to admission |
Day 2 of hospitalization |
Day 11 of hospitalization |
|
Total bilirubin [0.10 - 1.20] |
0.56 mg/dL |
1.20 mg/dL |
0.83 mg/dL |
|
Direct bilirubin [0.10 - 0.25] |
0.28 mg/dL |
1.02 mg/dL |
0.30 mg/dL |
|
Indirect bilirubin [0.00 - 0.75] |
0.28 mg/dL |
0.18 mg/dL |
0.53 mg/dL |
|
Alkaline phosphatase [40 - 129] |
90 U/L |
240 U/L |
487 U/L |
|
Gamma-glutamyl transferase [10 - 72] |
-- |
-- |
2091 U/L |
|
AST test [5 - 40] |
45 U/L |
317 U/L |
141 U/L |
|
ALT blood test [5 - 40] |
153 U/L |
414 U/L |
183 U/L |
|
Amylase test [28 - 100] |
-- |
-- |
138 U/L |
AST: aspartate aminotransferase; ALT: alanine aminotransferase.Source: Own elaboration.
Taking into account these results, on the 13th day of hospitalization, a magnetic resonance cholangiography was requested, which showed a gallbladder in good condition, narrowing of the lumen in the distal portion of the CBD of 10 mm extension with involvement of the pancreaticobiliary junction, with dilation of the intrahepatic and extrahepatic bile duct, as well as the main pancreatic duct (duct of Wirsung). No filling defects suggesting calculi were found. As an anatomical variant, a right posterior duct with drainage to the common hepatic duct was found (Figure 2).
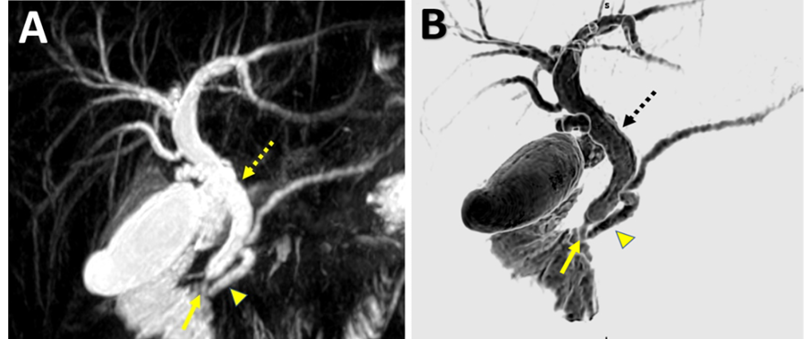
Figure 2. Magnetic resonance cholangiography: (A) Coronal maximum intensity projection and (B) 3D reconstruction, showing intrahepatic biliary dilatation and 10 mm CBD (dotted arrow). There is also evidence of a moderate 3.5 mm dilatation of the duct of Wirsung (arrowhead) caused by distal stricture of the CBD and the ampulla of Vater (arrow).
Source: Images obtained while conducting the study.
In view of these findings, on the 20th day of hospital stay, it was necessary to perform endoscopic retrograde cholangiopancreatography (ERCP), which revealed an area of irregular, friable mucosa with multiple membranes at the level of the pylorus and antrum, from which biopsies were taken (Figure 3).
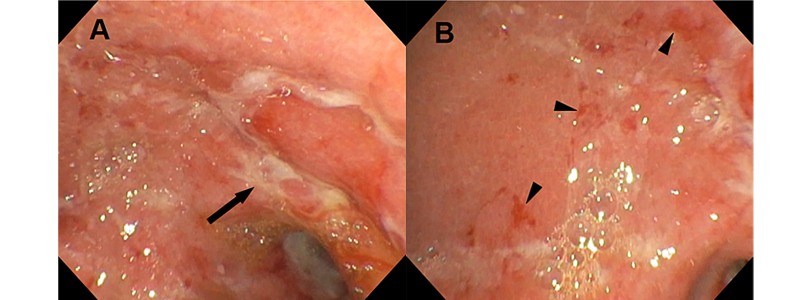
Figure 3. Upper gastrointestinal endoscopy at the level of the antro-pyloric region. A) friable mucosa, whitish membranes and pre-pyloric ulcers (arrow); B) some bleeding areas (arrowheads).
Source: Images obtained while conducting the study.
In the duodenum, the ampulla of Vater was found to be small and in its usual location. The bile duct was entered, and a cholangiography was performed, which confirmed dilatation of the CBD from its medial portion with a size of 10 mm (Figure 4). Papillotomy was performed and a 7 Fr by 10 cm stent was inserted; additionally, a biopsy of the ampulla of Vater was taken.
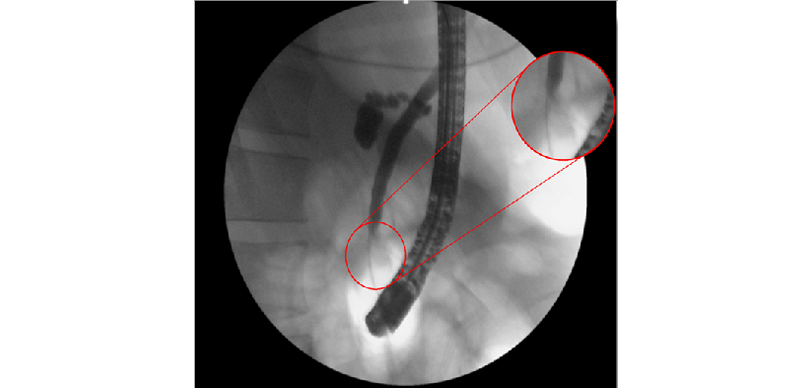
Figure 4. Endoscopic retrograde cholangiopancreatography. The cannulated bile duct is observed, as well as the image generated by the contrast medium that showed the narrowing during its course to the distal portion of the CBD where it became filamentous (enlarged image).
Source: Images obtained while conducting the study.
Given the low CD4+ lymphocyte count, resulting from ulcerative typhlitis, cholangiopathy and pancytopenia, CMV infection was suspected, so CMV testing was requested, reporting 10 616 copies/mL. Biopsies of the antrum and ampulla of Vater showed ulcerated and hemorrhagic mucosa with fibrin membranes. Eosinophilic intranuclear inclusions and cytoplasmic basophilic inclusions were observed in endothelial cells and fibroblasts (Figure 5), confirming the etiological diagnosis of CMV infection.
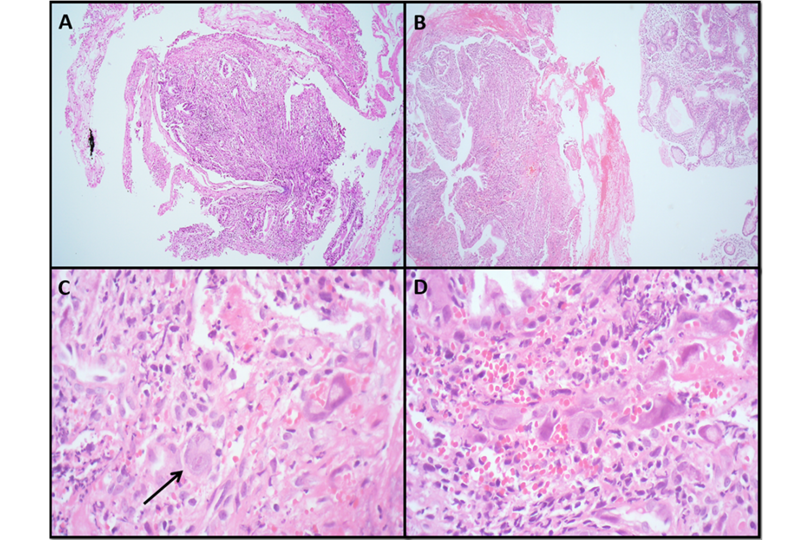
Figure 5. Microscopic biopsy images A) Antral gastric mucosa; B) H&E 4X, mucosa of the ampulla of Vater with foci of necrosis, hemorrhage and membranes containing fibrin and pus; C-D) H&E 40X, giant cell reaction (arrow in C) with eosinophilic intranuclear inclusions (viral) and cytoplasmic basophilic inclusions (D) suggestive of CMV infection.
Source: Images obtained while conducting the study.
Intravenous therapy with ganciclovir (5 mg/kg every 12 hours) was started with a switch to valganciclovir (900 mg every 12 hours orally) to complete 21 days of antiviral treatment and, subsequently, prophylaxis with valganciclovir 900 mg/day orally was started until the CD4+ lymphocyte count increased. The patient progressed satisfactorily, diarrhea and abdominal pain disappeared, and prophylaxis was maintained until the last follow-up. He was discharged on the 34th day of hospitalization.
Discussion
AIDS cholangiopathy is a rare condition. The first case described in the literature of AIDS cholangiopathy is attributed to Pitlik et al. (1), who described a patient with papillary stenosis and cholecystitis due to Cryptosporidium spp. in 1983. A study conducted in India in a cohort of 30 patients with this condition estimated an incidence of 0.9% (9), which has decreased with the advent of antiretroviral therapy (before its implementation, frequencies of up to 26% were reported) (10).
This report presents the case of a man diagnosed with AIDS with a low CD4+ lymphocyte count. This finding is consistent with other cases reported in the literature, since a low CD4+ lymphocyte count (less than 100 cells/µL) has been described as a distinctive condition (2,9); however, up to 10% of patients may have a count higher than 200 cells/µL (3).
80% of AIDS cholangiopathy cases are associated with infections by opportunistic microorganisms (3,9). The most frequently reported opportunistic infections include gastrointestinal cryptosporidiosis, Pneumocystis jirovecii infection, and CMV infection in multiple sites. Kaposi’s sarcoma is also often associated as an opportunistic neoplasm (3). In the present case, CMV and Cryptosporidium spp. coinfection, both opportunistic infections, was considered the main cause.
In this case, abdominal pain was the main symptom that led to the diagnosis of AIDS cholangiopathy. This symptom is common and occurs predominantly in the right upper quadrant (11) in 4 out of 5 patients (3,9). In a study conducted by Thuluvath et al. in a cohort of 63 AIDS patients with abdominal pain (35 of whom had right upper quadrant pain), 63% of the cases were related to AIDS cholangiopathy (12).
Another symptom that has been documented in AIDS cholangiopathy, regardless of the portion of the bile duct affected, is chronic diarrhea (2). Moreover, nausea and vomiting are usually observed (2) and in 25% of the cases fever is also present (9). These symptoms were found in the reported case.
According to a study conducted by Devarbhavi et al. in 30 people diagnosed with AIDS cholangiopathy, up to 20% of patients may be asymptomatic, and the diagnosis is usually made by an incidental finding (9). The most common finding on physical examination is hepatomegaly in 2 out of 3 patients with cholangiopathy (9), although this symptom was not present in this report.
Elevation of alkaline phosphatase (67% of cases), generally above 400 U/L, and GGT (in 80% of cases) (9) is the usual biochemical finding in AIDS cholangiopathy, as in the case presented. Jaundice and hyperbilirubinemia are rare, being found in only approximately 10% of patients (9). Transaminases are slightly elevated in 40% of patients, as in the case reported (9). It should be noted that 10% of the cases of patients with AIDS cholangiopathy develop pancreatitis; however, the cases described in the literature have been classified as mild, although the literature on the subject is scarce (9).
AIDS cholangiopathy can occur in multiple locations of the biliary tract and can have different manifestations that vary depending on the case. In some situations, distal stricture of the CBD at the level of the ampulla of Vater is described (9), in others papillary stricture in combination with sclerosing cholangitis is more frequently seen (3), while proximal stricture of the CBD has been observed in a small proportion (9). In a study by Ko et al. in 94 patients, the combination of papillary stricture and biliary cholangitis was present in 43% of cases, followed by papillary stricture with 36%, sclerosing cholangitis in 15%, and extrahepatic stricture in the remaining 5% (3). These findings are consistent with the results of another study by Daly & Padley (11) in a cohort of 50 patients.
In this case, biliary dilatation was observed in the abdominal ultrasound, magnetic resonance cholangiography and ERCP, so the syndromic diagnosis of AIDS cholangiopathy was based on the results of the imaging studies of the biliary tract. Ultrasonography, magnetic resonance cholangiography and ERCP are the best documented modalities in the study of AIDS cholangiopathy (11,13).
Compared to ERCP, ultrasound has a high detection rate of CBD dilatation, although it has an important limitation in the visualization of other signs of cholangiopathy such as the detection of thickening and irregularity of the wall of the extrahepatic bile duct. Despite this, ultrasound has a sensitivity of 97% and specificity of 100% (11).
Although magnetic resonance cholangiography has not been directly compared with ERCP in AIDS cholangiopathy, it is considered to have high detection power. In some cases, it appears to have better detection ability for intrahepatic biliary cholangitis than ERCP (13,14). However, ERCP is the gold standard for the detection of this type of disease, with the possibility of interventions (sphincterotomy).
In the case reported, co-infection by Cryptosporidium spp. and CMV was established. These two etiologic agents are frequently associated with AIDS cholangiopathy, both in isolation and in coinfection. However, other etiologic agents such as Cystoisospora belli and fungi of the Microsporidia class, among others, are usually involved, although in smaller numbers (Table 2).
Table 2. Diseases of the biliary tract in AIDS cholangiopathy.
|
Manifestation |
Associated etiologic agent |
Study |
|
Papillary stenosis |
Histoplasma capsulatum |
Kapelusznik et al. (15) |
|
Giardia lamblia |
Aronson et al. (16) |
|
|
Cryptosporidium spp. |
Pitlik et al. (1), Velásquez et al. (2), and Margulis et al. (17) |
|
|
CMV |
Tyagi et al. (6), Devarbhavi et al. (9), and Margulis et al. (17) |
|
|
Concomitant infection with CMV and Cryptosporidium spp. |
Margulis et al. (17), and Liong and Sukumar (18) |
|
|
Microsporidia |
Velásquez et al. (2) |
|
|
CBD stricture |
Unspecified etiology |
Devarbhavi et al. (9) |
|
Sclerosing cholangitis |
CMV |
Hidalgo-Tenorio et al. (5) |
|
Cryptosporidium spp. |
Velásquez et al. (2) |
|
|
Coinfection with CMV and Cryptosporidium spp. |
Liong and Sukumar (18) |
|
|
Cystoisospora belli |
Velásquez et al. (2), and Walther and Topazian (19) |
|
|
Microsporidia |
Velásquez et al. (2) |
|
|
Giardia lamblia |
Aronson et al. (16) |
|
|
Ductopenia |
CMV |
Tyagi et al. (6) |
|
Extrahepatic stricture |
Unspecified etiology |
Ko et al. (3) |
|
Acalculouscholecystitis |
Coinfection with CMV and Cryptosporidium spp. (15% of cases) |
French et al. (4) |
|
Microsporidia (8% of cases) |
French et al. (4) |
|
|
Cryptosporidium spp. (8% of cases) |
Pitlik et al. (1), French et al. (4), and Margulis et al. (17) |
|
|
CMV (6% of cases) |
French et al. (4) and Margulis et al. (17) |
|
|
Cystoisospora belli (1% of cases) |
French et al. (4) and Benator et al. (20) |
|
|
Pneumocystis jirovecii (1% of cases) |
French et al. (4) |
|
|
Kaposi’s sarcoma (1% of cases) |
French et al. (4) |
|
|
Histoplasma capsulatum |
Shinha and Zabarsky (21) |
|
|
Idiopathic (59% of cases) |
French et al. (4) |
|
|
Cholecystitis with cholelithiasis |
Coinfection with CMV and Cryptosporidium spp (7% of cases) |
French et al. (4) |
|
Cryptosporidium spp. (7% of cases) |
||
|
CMV (4% of cases) |
||
|
Microsporidia (4% of cases) |
||
|
Cholelithiasis (78% of cases) |
||
|
Biliary stricture after liver transplantation |
Unknown etiology |
Spaggiari et al. (22) |
Source: Own elaboration.
In the case presented, there was no involvement of the gallbladder; however, in cases where it does occur, it is usually isolated and mainly caused by acalculous cholecystitis due to opportunistic agents (4,22), although there are reported cases of concomitant involvement of the CBD and gallbladder (1,17). The microbiological diagnosis of AIDS cholangiopathy depends on the etiologic agent. In case of biliary involvement by Cryptosporidium spp., the detection of oocysts in the biliary fluid may be accompanied by the histological finding of the microorganism (17). Likewise, oocysts are usually found in fecal matter (2).
Cytopathic evidence of CMV was reported in only 8% of patients in a case series by Devarbhavi et al. (9); however, the etiology was unclear. In the case reported, the etiological diagnosis was achieved due to the oocysts found in the stool culture and the presence of CMV in the gastric mucosa. It should be noted that HIV-infected patients with a CD4+ cell count <100 cells/μL are at increased risk for CMV AIDS cholangiopathy (23). Furthermore, patients with CMV infection may not have invasive disease (24).
AIDS cholangiopathy is a prognostic factor for poor survival; the results of the study by Ko et al. (3) showed a median survival of 9 months from diagnosis in patients in the pre- and post-HAART period. However, when patients on HAART were differentially analyzed, they had a median survival of 53 months compared to 5-9 months in patients without HAART. Thus, HAART has been shown to substantially improve survival. Additionally, the median survival of patients with AIDS cholangiopathy in the presence of another opportunistic infection is much lower (Hazard Ratio= 0.08, 95% confidence interval between 0.02 and 0.35) (3). In another case study by Devarbhavi et al. (most patients on HAART), the median survival after the diagnosis of cholangiopathy was 34 months (9).
The treatment of AIDS cholangiopathy is based on antiretroviral therapy, endoscopic decompression of the biliary tract, and surgical resection of the gallbladder (when the gallbladder is involved). Antimicrobial treatment will depend on the etiologic agent. The increase in CD4+ lymphocyte count associated with the use of HAART correlates with improvement in abdominal pain (9). Decompression of the bile duct has been proposed through different techniques, including endoscopic sphincterotomy. Cello & Chan (25), in a case series of 25 patients, found that endoscopic sphincterotomy shows symptomatic improvement in pain management. In these patients, there was evidence of a decrease in this symptom (from moderate-severe to mild) even up to 11 months after the procedure (25). Likewise, there are reports that show a decrease in the dilatation of the CBD after this procedure (9). Biliary stent is another therapeutic option; however, decompression of the biliary tract has no effect on mortality (3).
Ganciclovir and foscarnet are the drugs of choice for the treatment of AIDS-related gastrointestinal CMV, with a recommended duration of three to six weeks, after which prophylaxis is recommended until an increase in CD4+ lymphocytes greater than 100 cells/µL is achieved for more than 6 months when antiretroviral therapy is taken (8). The patient in the case reported received antiretroviral therapy as background therapy. Antiparasitic drugs such as nitazoxanide were not considered useful for the management of Cryptosporidium spp. due to their low efficacy, but ganciclovir was chosen to treat CMV infection. Finally, endoscopic sphincterotomy was performed and it was decided to place a stent.
Conclusions
Abdominal pain in AIDS patients should be evaluated systematically. When it occurs in the right hypochondrium, the first diagnostic possibility is AIDS cholangiopathy. AIDS cholangiopathy presents mainly as a distal stricture of the CBD or secondary sclerosing cholangitis. Its etiology is mainly due to opportunistic infections, especially Cryptosporidium spp. and CMV. Treatment is based on HAART, which has been shown to improve survival, bile duct decompression, with an acceptable effect on abdominal pain, and microbiological treatment for the management of the etiologic agent.
Ethical considerations
Informed consent was obtained from the legal guardian relative of the patient due to his cognitive limitation during the development of the case report.
Conflict of interest
None stated by the authors.
Funding
None stated by the authors.
Acknowledgments
To the gastroenterology group of the Hospital Universitario Nacional de Colombia for providing the ERCP images.
References
1.Pitlik SD, Fainstein V, Rios A, Guarda L, Mansell PW, Hersh EM. Cryptosporidial cholecystitis. N Engl J Med. 1983;308(16):967. https://doi.org/c45j5s.
2.Velásquez JN, Marta E, di-Risio CA, Etchart C, Gancedo E, Chertcoff AV, et al. Molecular identification of protozoa causing AIDS-associated cholangiopathy in Buenos Aires, Argentina. Acta Gastroenterol Latinoam. 2012;42(4):301-8
3.Ko WF, Cello JP, Rogers SJ, Lecours A. Prognostic factors for the survival of patients with AIDS cholangiopathy. Am J Gastroenterol. 2003;98(10):2176-81. https://doi.org/b2vtsp.
4.French AL, Beaudet LM, Benator DA, Levy CS, Kass M, Orenstein JM. Cholecystectomy in patients with AIDS: clinicopathologic correlations in 107 cases. Clin Infect Dis. 1995;21(4):852-8. https://doi.org/cgmjxm.
5.Hidalgo-Tenorio C, Blasco-Morente G. Sclerosing cholangitis by cytomegalovirus in highly active antiretroviral therapy era. Rev Esp Enferm Dig. 2013;105(9):557-60. https://doi.org/kwqb.
6.Tyagi I, Puri AS, Sakhuja P, Majumdar K, Lunia M, Gondal R. Co-occurrence of cytomegalovirus-induced vanishing bile duct syndrome with papillary stenosis in HIV infection. Hepatol Res. 2013;43(3):311-4. https://doi.org/f4nfqj.
7.Gianella S, Letendre S. Cytomegalovirus and HIV: A Dangerous Pas de Deux. J Infect Dis. 2016;214(Suppl 2):S67-74. https://doi.org/f88h99.
8.Panel on Guidelines for the Prevention and Treatment of Opportunistic Infections in Adults and Adolescents with HIV. Guidelines for the Prevention and Treatment of Opportunistic Infections in Adults and Adolescents with HIV [Internet]. National Institutes of Health, Centers for Disease Control and Prevention, HIV Medicine Association, and Infectious Diseases Society of America. Updated 2023 [cited 2023 Sep 28]. Available at: https://bit.ly/3QwwG3B.
9.Devarbhavi H, Sebastian T, Seetharamu SM, Karanth D. HIV/AIDS cholangiopathy: clinical spectrum, cholangiographic features and outcome in 30 patients. J Gastroenterol Hepatol. 2010;25(10):1656-60. https://doi.org/c53vnc.
10.Vakil NB, Schwartz SM, Buggy BP, Brummitt CF, Kherellah M, Letzer DM, et al. Biliary cryptosporidiosis in HIV-infected people after the waterborne outbreak of cryptosporidiosis in Milwaukee. N Engl J Med. 1996;334(1): 19. https://doi.org/bjd2bk.
11.Daly CA, Padley SP. Sonographic prediction of a normal or abnormal ERCP in suspected AIDS related sclerosing cholangitis. Clin Radiol. 1996;51(9):618-21. https://doi.org/dwpsmn.
12.Thuluvath PJ, Connolly GM, Forbes A, Gazzard BG. Abdominal pain in HIV infection. Q J Med. 1991;78(287):275-85. https://doi.org/kwqf.
13.Bilgin M, Balci NC, Erdogan A, Momtahen AJ, Alkaade S, Rau WS. Hepatobiliary and pancreatic MRI and MRCP findings in patients with HIV infection. AJR Am J Roentgenol. 2008;191(1):228-32. https://doi.org/d6d8xc.
14.Tonolini M, Bianco R. HIV-related/AIDS cholangiopathy: pictorial review with emphasis on MRCP findings and differential diagnosis. Clin Imaging. 2013;37(2):219-26. https://doi.org/kwqg.
15.Kapelusznik L, Arumugam V, Caplivski D, Bottone EJ. Disseminated histoplasmosis presenting as AIDS cholangiopathy. Mycoses. 2011;54(3):262-264. https://doi.org/cxvt9k.
16.Aronson NE, Cheney C, Rholl V, Burris D, Hadro N. Biliary giardiasis in a patient with human immunodeficiency virus. J Clin Gastroenterol. 2001;33(2):167-70. https://doi.org/czj9xg.
17.Margulis SJ, Honig CL, Soave R, Govoni AF, Mouradian JA, Jacobson IM. Biliary tract obstruction in the acquired immunodeficiency syndrome. Ann Intern Med. 1986;105(2):207-10. https://doi.org/kwqj.
18.Liong SY, Sukumar SA. Case of the month: An African woman presenting with acalculous cholecystitis and sclerosing cholangiopathy. Br J Radiol. 2009;82(980):699-703. https://doi.org/dd5k2n.
19.Walther Z, Topazian MD. Isospora cholangiopathy: case study with histologic characterization and molecular confirmation. Hum Pathol. 2009;40(9):1342-6. https://doi.org/d5t5k6.
20.Benator DA, French AL, Beaudet LM, Levy CS, Orenstein JM. Isospora belli Infection Associated with Acalculous Cholecystitis in a Patient with AIDS. Ann Intern Med. 1994 Nov 1;121(9):663-4. https://doi.org/kwqn.
21.Shinha T, Zabarsky G. Acalculous Cholecystitis Due to Histoplasma capsulatum in a Patient With HIV Infection. ACG Case Rep J. 2015;2(4):245-6. https://doi.org/gcb67p.
22.Spaggiari M, Ballarin R, di Benedetto F, Montalti R, de Ruvo N, Cautero N, et al. Does HIV-related cholangiopathy exist in the setting of liver transplantation? AIDS. 2010;24(7):1072-5. https://doi.org/cnjzcn.
23.Steininger C. Clinical relevance of cytomegalovirus infection in patients with disorders of the immune system. Clin Microbiol Infect. 2007;13(10):953-63. https://doi.org/d79f28.
24.Jacobson MA. AIDS-related cytomegalovirus gastrointestinal disease [Internet]. UpToDate. Updated 2022 [cited 28 Sep 2023]. Available at: https://bit.ly/47pEmLD.
25.Cello JP, Chan MF. Long-term follow-up of endoscopic retrograde cholangiopancreatography sphincterotomy for patients with acquired immune deficiency syndrome papillary stenosis. Am J Med. 1995;99(6):600-3. https://doi.org/b865mw.
Referencias
References
Pitlik SD, Fainstein V, Rios A, Guarda L, Mansell PW, Hersh EM. Cryptosporidial cholecystitis. N Engl J Med. 1983;308(16):967. https://doi.org/c45j5s.
Velásquez JN, Marta E, di-Risio CA, Etchart C, Gancedo E, Chertcoff AV, et al. Molecular identification of protozoa causing AIDS-associated cholangiopathy in Buenos Aires, Argentina. Acta Gastroenterol Latinoam. 2012;42(4):301-8
Ko WF, Cello JP, Rogers SJ, Lecours A. Prognostic factors for the survival of patients with AIDS cholangiopathy. Am J Gastroenterol. 2003;98(10):2176-81. https://doi.org/b2vtsp.
French AL, Beaudet LM, Benator DA, Levy CS, Kass M, Orenstein JM. Cholecystectomy in patients with AIDS: clinicopathologic correlations in 107 cases. Clin Infect Dis. 1995;21(4):852-8. https://doi.org/cgmjxm.
Hidalgo-Tenorio C, Blasco-Morente G. Sclerosing cholangitis by cytomegalovirus in highly active antiretroviral therapy era. Rev Esp Enferm Dig. 2013;105(9):557-60. https://doi.org/kwqb.
Tyagi I, Puri AS, Sakhuja P, Majumdar K, Lunia M, Gondal R. Co-occurrence of cytomegalovirus-induced vanishing bile duct syndrome with papillary stenosis in HIV infection. Hepatol Res. 2013;43(3):311-4. https://doi.org/f4nfqj.
Gianella S, Letendre S. Cytomegalovirus and HIV: A Dangerous Pas de Deux. J Infect Dis. 2016;214(Suppl 2):S67-74. https://doi.org/f88h99.
Panel on Guidelines for the Prevention and Treatment of Opportunistic Infections in Adults and Adolescents with HIV. Guidelines for the Prevention and Treatment of Opportunistic Infections in Adults and Adolescents with HIV [Internet]. National Institutes of Health, Centers for Disease Control and Prevention, HIV Medicine Association, and Infectious Diseases Society of America. Updated 2023 [cited 2023 Sep 28]. Available at: https://bit.ly/3QwwG3B.
Devarbhavi H, Sebastian T, Seetharamu SM, Karanth D. HIV/AIDS cholangiopathy: clinical spectrum, cholangiographic features and outcome in 30 patients. J Gastroenterol Hepatol. 2010;25(10):1656-60. https://doi.org/c53vnc.
Vakil NB, Schwartz SM, Buggy BP, Brummitt CF, Kherellah M, Letzer DM, et al. Biliary cryptosporidiosis in HIV-infected people after the waterborne outbreak of cryptosporidiosis in Milwaukee. N Engl J Med. 1996;334(1): 19. https://doi.org/bjd2bk.
Daly CA, Padley SP. Sonographic prediction of a normal or abnormal ERCP in suspected AIDS related sclerosing cholangitis. Clin Radiol. 1996;51(9):618-21. https://doi.org/dwpsmn.
Thuluvath PJ, Connolly GM, Forbes A, Gazzard BG. Abdominal pain in HIV infection. Q J Med. 1991;78(287):275-85. https://doi.org/kwqf.
Bilgin M, Balci NC, Erdogan A, Momtahen AJ, Alkaade S, Rau WS. Hepatobiliary and pancreatic MRI and MRCP findings in patients with HIV infection. AJR Am J Roentgenol. 2008;191(1):228-32. https://doi.org/d6d8xc.
Tonolini M, Bianco R. HIV-related/AIDS cholangiopathy: pictorial review with emphasis on MRCP findings and differential diagnosis. Clin Imaging. 2013;37(2):219-26. https://doi.org/kwqg.
Kapelusznik L, Arumugam V, Caplivski D, Bottone EJ. Disseminated histoplasmosis presenting as AIDS cholangiopathy. Mycoses. 2011;54(3):262-264. https://doi.org/cxvt9k.
Aronson NE, Cheney C, Rholl V, Burris D, Hadro N. Biliary giardiasis in a patient with human immunodeficiency virus. J Clin Gastroenterol. 2001;33(2):167-70. https://doi.org/czj9xg.
Margulis SJ, Honig CL, Soave R, Govoni AF, Mouradian JA, Jacobson IM. Biliary tract obstruction in the acquired immunodeficiency syndrome. Ann Intern Med. 1986;105(2):207-10. https://doi.org/kwqj.
Liong SY, Sukumar SA. Case of the month: An African woman presenting with acalculous cholecystitis and sclerosing cholangiopathy. Br J Radiol. 2009;82(980):699-703. https://doi.org/dd5k2n.
Walther Z, Topazian MD. Isospora cholangiopathy: case study with histologic characterization and molecular confirmation. Hum Pathol. 2009;40(9):1342-6. https://doi.org/d5t5k6.
Benator DA, French AL, Beaudet LM, Levy CS, Orenstein JM. Isospora belli Infection Associated with Acalculous Cholecystitis in a Patient with AIDS. Ann Intern Med. 1994 Nov 1;121(9):663-4. https://doi.org/kwqn.
Shinha T, Zabarsky G. Acalculous Cholecystitis Due to Histoplasma capsulatum in a Patient With HIV Infection. ACG Case Rep J. 2015;2(4):245-6. https://doi.org/gcb67p.
Spaggiari M, Ballarin R, di Benedetto F, Montalti R, de Ruvo N, Cautero N, et al. Does HIV-related cholangiopathy exist in the setting of liver transplantation? AIDS. 2010;24(7):1072-5. https://doi.org/cnjzcn.
Steininger C. Clinical relevance of cytomegalovirus infection in patients with disorders of the immune system. Clin Microbiol Infect. 2007;13(10):953-63. https://doi.org/d79f28.
Jacobson MA. AIDS-related cytomegalovirus gastrointestinal disease [Internet]. UpToDate. Updated 2022 [cited 28 Sep 2023]. Available at: https://bit.ly/47pEmLD.
Cello JP, Chan MF. Long-term follow-up of endoscopic retrograde cholangiopancreatography sphincterotomy for patients with acquired immune deficiency syndrome papillary stenosis. Am J Med. 1995;99(6):600-3. https://doi.org/b865mw.
Cómo citar
APA
ACM
ACS
ABNT
Chicago
Harvard
IEEE
MLA
Turabian
Vancouver
Descargar cita
Licencia
Derechos de autor 2023 Case reports

Esta obra está bajo una licencia internacional Creative Commons Atribución 4.0.
Los autores al someter sus manuscritos conservarán sus derechos de autor. La revista tiene el derecho del uso, reproducción, transmisión, distribución y publicación en cualquier forma o medio. Los autores no podrán permitir o autorizar el uso de la contribución sin el consentimiento escrito de la revista.
El Formulario de Divulgación Uniforme para posibles Conflictos de Interés y los oficios de cesión de derechos y de responsabilidad deben ser entregados junto con el original.
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as conservarán sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cual estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons 4.0 que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los autores/as podrán adoptar otros acuerdos de licencia no exclusiva de distribución de la versión de la obra publicada (p. ej.: depositarla en un archivo telemático institucional o publicarla en un volumen monográfico) siempre que se indique la publicación inicial en esta revista.
Se permite y recomienda a los autores/as difundir su obra a través de Internet (p. ej.: en archivos telemáticos institucionales o en su página web) antes y durante el proceso de envío, lo cual puede producir intercambios interesantes y aumentar las citas de la obra publicada. (Véase El efecto del acceso abierto).