Epidemiological characteristics of tuberculosis in Colombia
Características epidemiológicas de la tuberculosis en Colombia
DOI:
https://doi.org/10.15446/revfacmed.v72n1.109537Palabras clave:
Tuberculosis, Public Health, Epidemiology, Colombia, Mycobacterium tuberculosis (en)Salud pública, Epidemiología, Colombia, Mycobacterium tuberculosis , Tuberculosis (es)
Descargas
Introduction: Tuberculosis (TB) is a serious global, regional, and national public health problem, as epidemiological data show it has a high burden of morbidity and mortality that has serious social, economic, and health impacts.
Objective: To describe the epidemiological characteristics of TB in Colombia.
Materials and methods: Descriptive study conducted using official data from the Colombian National Tuberculosis Control Program. TB cases reported in the country between 2019 and 2022 were characterized. Regarding treatment outcomes, given its duration, outcomes were analyzed from 2017 to 2021 and from 2017 to 2020 for susceptible TB and drug-resistant TB cases, respectively. TB incidence and mortality rates were calculated using historical data recorded in the National TB Control Program between 2002 and 2022.
Results: A stable trend was observed in the TB incidence rate between 2002 and 2015 (23-26.4 cases per 100 000 people); it slightly increased between 2016 to 2019 (25.0 to 27. 3 cases), but in 2020 and 2021, given the reduction in the detection of TB cases resulting from the COVID-19 pandemic, it decreased (22.0 and 25.9 cases). However, a significant increase was observed in 2022 (31.6 cases per 100 000 inhabitants), when the mortality rate was 2.4 cases per 100 000 inhabitants. The number of cases in children <15 years increased between 2019 and 2022 (2.71% vs. 3.30%). Finally, between 2017 and 2021, the frequency of successfully treated cases and relapses ranged from 60.97% to 75.0%.
Conclusion: The behavior of TB incidence and mortality in Colombia shows an increasing trend.
Introducción. La tuberculosis (TB) representa un grave problema de salud pública mundial, regional y nacional, toda vez que los datos epidemiológicos indican aún una alta carga de morbimortalidad con graves impactos sociales, económicos y en salud.
Objetivo. Describir las características epidemiológicas de la TB en Colombia.
Materiales y métodos. Estudio descriptivo realizado con los datos oficiales del Programa Nacional de Control de la Tuberculosis de Colombia. Se realizó una caracterización de los casos de TB reportados en el país entre 2019 y 2022. Respecto a los resultados del tratamiento, dada la duración del mismo, para TB sensible se analizaron de 2017 a 2021 y para TB farmacorresistente, de 2017 a 2020. Las tasas de incidencia y mortalidad por TB se calcularon usando los datos históricos registrados en el Programa Nacional de Control de la Tuberculosis entre 2002 y 2022.
Resultados. Entre 2002 y 2015 se observó una tendencia estable en la tasa de incidencia de TB (23-26.4 casos por cada 100 000 habitantes); entre 2016 y 2019 esta tasa sufrió un ligero aumento (25.0 a 27.3 casos), pero en 2020 y 2021, dada la reducción en la detección de casos producto de la pandemia por COVID-19, disminuyó (22.0 y 25.9 casos), aunque en 2022 se observó un aumento importante (31.6 casos por cada 100 000 habitantes), año en el que la tasa de mortalidad fue de 2.4 casos por cada 100 000 habitantes. La proporción de casos en menores de 15 años aumentó entre 2019 y 2022 (2.71% vs. 3.30%). Entre 2017 y 2021 el tratamiento exitoso de casos nuevos y recaídas osciló entre 60.97% y 75.0%.
Conclusiones. El comportamiento de la incidencia y la mortalidad por TB en Colombia muestra una tendencia al aumento.
Original research
Epidemiological characteristics of tuberculosis in Colombia
Características epidemiológicas de la tuberculosis en Colombia
Óscar Andrés Cruz-Martínez1,2 Julián Trujillo-Trujillo1,3
Julián Trujillo-Trujillo1,3
1 Ministerio de Salud y Protección Social de Colombia - Dirección de Promoción y Prevención - Programa Nacional de Control de la Tuberculosis - Bogotá D.C. - Colombia.
2 Universidad Nacional de Colombia - Bogotá Campus - Faculty of Nursing - Grupo de Investigación Salud y Cuidado de los Colectivos - Bogotá D.C. - Colombia.
3 Universidad Nacional Abierta y a Distancia - School of Health Sciences - Bogotá D.C. - Colombia.
Open access
Received: 17/06/2023
Accepted: 10/11/2023
Corresponding author: Óscar Andrés Cruz-Martínez. Universidad Nacional de Colombia. Bogotá D.C. Colombia. Email: oacruam@unal.edu.co.
Keywords: Tuberculosis; Public Health; Epidemiology; Colombia; Mycobacterium tuberculosis (MeSH).
Palabras clave: Tuberculosis; Salud pública; Epidemiología; Colombia; Mycobacterium tuberculosis (DeCS).
How to cite: Cruz-Martínez OA, Trujillo-Trujillo J. Epidemiological characteristics of tuberculosis in Colombia. Rev. Fac. Med. 2024;72(1):e109537. English. doi: https://doi.org/10.15446/revfacmed.v72n1.109537.
Cómo citar: Cruz-Martínez OA, Trujillo-Trujillo J. [Características epidemiológicas de la tuberculosis en Colombia]. Rev. Fac. Med. 2024;72(1):e109537. English. doi: https://doi.org/10.15446/revfacmed.v72n1.109537.
Copyright: Copyright: ©2024 Universidad Nacional de Colombia. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, as long as the original author and source are credited.
Abstract
Introduction: Tuberculosis (TB) is a serious global, regional, and national public health problem, as epidemiological data show it has a high burden of morbidity and mortality that has serious social, economic, and health impacts.
Objective: To describe the epidemiological characteristics of TB in Colombia.
Materials and methods: Descriptive study conducted using official data from the Colombian National Tuberculosis Control Program. TB cases reported in the country between 2019 and 2022 were characterized. Regarding treatment outcomes, given its duration, outcomes were analyzed from 2017 to 2021 and from 2017 to 2020 for susceptible TB and drug-resistant TB cases, respectively. TB incidence and mortality rates were calculated using historical data recorded in the National TB Control Program between 2002 and 2022.
Results: A stable trend was observed in the TB incidence rate between 2002 and 2015 (23-26.4 cases per 100 000 people); it slightly increased between 2016 to 2019 (25.0 to 27. 3 cases), but in 2020 and 2021, given the reduction in the detection of TB cases resulting from the COVID-19 pandemic, it decreased (22.0 and 25.9 cases). However, a significant increase was observed in 2022 (31.6 cases per 100 000 inhabitants), when the mortality rate was 2.4 cases per 100 000 inhabitants. The number of cases in children <15 years increased between 2019 and 2022 (2.71% vs. 3.30%). Finally, between 2017 and 2021, the frequency of successfully treated cases and relapses ranged from 60.97% to 75.0%.
Conclusion: The behavior of TB incidence and mortality in Colombia shows an increasing trend.
Resumen
Introducción. La tuberculosis (TB) representa un grave problema de salud pública mundial, regional y nacional, toda vez que los datos epidemiológicos indican aún una alta carga de morbimortalidad con graves impactos sociales, económicos y en salud.
Objetivo. Describir las características epidemiológicas de la TB en Colombia.
Materiales y métodos. Estudio descriptivo realizado con los datos oficiales del Programa Nacional de Control de la Tuberculosis de Colombia. Se realizó una caracterización de los casos de TB reportados en el país entre 2019 y 2022. Respecto a los resultados del tratamiento, dada la duración del mismo, para TB sensible se analizaron de 2017 a 2021 y para TB farmacorresistente, de 2017 a 2020. Las tasas de incidencia y mortalidad por TB se calcularon usando los datos históricos registrados en el Programa Nacional de Control de la Tuberculosis entre 2002 y 2022.
Resultados. Entre 2002 y 2015 se observó una tendencia estable en la tasa de incidencia de TB (23-26.4 casos por cada 100 000 habitantes); entre 2016 y 2019 esta tasa sufrió un ligero aumento (25.0 a 27.3 casos), pero en 2020 y 2021, dada la reducción en la detección de casos producto de la pandemia por COVID-19, disminuyó (22.0 y 25.9 casos), aunque en 2022 se observó un aumento importante (31.6 casos por cada 100 000 habitantes), año en el que la tasa de mortalidad fue de 2.4 casos por cada 100 000 habitantes. La proporción de casos en menores de 15 años aumentó entre 2019 y 2022 (2.71% vs. 3.30%). Entre 2017 y 2021 el tratamiento exitoso de casos nuevos y recaídas osciló entre 60.97% y 75.0%.
Conclusiones. El comportamiento de la incidencia y la mortalidad por TB en Colombia muestra una tendencia al aumento.
Introduction
Tuberculosis (TB) is an infectious disease that mainly involves the lungs and is caused by a bacterium named Mycobacterium tuberculosis, which is a facultative aerobic bacillus with a particle size of 1-10µ (microns) long by 0.2-0.6µ wide and a slow replication time of 15-18 hours.1,2 TB bacteria is spread through the air from one person to another via microaerosols. When someone with TB disease of the lungs or throat coughs, sneezes, speaks, or sings, tiny particles containing M. tuberculosis are expelled into the air and anyone nearby can breathe in these bacteria and become infected. This scenario may occur in any setting (family, work, community, or health care institutions).3-5
The World Health Organization (WHO) estimates that a quarter of the world’s population is infected with M. tuberculosis, but only 5-10% develop active TB at some point in their lives. In this regard, it has been reported that the risk of activation is higher at extreme ages or in the presence of diseases or conditions that generate immunosuppression.4,6
According to the WHO Global Tuberculosis Report 2023,7 in 2022, there were 10.6 million TB cases (95%CI: 9.8-11.4 million) and 1.30 million TB deaths (95%CI: 1.18-1.43 million) worldwide, of which 167 000 occurred in HIV-positive individuals. Furthermore, in that same year, WHO7 estimated that 410 000 people with TB (95%CI: 370 000-450 000) developed forms of TB resistant to isoniazid and rifampicin, which is known as multidrug-resistant tuberculosis (MDR/RR-TB).
In 2022, the total incidence rate of TB in Colombia, according to WHO, was 25 000 cases (95%CI: 19 000-30 000),7 and 17 460 cases were reported according to official data from the National Tuberculosis Control Program, with a reported incidence and mortality rate of 31.6 and 2.4 cases per 100 000 inhabitants, respectively.8
The COVID-19 pandemic led to a significant setback in meeting the goals established in the Colombian Ministry of Health and Social Protection’s National Strategic Plan “Toward the End of Tuberculosis. Colombia 2016-2025”,9 which adopted the WHO’s End of TB strategy,10 resulting in an unusual reduction of cases in 2020 and 2021, when detection rates were 66% and 67%, respectively. These figures were far from the goal of more than 90% of detected cases that was set out in the national strategic plan.9
In 2020, the Ministry of Health and Social Protection issued Resolution 227,11 which is a milestone for the control of TB in the country since it updated the technical and operational guidelines for the prevention and management of this disease nationwide. This regulation adopted the recommended therapeutic regimens for active and latent TB infection and stipulated that the Benefit Plan Administrators and public and private health service providers must guarantee access to diagnostic technologies such as molecular tests, liquid cultures, and chest X-rays. The resolution also included new oral treatment regimens for sensitive TB, resistant TB, and latent infection, and outlined the responsibilities of health system actors, new treatment supervision modalities, comprehensive and interdisciplinary care, and the community approach with differential interventions in vulnerable groups.11
With this in mind, the objective of this article was to describe the epidemiological characteristics of TB in Colombia.
Materials and methods
Study type
Descriptive study.
Data collection
The data were collected from the National Tuberculosis Control Program8 and were anonymized to safeguard the confidentiality and security of the information. Data were collected on TB incidence and mortality, as well as data related to the characterization of the TB cases notified, namely, age, sex, geographic area of notification, insurance regime in the Colombian health system, TB type (sensitive or multidrug-resistant), and treatment outcome at discharge.
Incidence and mortality rates were calculated using historical data recorded in the National Tuberculosis Control Program between 2002 and 2022 reported to WHO.8 Information regarding characterization was obtained from the national nominal database of TB cases notified between 2019 and 2022, after they were cleaned, standardized, and validated. Regarding treatment outcomes, given the duration of treatment, data recorded between 2017 and 2021 for sensitive TB and between 2017 and 2020 for multidrug-resistant TB were analyzed.
Procedures
Cases were characterized by age group (≤14 years, 15-19 years, 20-34 years, 35-54 years, 55-64 years, or ≥65 years), sex (male or female), TB type (pulmonary or extrapulmonary), type of affected population, presence of comorbidities, geographic area of notification, health system enrollment (subsidized, contributory, special, or exceptional) and type of drug resistance (rifampicin-resistant and multidrug-resistant TB [RR/MDR-TB], isoniazid-resistant mono-resistant TB, and extensively drug-resistant TB [XDR]: RR/MDR TB with additional resistance to quinolone plus linezolid or bedaquiline; the latter category was applicable for the years 2020 to 2022). The indicator for successful treatment was also analyzed, which is the sum of cured cases and completed treatments according to WHO definitions.12
Statistical analysis
Data are described using absolute and relative frequencies. Incidence and mortality rates between 2002 and 2022 were calculated using the information available in the 2018 National Population and Housing Census Population Projections of the National Administrative Department of Statistics13 and the historical series of data reported in the National Tuberculosis Control Program as the denominator.8
Programmatic data analysis, including plots and tables, was performed using the National Tuberculosis Control Program nominal databases available for the years 2019 to 2022,8 in Microsoft Excel. It is worth noting that there were no nominal databases available for years prior to 2019.
Ethical considerations
Secondary and officially available data were used in the present study, so approval by an institutional ethics committee was not required. To safeguard the identity of the individuals affected by TB, data were anonymized and presented in a consolidated form.
Results
Between 2002 and 2015, there was a stable trend in terms of the reported incidence rate (23-26.4 cases per 100 000 population) and a reduction in the estimated incidence rate (new cases and relapses): 40 cases in 2002 vs. 31 in 2015. Between 2016 and 2019, the reported incidence rate underwent a slight increase from 25.0 to 27.3 cases per 100 000 inhabitants; however, in 2020 and 2021, an unusual decrease in case detection was observed, leading to a reduction in the incidence rate (22.0 and 25.9 cases per 100 000 inhabitants, respectively). Finally, in 2022, the trend reverted and a significant increase in cases was observed, reaching a reported incidence rate of 31.6 cases per 100 000 population (Figure 1).
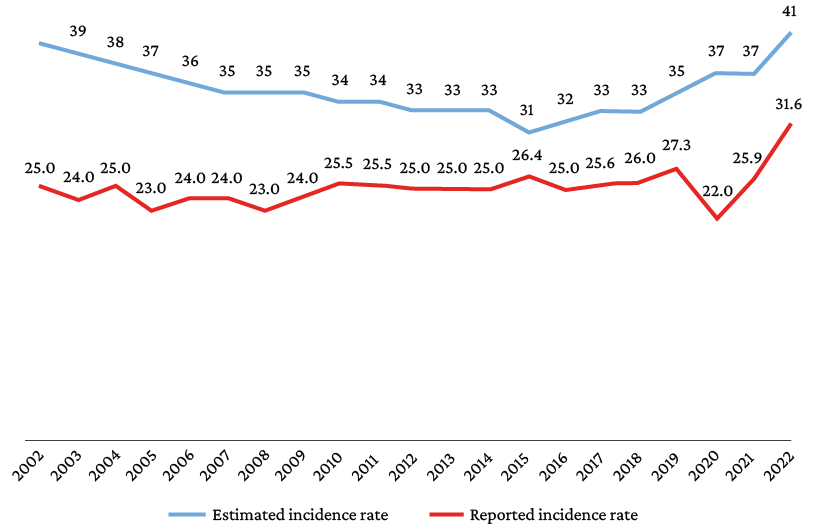
Figure 1. Incidence rates of tuberculosis per 100 000 inhabitants in Colombia. 2002-2022.
Regarding the mortality indicator, between 2002 and 2011, rates ranging from 2.50 to 1.85 per 100 000 inhabitants were reported, and from 2011 to 2019, a slight and stable increase in the mortality rate was observed, going from 1.85 to 2.24 per 100 000 inhabitants. In 2020, although there was a decrease (1.93 cases per 100 000 population), in 2021 and 2022 there was an upward trend (2.1 and 2.4 cases per 100 000 population, respectively) (Figure 2).
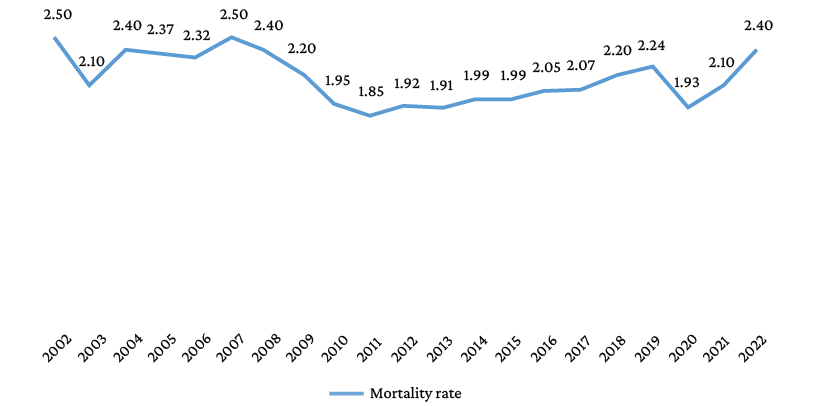
Figure 2. Tuberculosis mortality rates per 100 000 inhabitants in Colombia. 2002-2022.
In 2022, 17 460 TB cases were reported in Colombia, of which 14 824 (84.90%) were pulmonary and 2 636 (15.10%) extrapulmonary; in addition, 65.14% of people affected by TB were men, equivalent to a male-to-female ratio of 2:1. The annual distribution of TB cases by sex, age, population type, and presence of comorbidities from 2019 to 2022 is shown in Table 1.
Table 1. Tuberculosis cases reported in the Colombian National Tuberculosis Control Program. 2019-2022.
|
Variable |
Year 2019 |
Year 2020 |
Year 2021 |
Year 2022 |
|||||
|
n |
% |
n |
% |
n |
% |
n |
% |
||
|
Sex |
Male |
9 659 |
64.89 |
8 277 |
65.78 |
9 399 |
66.70 |
11 374 |
65.14 |
|
Female |
5 229 |
35.13 |
4 305 |
34.22 |
4 692 |
33.30 |
6 086 |
34.86 |
|
|
Age (years) |
≥65 |
3 226 |
21.67 |
2 471 |
19.64 |
2 783 |
19.75 |
3 689 |
21.13 |
|
55-64 |
1 916 |
12.87 |
1 566 |
12.45 |
1 891 |
13.42 |
2 516 |
14.41 |
|
|
35-54 |
3 884 |
26.09 |
3 423 |
27.21 |
3 728 |
26.46 |
4 548 |
26.05 |
|
|
20-34 |
4 769 |
32.04 |
4 208 |
33.44 |
4 707 |
33.40 |
5 384 |
30.84 |
|
|
15-19 |
687 |
4.62 |
586 |
4.66 |
602 |
4.27 |
746 |
4.27 |
|
|
≤14 |
404 |
2.71 |
328 |
2.61 |
380 |
2.70 |
577 |
3.30 |
|
|
Specific populations |
Deprived of liberty |
997 |
6.70 |
833 |
6.62 |
1 412 |
10.02 |
1 241 |
7.11 |
|
Indigenous |
770 |
5.17 |
624 |
4.96 |
631 |
4.48 |
773 |
4.43 |
|
|
Afro-descendants |
793 |
5.33 |
478 |
3.80 |
507 |
3.60 |
630 |
3.61 |
|
|
Homeless |
537 |
3.61 |
500 |
3.97 |
438 |
3.11 |
567 |
3.25 |
|
|
Migrants |
666 |
4.47 |
740 |
5.88 |
879 |
6.24 |
935 |
5.36 |
|
|
LGBTIQ+ |
ND |
ND |
ND |
ND |
20 |
0.14 |
32 |
0.18 |
|
|
Health workers |
318 |
2.14 |
263 |
2.09 |
224 |
1.59 |
289 |
1.66 |
|
|
Disabled |
124 |
0.83 |
120 |
0.95 |
111 |
0.79 |
126 |
0.72 |
|
|
Gypsies |
34 |
0.23 |
7 |
0.06 |
10 |
0.07 |
32 |
0.18 |
|
|
Pregnant |
35 |
0.24 |
21 |
0.17 |
37 |
0.26 |
42 |
0.24 |
|
|
Psychiatric centers |
36 |
0.24 |
2 |
0.02 |
4 |
0.03 |
37 |
0.21 |
|
|
Comorbidities |
TB-malnutrition |
2 067 |
13.89 |
1 668 |
13.26 |
2 039 |
14.47 |
2 815 |
16.12 |
|
TB-HIV/AIDS |
1 724 |
11.58 |
1 644 |
13.07 |
1 654 |
11.74 |
2 057 |
11.78 |
|
|
TB-diabetes |
1 353 |
9.09 |
934 |
7.42 |
1 323 |
9.39 |
1 623 |
9.30 |
|
|
TB-COPD |
987 |
6.63 |
749 |
5.95 |
711 |
5.05 |
1 328 |
7.61 |
|
|
TB-kidney disease |
458 |
3.08 |
324 |
2.58 |
522 |
3.70 |
560 |
3.21 |
|
|
TB-cancer |
348 |
2.34 |
334 |
2.65 |
338 |
2.40 |
524 |
3.00 |
|
|
TB-use of psychoactives |
ND |
ND |
540 |
4.29 |
565 |
4.01 |
521 |
2.98 |
|
|
TB-COVID-19 |
ND |
ND |
1 060 |
8.42 |
294 |
2.09 |
70 |
0.40 |
|
|
TB-liver disease |
115 |
0.77 |
81 |
0.64 |
108 |
0.77 |
129 |
0.74 |
|
|
TB-silicosis |
50 |
0.34 |
56 |
0.45 |
46 |
0.33 |
73 |
0.42 |
|
|
Total |
14 886 |
100 |
12 582 |
100 |
14 091 |
100 |
17 460 |
100 |
|
LGBTIQ+: lesbian, gay, bisexual, transgender, transsexual, transvestite, intersex, queer; TB: tuberculosis; HIV: human immunodeficiency virus; AIDS: acquired immunodeficiency syndrome; COPD: chronic obstructive pulmonary disease; ND: no data.
Geographic distribution
Of the 17 460 TB cases reported in Colombia in 2022, 75.00% (n=13 095) were registered in 11 departments, and 753 (67.77%) of the country’s 1 111 municipalities and districts (including the capital district of Bogotá) reported 1 or more cases; in addition, 15 975 cases (91.49%) were reported in urban areas. In the same year, 52.28% (n=9 142) of the country’s TB cases were reported in the following 13 cities: Medellín (n=2 182, 12.49%), Santiago de Cali (n=1 466, 8.39%), Bogotá D.C. (n=1 326, 7.59%), Barranquilla (n=785, 4.49%), Cúcuta (n=489, 2.80%), Villavicencio (n=488, 2.79%), Cartagena (n=419, 2.39%), Bucaramanga (n=401, 2.29%), Bello (n=352, 2.01%), Pereira (n=349, 1.99%), Ibagué (n=345, 1.97%), Soledad (n=296, 1.69%), and Valledupar (n=244, 1.39%).
Distribution by type of health insurance plan in the Colombian health system
In 2022, 54.79% of the 17 460 people with TB were under the subsidized regime, with an incidence rate of 30 cases per 100 000 beneficiaries, while 33.21% belonged to the contributory regime, with a rate of 17 cases per 100 000 members. On the other hand, 5.50% of the people with TB were not insured and 6.50% belonged to the special health insurance and exception regimes.
Drug-resistant TB cases
Regarding drug-resistant TB cases, it was noted that there were fewer cases in 2020 and 2021 (years in which strict social isolation and mobility restriction measures were implemented and maintained due to the COVID-19 pandemic) (321 and 350, respectively) compared to 2017, 2018, 2019, and 2022 (408-469). Moreover, with respect to the type of drug-resistant TB, MDR/RR-TB was the most frequent in the study period (2017-2022) with 60.82% of the cases, except for 2017 when H mono/poly DR-TB was the most frequent (48.87%). Table 2 presents the annual distribution of drug-resistant TB cases in Colombia by type of resistance for the period 2017-2022.
Table 2. Cases of drug-resistant tuberculosis in Colombia. 2017-2022.
|
Year |
MDR/RR-TBa |
H mono/poly |
Non-H mono/poly |
XDR TB and pre-XDR-TBc |
Clinical diagnosis |
Total |
||||||
|
n |
% |
n |
% |
n |
% |
n |
% |
n |
% |
n |
% |
|
|
2017 |
212 |
47.75 |
217 |
48.87 |
0 |
0 |
7 |
1.58 |
8 |
1.80 |
444 |
100 |
|
2018 |
211 |
49.30 |
209 |
48.83 |
0 |
0 |
7 |
1.64 |
1 |
0.23 |
428 |
100 |
|
2019 |
209 |
51.23 |
168 |
41.18 |
2 |
0.49 |
5 |
1.23 |
24 |
5.88 |
408 |
100 |
|
2020 |
172 |
53.58 |
125 |
38.94 |
2 |
0.62 |
4 |
1.25 |
18 |
5.61 |
321 |
100 |
|
2021 |
203 |
58.00 |
129 |
36.86 |
1 |
0.29 |
11 |
3.14 |
6 |
1.71 |
350 |
100 |
|
2022 |
246 |
52.45 |
208 |
44.35 |
2 |
0.43 |
5 |
1.07 |
8 |
1.71 |
469 |
100 |
|
Total |
1 253 |
60.82 |
1056 |
51.26 |
7 |
0.33 |
39 |
1.89 |
65 |
3.15 |
2 060 |
100 |
MDR/RR-TB: multidrug-resistant or rifampicin-resistant tuberculosis; H: tuberculosis resistant only to isoniazid or poly-resistant to isoniazid (resistance to isoniazid and to a first-line drug other than rifampicin); XDR TB: extensively drug-resistant tuberculosis (resistance to isoniazid and rifampicin plus additional resistance to a quinolone and to bedaquiline and/or linezolid); Pre-XDR-TB: tuberculosis resistant to isoniazid and rifampicin plus a quinolone (levofloxacin or moxifloxacin).
Furthermore, of the 246 cases of MDR/RR-TB reported in 2022, 76.01% were reported in the following departments or cities: Antioquia (n=49, 19.92%), Santiago de Cali (n=30, 12.19%), Risaralda (n=21, 8.54%), Bogotá D.C. (n=19, 7.72%), Santander (n=17, 6.91%), Barranquilla (n=15, 6.10%), Tolima (n=10, 4.06%), Norte de Santander (n=9, 3.66%), Meta (n=9, 3.66%), and Buenaventura (n=8, 3.25%).
TB treatment outcomes
Between 2017 and 2021, the percentage of new and relapsed cases that were successfully treated ranged from 60.96% to 75.00%. The treatment outcomes of TB cases for this period are presented in Table 3.
Table 3. Tuberculosis treatment outcomes in Colombia. 2017-2021.
|
Year |
Total new cases and relapses |
Successful treatment |
Loss of treatment follow-up |
Failure |
Deaths |
Not evaluated |
|||||
|
n |
n |
% |
n |
% |
n |
% |
n |
% |
n |
% |
|
|
2017 |
13 212 |
8 055 |
60.96 |
1 150 |
8.70 |
66 |
0.49 |
1 653 |
12.51 |
2 288 |
17.31 |
|
2018 |
13 024 |
9 653 |
74.11 |
1 198 |
9.19 |
143 |
1.09 |
1 601 |
12.29 |
429 |
3.29 |
|
2019 |
13 480 |
10 110 |
75.00 |
1 213 |
8.99 |
134 |
0.99 |
1 685 |
12.50 |
338 |
2.50 |
|
2020 |
11 066 |
7 856 |
70.99 |
1 106 |
9.99 |
99 |
0.89 |
1 803 |
16.29 |
202 |
1.83 |
|
2021 |
12 667 |
9 373 |
73.99 |
1 114 |
8.79 |
139 |
1.09 |
1 757 |
13.87 |
284 |
2.24 |
|
Total |
63 449 |
45 047 |
70.99 |
5781 |
9.11 |
581 |
0.91 |
8 499 |
13.39 |
3 541 |
5.58 |
Finally, of the 1 654 TB and HIV coinfection cases reported in 2021, 55.02% were successfully treated (i.e., cured of infection after completing antifungal treatment), 28.78% died, 13.00% did not continue with follow-up or abandoned medication for more than 30 days, 2.00% were not evaluated, and 1.21% failed treatment. Regarding the treatment outcome of MDR/RR-TB, the success rate in 2017 was 44.02% and increased to 60.14% in 2020.
Discussion
According to the data analyzed in this study, TB is a disease that persists in the Colombian epidemiological setting and, additionally, shows an increase in its incidence and mortality rates, making it a national public health problem.
According to our findings, TB mainly affects the population between 20 and 34 years of age (32.30%), followed by the 35 to 54 years age group (26.40%). In addition, it was noted that there is a significant proportion of individuals aged 65 years or older suffering from this disease (20.61%) and that there was an increase in the number of cases in children under 15 years of age during the period studied, going from 404 in 2019 to 577 in 2022 (2.71% and 3.30% of the annual total, respectively). It was also observed that this disease affects men to a greater extent, with proportions that ranged between 64.89% and 66.70% in the years analyzed.
These findings partially concur with what was reported in Latin America by Escobar,14 who conducted a study detailing the epidemiological situation of TB in Chile in 2018, finding that the TB incidence rate in men was 1.9 times higher than in women and that the highest number of cases was encountered in people with TB between the ages of 25 and 64 years. They are also similar to the results reported by Estigarribia et al.,15 who, in a study in which they clinically and epidemiologically characterized the 659 TB cases registered in the department of Caaguazú (Paraguay) between 2014 and 2017, found that 63.3% of patients were men and that the average age of people with this disease was 35.8 years.
Furthermore, the present study observed a heterogeneous behavior in the TB incidence rate. Although in most population groups an increase was noted, for example, between 2019 and 2022 in specific groups such as migrants and persons deprived of liberty (666 vs. 935 and 997 vs. 1 241, respectively), in other population groups such as street dwellers, Afro-descendants, health workers, children under 15 and indigenous people, a stable or even a decreasing trend was found.
It should be mentioned that, while this study showed an increase in the number of registered TB cases, the country has not met the detection target (90% of cases) established in the National Strategic Plan “Toward the End of Tuberculosis”,9 since only 17 460 cases were detected out of the 25 000 cases estimated by the WHO for 2022 in Colombia,7 which indicates a gap of almost 7 540 undiagnosed cases.
One of the reasons that could explain the low detection of TB cases in Colombia is that, as documented in some studies, there are barriers to access to diagnostic technologies such as molecular tests or liquid cultures, despite the fact that these techniques are included in the Health Benefits Plan and are key for diagnostic algorithms.16-18
On the other hand, the COVID-19 pandemic also had a negative impact (decrease) on TB case detection in 2020 and 2021 in Colombia, which could be explained by a reduction in the uptake of respiratory symptomatic individuals associated with the isolation of the population and reduced access to health services due to biosecurity measures and human mobility restrictions put in place to control the spread of SARS-CoV-2. Similarly, respiratory symptomatic individuals or those with a suspected diagnosis of TB could be classified as suspected COVID-19 cases, which may have influenced the late diagnosis of TB. In addition, there was an increase in the mortality rate among people with TB in 2022 (2.4 cases per 100 000 people), possibly driven by comorbidity with COVID-19, diabetes, HIV, among other diseases, as evidenced in several studies that corroborate how these conditions increase the risk of TB-associated mortality.17-21
In this regard, it should be noted that despite the fact that the Colombian government issued technical guidelines during the COVID-19 health emergency to maintain the continuity of TB prevention and detection services and guarantee a constant supply of anti-TB drugs,22 it was inevitable that both the active search for cases in health institutions and in the community, as well as outreach and education activities on this disease, decreased.
In terms of treatment effectiveness, the goal of the National Strategic Plan “Towards the End of Tuberculosis”9 of achieving successful treatment in more than 90% of cases (new and relapsed) was not met in the years in which it was possible to analyze this variable (2017-2021), with 2019 being the year in which it was closest to this goal (75.00%). Moreover, of the total number of individuals affected by TB (new cases and relapses) in this period (n=63 449), 13.39% died, 9.11% did not complete treatment or did not continue with follow-up, treatment failed in 0.91%, and this aspect was not evaluated in 5.58%. Also, regardless of the use of effective treatment regimens, in MDR/RR-TB cases, the proportion of successful treatment was 60.14% in 2020, which may be associated with difficulties, both individual and social, in adherence and duration of treatment and programmatic barriers that prevent the cure of those affected.23-25
As for persons with TB-HIV coinfection, of the 1 654 cases reported in 2021, only 55.02% were successfully treated (i.e., cured of TB infection after completing antifungal treatment), which is much lower than the percentage of successful treatment found for all TB cases registered that same year (74%). On the contrary, mortality was higher in this subgroup compared to the total number of deaths reported that year (28.78% vs. 13.87%). This is consistent with reports in several studies showing an increased risk of death in people with this co-infection.26,27
A finding for consideration in this study is that diabetes mellitus was a comorbidity in between 7.42% and 9.39% of TB cases registered between 2019 and 2022, a figure that cannot be ignored. In this regard, the presence of this comorbidity in people with TB has been reported by authors such as Hernández-Solís et al.28 who reported in an analytical and retrospective study of cases (n=420) and controls (n=840) treated between 2012 and 2016 in a hospital in Mexico an association between TB and diabetes mellitus (MR=9.1; p=0.000), and also reported that the latter was an important risk factor for the development of TB in 28% of people with pulmonary TB and in 17% of those with extrapulmonary TB.
Another striking finding is the number of health care workers with TB, given that annual cases in this population varied between 224 and 318 (1.59% and 2.14%, respectively) from 2019 to 2022, which may reflect their occupational vulnerability in terms of exposure to this infection due to deficits in safe working conditions and poor infection control in health care institutions. This was also noted by Jurado et al.29 and Muñoz-Sánchez et al.30 in their studies on TB and its prevention in health care institutions from an occupational perspective.
The main strength of this study is that it was possible to consolidate, clean and analyze data of great relevance for TB control in Colombia. However, in view of the limitations of the databases used, it was not possible to describe the information by place of residence in order to organize the data by cities or departments or to calculate the incidences by regions.
Conclusions
According to the data reported, TB incidence and mortality rates in Colombia show an increasing trend. Therefore, it is necessary to make efforts to, first, increase the detection of cases with molecular tests to reach at least a 90% detection rate and, second, achieve an annual rate of successful treatment in at least 90% of cases, as this will allow reversing the mortality curve and accelerate compliance with international goals and the national strategic plan “Towards the End of Tuberculosis” of the Ministry of Health and Social Protection of Colombia.9 In this regard, the need to expand the use of molecular diagnostic techniques, the approach to childhood TB, and integrated and interprogrammatic prevention, as established by the WHO31 in its latest recommendations on TB management, is stressed.
It was also clear that between 2017 and 2021 the frequency of successful treatment was not as desirable. Consequently, it is recommended to implement shortened oral treatment schedules in people with sensitive and resistant TB; strengthen the involvement of those affected, their families and the community with the disease by improving information, education and communication actions on TB management; and expand policies for the care and social protection of people with TB and their families.
Likewise, it is necessary to adopt TB prevention and control measures in health institutions given the alarming number of cases of this disease among health workers observed here. Finally, research and knowledge generation on TB should be strengthened in the country by bringing together academia, scientific societies, research centers, networks of affected persons, and all the actors involved in the management of this disease.32
Conflicts of interest
None stated by the authors.
Funding
None stated by the authors.
Acknowledgments
To the departmental, district and municipal health departments, and to the case notification units involved in surveillance and programmatic reporting of the information submitted to the Ministry of Health and Social Protection.
References
1.España. Ministerio de Trabajo y Economía Social. Instituto Nacional de Seguridad y Salud en el Trabajo (INSST). Mycobacterium tuberculosis. Madrid: INSST; 2021 [cited 2023 Sep 2]. Available from: https://www.insst.es/agentes-biologicos-basebio/bacterias/mycobacterium-tuberculosis.
2.Hameed MM, Alattabi AS, Abolmaali HM. An epidemiological study on common types of tuberculosis in Al-Najaf City. Indian Journal of Public Health Research and Development. 2019;10(9):240-4 https://doi.org/mjkf.
3.Swaminathan N, Perloff SR, Zuckerman JM. Prevention of Mycobacterium tuberculosis Transmission in Health Care Settings. Infect Dis Clin North Am. 2021;35(4):1013-25. https://doi.org/gnkd6t.
4.Organización Panamericana de la Salud (OPS). Directrices unificadas de la OMS sobre la tuberculosis. Módulo 1: Prevención, Tratamiento preventivo de la tuberculosis. Washington D.C.: OPS; 2022.
5.Centers for Disease Control and Prevention (CDC). How TB Spreads. Atlanta: CDC; 2022.
6.World Health Organization (WHO). Tuberculosis. Geneva: WHO; 2023 [cited 2023 Apr 21]. Available from: https://www.who.int/es/news-room/fact-sheets/detail/tuberculosis.
7.World Health Organization (WHO). Global Tuberculosis Report 2023. Geneva: WHO; 2023.
8.Colombia. Ministerio de Salud y Protección Social (MinSalud). Informe de evento Tuberculosis 2022. Bogotá D.C.: MinSalud; 2022 [cited 2023 Sep 12]. Available from: https://www.minsalud.gov.co/sites/rid/Lists/BibliotecaDigital/RIDE/VS/PP/ET/informe-tuberculosis-2022-colombia.pdf.
9.Colombia. Ministerio de Salud y Protección Social (MinSalud). Plan Estratégico ”Hacia el fin de la Tuberculosis”. Colombia 2016-2025. Herramientas de adaptación del Plan Estratégico Colombia Libre de Tuberculosis post 2015. Bogotá D.C.: MinSalud; 2016 [cited 2024 Feb 29]. Available from: https://www.minsalud.gov.co/sites/rid/Lists/BibliotecaDigital/RIDE/INEC/INTOR/Plan-estrategico-fin-tuberculosis-colombia-2016-2025.pdf.
10.World Health Organization (WHO). The end TB strategy. Geneva: WHO; 2015 [cited 2024 Feb 29]. Available from: https://www.who.int/publications-detail-redirect/WHO-HTM-TB-2015.19
11.Colombia. Ministerio de Salud y Protección Social. Resolución 227 de 2020 (febrero 20): Por medio de la cual se adoptan los lineamientos técnicos y operativos del Programa Nacional de Prevención y Control de la Tuberculosis (PNPCT) y se dictan otras disposiciones. Bogotá D.C.: Registro Distrital 6710; January 8 2020 [cited 2021 Oct 26]. Available from: https://bit.ly/3RbzAcD.
12.World Health Organization (WHO). Definitions and reporting framework for tuberculosis - 2013 revision: updated December 2014 and January 2020. Geneva: WHO; 2013 [cited 2023 Nov 18]. Available from: https://www.who.int/publications/i/item/9789241505345.
13.Colombia. Departamento Administrativo Nacional de Estadística (DANE). Proyecciones de población. Bogotá D.C.: DANE; [cited 2023 Jun 15]. Available from: https://www.dane.gov.co/index.php/estadisticas-por-tema/demografia-y-poblacion/proyecciones-de-poblacion.
14.Escobar N. Situación epidemiológica de la tuberculosis en Chile en el escenario global 2018. Rev Chil Enferm Respir. 2019;35(1):63-70, https://doi.org/mjkj.
15.Estigarribia G, Román O, Aguirre S, Sequera G, Aguilar G, Toledo-Núñez SD, et al. Caracterización clínico-epidemiológica de pacientes con tuberculosis en el Departamento de Caaguazú, Paraguay. 2014 a 2017. Rev Chilena Infectol. 2020;37(6):750-5. https://doi.org/mjkm.
16.Rodríguez DA, Verdonck K, Bissell K, Victoria JJ, Khogali M, Marín D, et al. Monitoring delays in diagnosis of pulmonary tuberculosis in eight cities in Colombia. Rev Panam Salud Pública. 2016;39(1):12-8.
17.González-Duran JA, Plaza RV, Luna L, Arbeláez MP, Deviaene M, Keynan Y, et al. Retraso en el tratamiento para VIH, barreras en el acceso a la atención en salud y mortalidad en personas coinfectadas con tuberculosis y VIH en Cali, Colombia. Colomb Med (Cali) 2021;52(4):e2024875.
18.Rodríguez-Márquez I, Montes F, Upegui LD, Montoya N, Vargas NE, Rojas A, et al. Delays in diagnosing pulmonary tuberculosis within a context of medium incidence, Medellín, Colombia, 2017: an operational research. BMC Public Health. 2020;20(1):757. https://doi.org/mjkn.
19.Plata-Casas L, González-Támara L, Cala-Vitery F. Tuberculosis Mortality in Children under Fifteen Years of Age: Epidemiological Situation in Colombia, 2010-2018. Trop Med Infect Dis. 2022;7(7):117. https://doi.org/mjkp.
20.TB/COVID-19 Global Study Group. Tuberculosis and COVID-19 co-infection: description of the global cohort. Eur Respir J. 2022;59(3):2102538. https://doi.org/gnkdzg.
21.Gautam S, Shrestha N, Mahato S, Nguyen TPA, Mishra SR, Berg-Beckhoff G. Diabetes among tuberculosis patients and its impact on tuberculosis treatment in South Asia: a systematic review and meta-analysis. Sci Rep. 2021;11(1):2113. https://doi.org/gm97w4.
22.Colombia. Ministerio de Salud y Protección Social (MinSalud). Lineamientos para la prevención y control de la tuberculosis ante la contingencia de la pandemia por el COVID 19 en Colombia año 2020. Bogotá D.C.: MinSalud; 2020 [cited 2023 Feb 29]. Available from: https://www.minsalud.gov.co/Ministerio/Institucional/Procesos%20y%20procedimientos/GIPS23.pdf.
23.Paniagua-Saldarriaga LA, Pelissari DM, Rueda ZV. Factors associated with unsuccessful outcomes of tuberculosis treatment in 125 municipalities in Colombia 2014 to 2016. Am J Trop Med Hyg. 2021;105(5):1326-34. https://doi.org/mjkr.
24.Muñoz-Sánchez AI, Cruz-Martínez OA, Rubiano-Mesa YL. Trabajadores de la salud y sus significados en torno a la adherencia al tratamiento de la tuberculosis. Enferm Glob. 2013;12(31):86-108.
25.Calle-Ramírez AM, Cuartas-Ramírez JM, Álvarez-Marín T. Factores asociados al éxito del tratamiento de los pacientes con tuberculosis en Medellín, 2014. CES Salud Pública. 2017;8(1):34-47.
26.Fekadu G, Turi E, Kasu T, Bekele F, Chelkeba L, Tolossa T, et al. Impact of HIV status and predictors of successful treatment outcomes among tuberculosis patients: A six-year retrospective cohort study. Ann Med Surg. 2020;60:531-41. https://doi.org/gpfh6t.
27.Ogyiri L, Lartey M, Ojewale O, Adjei AA, Kwara A, Adanu RM, et al. Effect of HIV infection on TB treatment outcomes and time to mortality in two urban hospitals in Ghana-a retrospective cohort study. Pan Afr Med J. 2019;32:206. https://doi.org/mjkq.
28.Hernández-Solís A, Navarro-Reynoso F, Reding-Bernal A. Factores de riesgo en pacientes con tuberculosis pulmonar y extrapulmonar en un hospital de concentración de la Ciudad de México. Salud pública Méx. 2020;62(4):452. https://doi.org/mjks.
29.Jurado LF, Barrera V, De la Rosa-Noriega ZR, Serpa C, Baldión M, Pinzón B, et al. Tuberculosis among health care workers treated at a university hospital in Bogotá D.C., Colombia. 2008-2018. Rev. Fac. Med. 2022;70(1):e90501. https://doi.org/hppr.
30.Muñoz-Sánchez AI, Rubiano-Mesa YL, Saavedra-Cantor CJ. Medidas de control de la infección por tuberculosis: un desafío colectivo para las instituciones de salud. In: Chaparro-Díaz L, editor. Avances de investigación en la Facultad de Enfermería. Bogotá D.C.: Editorial UN; 2022.
31.Wolrd Health Organization (WHO). WHO Operational handbook on tuberculosis. Module 4: treatment - drug-resistant tuberculosis treatment, 2022 update. Geneva: WHO; 2022.
32.Rincón-Torres CE, Rubio V, Castro C, García I, Cruz OA, Trujillo-Trujillo J, et al. Red Nacional de Gestión de Conocimiento, Investigación e Innovación en Tuberculosis en Colombia. Rev Panam Salud Pública. 2021;45:e23. https://doi.org/mjkv.
Referencias
España. Ministerio de Trabajo y Economía Social. Instituto Nacional de Seguridad y Salud en el Trabajo (INSST). Mycobacterium tuberculosis. Madrid: INSST; 2021 [cited 2023 Sep 2]. Available from: https://www.insst.es/agentes-biologicos-basebio/bacterias/mycobacterium-tuberculosis.
Hameed MM, Alattabi AS, Abolmaali HM. An epidemiological study on common types of tuberculosis in Al-Najaf City. Indian Journal of Public Health Research and Development. 2019;10(9):240-4 https://doi.org/mjkf.
Swaminathan N, Perloff SR, Zuckerman JM. Prevention of Mycobacterium tuberculosis Transmission in Health Care Settings. Infect Dis Clin North Am. 2021;35(4):1013-25. https://doi.org/gnkd6t.
Organización Panamericana de la Salud (OPS). Directrices unificadas de la OMS sobre la tuberculosis. Módulo 1: Prevención, Tratamiento preventivo de la tuberculosis. Washington D.C.: OPS; 2022. DOI: https://doi.org/10.26633/RPSP.2022.172
Centers for Disease Control and Prevention (CDC). How TB Spreads. Atlanta: CDC; 2022.
World Health Organization (WHO). Tuberculosis. Geneva: WHO; 2023 [cited 2023 Apr 21]. Available from: https://www.who.int/es/news-room/fact-sheets/detail/tuberculosis.
World Health Organization (WHO). Global Tuberculosis Report 2023. Geneva: WHO; 2023.
Colombia. Ministerio de Salud y Protección Social (MinSalud). Informe de evento Tuberculosis 2022. Bogotá D.C.: MinSalud; 2022 [cited 2023 Sep 12]. Available from: https://www.minsalud.gov.co/sites/rid/Lists/BibliotecaDigital/RIDE/VS/PP/ET/informe-tuberculosis-2022-colombia.pdf.
Colombia. Ministerio de Salud y Protección Social (MinSalud). Plan Estratégico ”Hacia el fin de la Tuberculosis”. Colombia 2016-2025. Herramientas de adaptación del Plan Estratégico Colombia Libre de Tuberculosis post 2015. Bogotá D.C.: MinSalud; 2016 [cited 2024 Feb 29]. Available from: https://www.minsalud.gov.co/sites/rid/Lists/BibliotecaDigital/RIDE/INEC/INTOR/Plan-estrategico-fin-tuberculosis-colombia-2016-2025.pdf.
World Health Organization (WHO). The end TB strategy. Geneva: WHO; 2015 [cited 2024 Feb 29]. Available from: https://www.who.int/publications-detail-redirect/WHO-HTM-TB-2015.19
Colombia. Ministerio de Salud y Protección Social. Resolución 227 de 2020 (febrero 20): Por medio de la cual se adoptan los lineamientos técnicos y operativos del Programa Nacional de Prevención y Control de la Tuberculosis (PNPCT) y se dictan otras disposiciones. Bogotá D.C.: Registro Distrital 6710; January 8 2020 [cited 2021 Oct 26]. Available from: https://bit.ly/3RbzAcD.
World Health Organization (WHO). Definitions and reporting framework for tuberculosis - 2013 revision: updated December 2014 and January 2020. Geneva: WHO; 2013 [cited 2023 Nov 18]. Available from: https://www.who.int/publications/i/item/9789241505345.
Colombia. Departamento Administrativo Nacional de Estadística (DANE). Proyecciones de población. Bogotá D.C.: DANE; [cited 2023 Jun 15]. Available from: https://www.dane.gov.co/index.php/estadisticas-por-tema/demografia-y-poblacion/proyecciones-de-poblacion.
Escobar N. Situación epidemiológica de la tuberculosis en Chile en el escenario global 2018. Rev Chil Enferm Respir. 2019;35(1):63-70, https://doi.org/mjkj.
Estigarribia G, Román O, Aguirre S, Sequera G, Aguilar G, Toledo-Núñez SD, et al. Caracterización clínico-epidemiológica de pacientes con tuberculosis en el Departamento de Caaguazú, Paraguay. 2014 a 2017. Rev Chilena Infectol. 2020;37(6):750-5. https://doi.org/mjkm.
Rodríguez DA, Verdonck K, Bissell K, Victoria JJ, Khogali M, Marín D, et al. Monitoring delays in diagnosis of pulmonary tuberculosis in eight cities in Colombia. Rev Panam Salud Pública. 2016;39(1):12-8.
González-Duran JA, Plaza RV, Luna L, Arbeláez MP, Deviaene M, Keynan Y, et al. Retraso en el tratamiento para VIH, barreras en el acceso a la atención en salud y mortalidad en personas coinfectadas con tuberculosis y VIH en Cali, Colombia. Colomb Med (Cali) 2021;52(4):e2024875.
Rodríguez-Márquez I, Montes F, Upegui LD, Montoya N, Vargas NE, Rojas A, et al. Delays in diagnosing pulmonary tuberculosis within a context of medium incidence, Medellín, Colombia, 2017: an operational research. BMC Public Health. 2020;20(1):757. https://doi.org/mjkn.
Plata-Casas L, González-Támara L, Cala-Vitery F. Tuberculosis Mortality in Children under Fifteen Years of Age: Epidemiological Situation in Colombia, 2010-2018. Trop Med Infect Dis. 2022;7(7):117. https://doi.org/mjkp.
TB/COVID-19 Global Study Group. Tuberculosis and COVID-19 co-infection: description of the global cohort. Eur Respir J. 2022;59(3):2102538. https://doi.org/gnkdzg.
Gautam S, Shrestha N, Mahato S, Nguyen TPA, Mishra SR, Berg-Beckhoff G. Diabetes among tuberculosis patients and its impact on tuberculosis treatment in South Asia: a systematic review and meta-analysis. Sci Rep. 2021;11(1):2113. https://doi.org/gm97w4.
Colombia. Ministerio de Salud y Protección Social (MinSalud). Lineamientos para la prevención y control de la tuberculosis ante la contingencia de la pandemia por el COVID 19 en Colombia año 2020. Bogotá D.C.: MinSalud; 2020 [cited 2023 Feb 29]. Available from: https://www.minsalud.gov.co/Ministerio/Institucional/Procesos%20y%20procedimientos/GIPS23.pdf.
Paniagua-Saldarriaga LA, Pelissari DM, Rueda ZV. Factors associated with unsuccessful outcomes of tuberculosis treatment in 125 municipalities in Colombia 2014 to 2016. Am J Trop Med Hyg. 2021;105(5):1326-34. https://doi.org/mjkr.
Muñoz-Sánchez AI, Cruz-Martínez OA, Rubiano-Mesa YL. Trabajadores de la salud y sus significados en torno a la adherencia al tratamiento de la tuberculosis. Enferm Glob. 2013;12(31):86-108. DOI: https://doi.org/10.6018/eglobal.12.3.151901
Calle-Ramírez AM, Cuartas-Ramírez JM, Álvarez-Marín T. Factores asociados al éxito del tratamiento de los pacientes con tuberculosis en Medellín, 2014. CES Salud Pública. 2017;8(1):34-47.
Fekadu G, Turi E, Kasu T, Bekele F, Chelkeba L, Tolossa T, et al. Impact of HIV status and predictors of successful treatment outcomes among tuberculosis patients: A six-year retrospective cohort study. Ann Med Surg. 2020;60:531-41. https://doi.org/gpfh6t.
Ogyiri L, Lartey M, Ojewale O, Adjei AA, Kwara A, Adanu RM, et al. Effect of HIV infection on TB treatment outcomes and time to mortality in two urban hospitals in Ghana-a retrospective cohort study. Pan Afr Med J. 2019;32:206. https://doi.org/mjkq.
Hernández-Solís A, Navarro-Reynoso F, Reding-Bernal A. Factores de riesgo en pacientes con tuberculosis pulmonar y extrapulmonar en un hospital de concentración de la Ciudad de México. Salud pública Méx. 2020;62(4):452. https://doi.org/mjks.
Jurado LF, Barrera V, De la Rosa-Noriega ZR, Serpa C, Baldión M, Pinzón B, et al. Tuberculosis among health care workers treated at a university hospital in Bogotá D.C., Colombia. 2008-2018. Rev. Fac. Med. 2022;70(1):e90501. https://doi.org/hppr.
Muñoz-Sánchez AI, Rubiano-Mesa YL, Saavedra-Cantor CJ. Medidas de control de la infección por tuberculosis: un desafío colectivo para las instituciones de salud. In: Chaparro-Díaz L, editor. Avances de investigación en la Facultad de Enfermería. Bogotá D.C.: Editorial UN; 2022.
Wolrd Health Organization (WHO). WHO Operational handbook on tuberculosis. Module 4: treatment - drug-resistant tuberculosis treatment, 2022 update. Geneva: WHO; 2022.
Rincón-Torres CE, Rubio V, Castro C, García I, Cruz OA, Trujillo-Trujillo J, et al. Red Nacional de Gestión de Conocimiento, Investigación e Innovación en Tuberculosis en Colombia. Rev Panam Salud Pública. 2021;45:e23. https://doi.org/mjkv.
Cómo citar
APA
ACM
ACS
ABNT
Chicago
Harvard
IEEE
MLA
Turabian
Vancouver
Descargar cita
CrossRef Cited-by
1. Alvaro D. Orjuela-Cañón. (2025). BERT-Based Approach for Tuberculosis Diagnosis from Electronic Medical Records. 2025 IEEE Latin American Conference on Computational Intelligence (LA-CCI). , p.1. https://doi.org/10.1109/LA-CCI66231.2025.11270453.
2. Juan C. Polo, Jesus M. Angulo-Mercado, Sandra M. Coronado-Ríos, Fernando de la Vega, Edwin D. Correa, Nelson E. Arenas. (2026). Dynamic Biochemical Phenotypes in Hospitalized Patients with Pulmonary Tuberculosis. Sci, 8(2), p.35. https://doi.org/10.3390/sci8020035.
Dimensions
PlumX
Visitas a la página del resumen del artículo
Descargas
Licencia
Derechos de autor 2024 Revista de la Facultad de Medicina

Esta obra está bajo una licencia Creative Commons Reconocimiento 3.0 Unported.
-





















