Drenaje aberrante del conducto hepático sectorial posterior derecho en el conducto cístico. Reporte de caso
Aberrant drainage of the right sectoral posterior hepatic duct into the cystic duct. Case report
DOI:
https://doi.org/10.15446/cr.v10n1.101619Palabras clave:
Colecistitis, Colecistectomía, Conducto Colédoco, Variación anatómica (es)Cholecystitis, Anatomic Variation, Common Bile Duct, Cholecystectomy (en)
Descargas
Resumen
Introducción. La anatomía de la vía biliar con frecuencia suele presentar variantes de relevancia quirúrgica. La variante A5 (en la que el conducto hepático sectorial posterior derecho drena al conducto cístico) se presenta con una frecuencia de 1%, lo que la hace una patología rara que representa un alto riesgo de lesión durante un procedimiento quirúrgico como la colecistectomía.
Presentación del caso. Mujer de 27 años que ingresó al servicio de urgencias de una institución de cuarto nivel de complejidad en la ciudad de Tunja (Colombia) por sintomatología consistente en dolor abdominal localizado en hipocondrio derecho. Durante su estancia hospitalaria fue diagnosticada con colecistitis aguda y coledocolitiasis, por lo que se realizó una colangiopancreatografía retrógrada endoscópica (CPRE) y, posteriormente, una colecistectomía laparoscópica, cuyos resultados documentaron una variante de la vía biliar anatómica tipo A5.
Conclusión. Es de gran importancia clínica que el cirujano tenga un adecuado conocimiento de la anatomía del árbol biliar, así como de sus variantes anatómicas, con el fin de disminuir al máximo la posibilidad de lesiones durante el desarrollo de una cirugía y, de esta forma, mejorar el pronóstico de estos pacientes.
Abstract
Introduction: The anatomy of the biliary tract often presents variants of surgical relevance. The A5 variant (in which the right posterior sectoral hepatic duct drains into the cystic duct) occurs with a frequency of 1%, making it a rare condition that poses a high risk of injury during a surgical procedure such as cholecystectomy.
Case presentation: A 27-year-old woman was admitted to the emergency room of a quaternary care institution located in the city of Tunja (Colombia) due to abdominal pain in the right hypochondrium. During her hospital stay, she was diagnosed with acute cholecystitis and choledocholithiasis. She underwent an endoscopic retrograde cholangiopancreatography (ERCP) and, subsequently, a laparoscopic cholecystectomy. The results of these procedures showed a type A5 anatomical variant of the biliary tract.
Conclusion: An adequate knowledge of the anatomy of the biliary tree, as well as its anatomical variants, is of great clinical relevance for surgeons in order to minimize the possibility of injury during surgery and, thus, improve the prognosis of these patients.
https://doi.org/10.15446/cr.v10n1.101619
Aberrant drainage of the right sectoral posterior hepatic duct into the cystic duct. Case report
Keywords: Cholecystitis; Cholecystectomy; Common Bile Duct; Anatomic Variation.
Palabras clave: Colecistitis; Colecistectomía; Conducto Colédoco; Variación Anatómica.
José Antonio Támara-Prieto
Hospital Universitario San Rafael de Tunja - Research Department - Tunja - Colombia
Daniel Gerardo Fernández-Ávila
Hospital Universitario San Ignacio - Rheumatology Unit - Pontificia Universidad Javeriana - Bogotá - Colombia
José Antonio Támara-López
Hospital Universitario San Rafael - General Surgery Service - Tunja - Colombia
Corresponding author
José Antonio Támara-Prieto. División de Investigaciones, Hospital Universitario San Rafael de Tunja. Tunja. Colombia. E-mail: josetamara3@gmail.com
Received: 14/03/2022 Accepted: 16/06/2022
Resumen
Introducción. La anatomía de la vía biliar con frecuencia suele presentar variantes de relevancia quirúrgica. La variante A5 (en la que el conducto hepático sectorial posterior derecho drena al conducto cístico) se presenta con una frecuencia de 1%, lo que la hace una patología rara que representa un alto riesgo de lesión durante un procedimiento quirúrgico como la colecistectomía.
Presentación del caso. Mujer de 27 años que ingresó al servicio de urgencias de una institución de cuarto nivel de complejidad en la ciudad de Tunja (Colombia) por sintomatología consistente en dolor abdominal localizado en hipocondrio derecho. Durante su estancia hospitalaria fue diagnosticada con colecistitis aguda y coledocolitiasis, por lo que se realizó una colangiopancreatografía retrógrada endoscópica (CPRE) y, posteriormente, una colecistectomía laparoscópica, cuyos resultados documentaron una variante de la vía biliar anatómica tipo A5.
Conclusión. Es de gran importancia clínica que el cirujano tenga un adecuado conocimiento de la anatomía del árbol biliar, así como de sus variantes anatómicas, con el fin de disminuir al máximo la posibilidad de lesiones durante el desarrollo de una cirugía y, de esta forma, mejorar el pronóstico de estos pacientes.
Abstract
Introduction: The anatomy of the biliary tract often presents variants of surgical relevance. The A5 variant (in which the right posterior sectoral hepatic duct drains into the cystic duct) occurs with a frequency of 1%, making it a rare condition that poses a high risk of injury during a surgical procedure such as cholecystectomy.
Case presentation: A 27-year-old woman was admitted to the emergency room of a quaternary care institution located in the city of Tunja (Colombia) due to abdominal pain in the right hypochondrium. During her hospital stay, she was diagnosed with acute cholecystitis and choledocholithiasis. She underwent an endoscopic retrograde cholangiopancreatography (ERCP) and, subsequently, a laparoscopic cholecystectomy. The results of these procedures showed a type A5 anatomical variant of the biliary tract.
Conclusion: An adequate knowledge of the anatomy of the biliary tree, as well as its anatomical variants, is of great clinical relevance for surgeons in order to minimize the possibility of injury during surgery and, thus, improve the prognosis of these patients.
Introduction
Anatomical variants of the biliary tract can occur both intrahepatically and extrahepatically. According to the literature, the frequency of these variants may range from 24% to 57% of the population (1). Based on the classification proposed by Huang, described in the study conducted by Swain et al. (2), there are 5 variant types: A1: right posterior sectoral duct draining into the right anterior sectoral duct (typical); A2: trifurcation where the right posterior sectoral duct, the right anterior sectoral duct, and the left hepatic duct converge to form the common hepatic duct; A3: right posterior sectoral duct draining into the left hepatic duct; A4: right posterior sectoral hepatic duct draining directly into the common hepatic duct, and A5: right posterior sectoral posterior hepatic duct draining into the cystic duct.
Bile duct injuries during cholecystectomy, either open or laparoscopic, usually occur because of the different anatomical variants described in the literature (3). Therefore, it is necessary to be aware of these variants and perform an adequate preoperative analysis with supporting imaging studies such as magnetic resonance cholangiopancreatography and intraoperative cholangiogram (4).
Case presentation
A 27-year-old woman, farmer, was admitted to the emergency room of a quaternary care institution in the city of Tunja (Colombia) after a 2-week history of symptoms consisting of colicky abdominal pain located in the right hypochondrium, with no vomiting, nausea, jaundice, acholia, or choluria. The patient did not report any relevant clinical history.
On physical examination, she was in good general condition with normal vital signs, hydrated, oriented and alert. During the abdominal examination, the patient’s abdomen was soft, bowel sounds were present, and she complained of pain on superficial and deep palpation in the right hypochondrium, with a negative Murphy’s sign. No signs of peritoneal irritation, masses or organ enlargement were found. Laboratory tests performed on admission are described in Table 1.
Table 1. Results of blood test performed on admission.
|
Test |
Results |
Normal values |
|
Blood count |
||
|
Leucocytes Neutrophils Lymphocytes Hemoglobin Hematocrits Platelets |
7.29 x 103u/L 5.38 x 103u/L1.34 x 103u/L15.4 g/dL 43.9% 329 x 103u/L |
4 - 10 2 – 7 0.8 – 4 11 – 16 37 – 54 150 – 450 |
|
Amylase |
316 U/L |
30 – 118 |
|
Alkaline phosphatase |
302.95 UI/L |
38 – 116 |
|
ALT |
997 U/L |
0 - 40 |
|
AST |
1198 U/L |
9 – 49 |
|
Indirect bilirubin |
0.6 mg/dL |
- |
|
Direct bilirubin |
1.26 mg/dL |
- |
|
Total bilirubin |
1.2 mg/dL |
- |
ALT: alanine aminotransferase; AST: aspartate aminotransferase.
Source: Own elaboration.
Significant findings included an abnormal liver profile with increased alkaline phosphatase and transaminases, as well as increased amylase, while the blood count was normal and there was no evidence of anemia. On the same day of admission, an abdominal ultrasound was performed, reporting multiple gallstones with dilatation of intrahepatic and extrahepatic bile ducts and choledocholithiasis (dilatation of up to 12mm and gallstone located in the distal third of the common bile duct).
As a result, it was decided to admit the patient to the hospital on the same day she visited the ER for medical management and follow-up by the general surgery department. Furthermore, she was evaluated by the gastroenterology service 24 hours after admission, which considered that an ERCP with papillectomy should be performed, together with the removal of the gallstone.
During the ERCP, performed two days after admission, the gallstone was extracted from the common bile duct and the following findings were observed: normal intrahepatic bile duct, moderately dilated extrahepatic duct with a common bile duct of up to 8mm with a filling defect of 5mm inside, and a slightly contracted gallbladder, without identifiable cystic duct. However, confluence in the right hepatic duct or proximal common hepatic duct was suspected.
Two days after the ERCP, a laparoscopic cholecystectomy was performed to dissect the gallbladder. During the procedure, we found a normal common bile duct and an anomalous drainage of the right posterior sectoral hepatic duct draining into the middle third of the cystic duct, which was 0.5cm long (Figure 1).
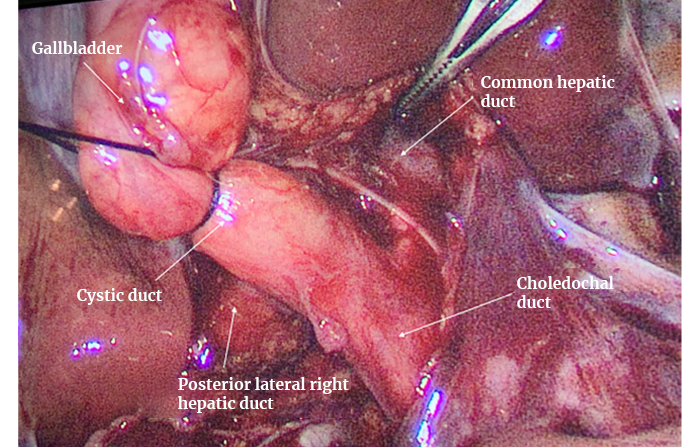
Figure 1. Right posterior hepatic duct draining into the cystic duct.
Source: Image obtained while conducting the study.
In view of these findings, an intraoperative cholangiogram was requested, which showed normal filling of the common bile duct and hepatic ducts and confirmed the diagnosis of anomalous drainage of the right posterior sectoral hepatic duct into the cystic duct (Figure 2). The posterior wall of the gallbladder (which was in contact with the liver) was dissected, the artery and the cystic duct were located and ligated by means of a Hem-o-lok® device, which was placed between the infundibulum of the gallbladder (where the cystic duct begins) and the cystic artery to prevent bleeding. Subsequently, a transcystic probe was placed to drain the contents with an adequate flow.

Figure 2. Intraoperative cholangiogram. Anomalous drainage of the right posterior hepatic duct into the cystic duct.
Source: Image obtained while conducting the study.
The patient progressed satisfactorily and had an adequate immediate postoperative recovery in the recovery room. She was taken to her room where she received food without any problems. Analgesic therapy was administered with diclofenac 75mg every 8 hours intravenously and acetaminophen 1g every 8 hours orally for 4 days, without complications. Four days after surgery, the patient was evaluated and discharged. Additionally, a follow-up appointment was scheduled 8 days later, during which the patient showed an excellent progress, so the general surgery department decided to definitively discharge her.
Discussion
The anatomy of the biliary tree is complex due to the anatomical variations at both the intrahepatic and extrahepatic levels. Although they are not of clinical interest in most cases, their importance for surgery is evident (5). Surgical interventions of the biliary tract are increasingly common, so there is an elevation in the frequency with which this type of anatomical variants and, therefore, of biliary tract injuries are found (6).
Variants of the extrahepatic right bile duct, as in this case, are a major risk factor for surgical injury during a laparoscopic procedure due to their low incidence and the high probability of injury to the biliary tract (7). Although the literature contains several classifications that accurately describe the variants of the bile duct, the classification proposed by Huang is probably the one that best depicts the reported case. This classification has 5 types: A1, A2, A3, A4 and A5, the latter being the rarest, showing an anomalous drainage of the right posterior sectoral duct into the cystic duct, as in the present case report (2).
According to Nari et al. (8), a study conducted by Jozami et al. describes a cohort of 338 cholangiographies, and their review establishes that the A5 variant is found in only 1.2% of the described cases. This variant has great surgical importance due to the high possibility of injuring the biliary tract during cholecystectomy (8,9).
The A5 variant described in Huang’s classification, the type F variant described in Blumgart’s classification (8), and the variant described in this case are all reporting the same findings. Multiple studies show that the frequency of this variant is between 2% and 5%, which reinforces the importance of having proper knowledge of the anatomy of the biliary tract and the use of prophylactic strategies for injuries that help the surgeon prevent possible complications (8).
Intraoperative cholangiogram during cholecystectomy is becoming increasingly common and routine in specialized centers, which has helped to reduce the incidence of biliary tract injuries due to its high effectiveness in the diagnosis of anatomical variants of the biliary tract, besides being a cost-effective method. This technique also allows the surgeon to make a more accurate incision in the biliary tract and thus operate with much more confidence, avoiding any injury to the biliary tree and reducing the associated complications as much as possible. This gives the patient the opportunity to have a quick recovery and reduces costs to the health system, reducing the time of hospital stays and possible re-operations, as was the case reported here (9,10).
Conclusions
More studies and reports related to the findings of aberrant anatomy of the biliary tract should be carried out in order to be able to identify more accurately all the possible injuries that may occur, expanding the existing literature and, in this way, know first-hand the incidence and the most frequent complications of these variations. Adequate planning of the surgical procedure should also be considered to prevent possible iatrogenic injuries to the biliary tract caused by an anatomical variant. Intraoperative cholangiogram is a simple, cost-effective and helpful method for the diagnosis and correct approach to these variants, which leads to a reduction of biliary tract injuries and more safety for the surgeon at the time of surgery.
Ethical considerations
The authors state that they have followed the protocols for the publication of patient data. The patient gave informed consent for the publication of this case report.
Conflicts of interest
None stated by the authors.
Funding
None stated by the authors.
References
1.Tolino MJ, Tartaglione AS, Sturletti CD, García MI. Variedades Anatómicas del Árbol Biliar. Implicancia Quirúrgica. Int J Morphol. 2010;28(4):1235-40. https://doi.org/c76j
2.Swain B, Sahoo RK, Sen KK, G MK, Parihar SS, Dubey R. Evaluation of intrahepatic and extrahepatic biliary tree anatomy and its variation by magnetic resonance cholangiopancreatography in Odisha population: a retrospective study. Anat and Cell Biol. 2020;53(1):8-14. https://doi.org/mtzd
3.Gómez-Portilla A, Romero E, Martín E, de Lecea CM, Cendoya I. Lesión iatrogénica del conducto sectorial anterior derecho hepático (segmentos V-VIII) aberrante e independiente. Dificultades en su diagnóstico y tratamiento. Cir Esp. 2008;84(2):109-11. https://doi.org/bgq7md
4.Mitidieri V, Ottone NE. La Vía Biliar Intrahepática. Clasificación Anátomo-Quirúrgica con Base Colangiográfica. Int J Morphol. 2015;33(4):1427-35. https://doi.org/mtzg
5.García MM, Barrón-González O, Hernández-Ramírez FJ, Ortiz-Amador M, Meléndez-Delgado MD. Conducto cístico con desembocadura en hepático derecho. Reporte de un caso. Rev Mex Cir Endoscop. 2018;19(1):17-20.
6.Cova-Bellot JE, Louis-Pérez C. Variantes anatómicas de las vías biliares: diagnóstico por CPRE y su relación con enfermedades biliares. GEN. 2016;70(1):16-22.
7.Limaylla-Vega H, Vega-Gonzales E. Lesiones iatrogénicas de las vías biliares. Rev Gastroenterol Peru. 2017; 37(4):350-6.
8.Nari GA, Viotto L, Gil F, Lamoratta F, Layún J, Arias A, et al. Lesión quirúrgica de la vía biliar de la variante anatómica de la confluencia tipo F. Importancia de la colangiografía intra-operatoria sistemática y las alternativas terapéuticas. Acta Gastroenterol Latinoam. 2015;45(4):303-6.
9.Wójcicki M, Patkowski W, Chmurowicz T, Bialek A, Wiechowska-Kozlowska A, Stankiewicz R, et al. Isolated right posterior bile duct injury following cholecystectomy: Report of two cases. World J Gastroenterol. 2013;19(36):6118-21. https://doi.org/f5brnv
10.Muñoz-Castro C, Inzunza M, Marino C, Martínez J. Cómo evitar la lesión de vía biliar en colecistectomía laparoscópica: Más allá de la visión crítica de seguridad. Rev Cir. 2021;73(3):362-9. https://doi.org/mtz8
Referencias
References
Tolino MJ, Tartaglione AS, Sturletti CD, García MI. Variedades Anatómicas del Árbol Biliar. Implicancia Quirúrgica. Int J Morphol. 22010;28(4):1235-40. https://doi.org/c76j
Swain B, Sahoo RK, Sen KK, G MK, Parihar SS, Dubey R. Evaluation of intrahepatic and extrahepatic biliary tree anatomy and its variation by magnetic resonance cholangiopancreatography in Odisha population: a retrospective study. Anat and Cell Biol. 2020;53(1):8-14. https://doi.org/mtzd
Gómez-Portilla A, Romero E, Martín E, de Lecea CM, Cendoya I. Lesión iatrogénica del conducto sectorial anterior derecho hepático (segmentos V-VIII) aberrante e independiente. Dificultades en su diagnóstico y tratamiento. Cir Esp. 2008;84(2):109-11. https://doi.org/bgq7md
Mitidieri V, Ottone NE. La Vía Biliar Intrahepática. Clasificación Anátomo-Quirúrgica con Base Colangiográfica. Int J Morphol. 2015;33(4):1427-35. https://doi.org/mtzg
García MM, Barrón-González O, Hernández-Ramírez FJ, Ortiz-Amador M, Meléndez-Delgado MD. Conducto cístico con desembocadura en hepático derecho. Reporte de un caso. Rev Mex Cir Endoscop. 2018;19(1):17-20.
Cova-Bellot JE, Louis-Pérez C. Variantes anatómicas de las vías biliares: diagnóstico por CPRE y su relación con enfermedades biliares. GEN. 2016;70(1):16-22.
Limaylla-Vega H, Vega-Gonzales E. Lesiones iatrogénicas de las vías biliares. Rev Gastroenterol Peru. 2017; 37(4):350-6.
Nari GA, Viotto L, Gil F, Lamoratta F, Layún J, Arias A, et al. Lesión quirúrgica de la vía biliar de la variante anatómica de la confluencia tipo F. Importancia de la colangiografía intra-operatoria sistemática y las alternativas terapéuticas. Acta Gastroenterol Latinoam. 2015;45(4):303-6.
Wójcicki M, Patkowski W, Chmurowicz T, Bialek A, Wiechowska-Kozlowska A, Stankiewicz R, et al. Isolated right posterior bile duct injury following cholecystectomy: Report of two cases. World J Gastroenterol. 2013;19(36):6118-21. https://doi.org/f5brnv
Muñoz-Castro C, Inzunza M, Marino C, Martínez J. Cómo evitar la lesión de vía biliar en colecistectomía laparoscópica: Más allá de la visión crítica de seguridad. Rev Cir. 2021;73(3):362-9. https://doi.org/mtz8
Cómo citar
APA
ACM
ACS
ABNT
Chicago
Harvard
IEEE
MLA
Turabian
Vancouver
Descargar cita
Licencia
Derechos de autor 2024 Case reports

Esta obra está bajo una licencia internacional Creative Commons Atribución 4.0.
Los autores al someter sus manuscritos conservarán sus derechos de autor. La revista tiene el derecho del uso, reproducción, transmisión, distribución y publicación en cualquier forma o medio. Los autores no podrán permitir o autorizar el uso de la contribución sin el consentimiento escrito de la revista.
El Formulario de Divulgación Uniforme para posibles Conflictos de Interés y los oficios de cesión de derechos y de responsabilidad deben ser entregados junto con el original.
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as conservarán sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cual estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons 4.0 que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los autores/as podrán adoptar otros acuerdos de licencia no exclusiva de distribución de la versión de la obra publicada (p. ej.: depositarla en un archivo telemático institucional o publicarla en un volumen monográfico) siempre que se indique la publicación inicial en esta revista.
Se permite y recomienda a los autores/as difundir su obra a través de Internet (p. ej.: en archivos telemáticos institucionales o en su página web) antes y durante el proceso de envío, lo cual puede producir intercambios interesantes y aumentar las citas de la obra publicada. (Véase El efecto del acceso abierto).


























