Gestational obesity as a determinant of general anesthesia technique for caesarean delivery: a case report.
Obesidad en la gestación como determinante de técnica anestésica general para cesárea: reporte de caso
Palabras clave:
obesidad, gestación, anestesia obstétrica, anestesia general. (en)obesity, pregnancy, obstetrics, anesthesia, general anesthesia. (es)
Background. The incidence of obesity has undergone a dramatic increase around the world during the last few years. Such epidemic behavior has been associated with obstetric patient’s frequent presentation of different stages of obesity when undergoing anesthetic procedure. Obesity in pregnant women involves the risk of adverse maternal and fetal outcomes. Hypertension and preeclampsia, diabetes, fetal macrosomia, caesarean delivery, difficult airway management and neuroaxial techniques are more likely to be performed in this group of patients.
Materials and methods. This is a case report of a morbid obese patient scheduled for caesarean delivery and tubal ligation. Regional, spinal and epidural techniques were attempted for surgery with unsuccessful results; this entails general anesthesia for surgery. The literature on complications due to obesity during pregnancy was reviewed, emphasising relevance for the anesthesiologist.
Conclusion.Obesity, especially morbid obesity in pregnant women, represents a challenge for anesthesia management. Updated knowledge of physiology and the conditions related to obesity in pregnancy is necessary; medical services must be prepared to provide optimum and safe obstetric anesthesia, analgesia and post-operation care.
Antecedentes. La incidencia de obesidad ha tenido un incremento importante en los últimos años a nivel global. Este comportamiento epidémico ha llevado a la presentación cada vez más frecuente de pacientes obstétricas con diversos grados de obesidad para procedimientos anestésicos. La obesidad en la paciente gestante tiene asociación con desenlaces adversos maternos y fetales, incremento en el riesgo de hipertensión y trastornos hipertensivos, diabetes, macrosomía fetal, nacimiento por cesárea, además de dificultad para realizar técnicas neuroaxiales y para el manejo de la vía aérea.
Material y métodos.Este es un reporte de caso de una paciente obesa extrema programada para cesárea segmentaria y esterilización tubárica. Se intentó la realización del procedimiento bajo anestesia neuroaxial subaracnoidea y epidural, sin éxito. Esto condicionó el empleo de anestesia general. Se realizó una revisión personal de la literatura que incluye las complicaciones relacionadas con obesidad durante la gestación de relevancia para el anestesiólogo.
Conclusión. La obesidad, especialmente cuando es extrema, representa un reto para el manejo anestésico de la paciente obstétrica. Es importante conocer la fisiología y las condiciones asociadas con la obesidad en la gestación y disponer de los recursos necesarios para conducir de forma segura la analgesia, la anestesia obstétrica y el cuidado postoperatorio.
CASE PRESENTATION
GESTATIONAL OBESITY AS A DETERMINANT OF GENERAL ANESTHESIA TECHNIQUE FOR CAESAREAN DELIVERY: A CASE REPORT
Obesidad en la gestación como determinante de técnica anestésica general para cesárea: reporte de caso>
José Ricardo Navarro-Vargas1, José Luis Aldana-Díaz2, Javier H. Eslava-Schamalbach3
1 MD. Associate Profesor, Anaesthesiology and Reanimation, Universidad Nacional de Colombia, Bogotá. Summary
Background. The incidence of obesity has undergone a
dramatic increase around the world during the last few
years. Such epidemic behavior has been associated with
obstetric patients frequent presentation of different
stages of obesity when undergoing anesthetic procedure.
Obesity in pregnant women involves the risk of adverse
maternal and fetal outcomes. Hypertension and
preeclampsia, diabetes, fetal macrosomia, caesarean
delivery, difficult airway management and neuroaxial
techniques are more likely to be performed in this group
of patients.
Materials and methods. This is a case report of a
morbid obese patient scheduled for caesarean delivery
and tubal ligation. Regional, spinal and epidural
techniques were attempted for surgery with unsuccessful
results; this entails general anesthesia for surgery. The
literature on complications due to obesity during
pregnancy was reviewed, emphasising relevance for the
anesthesiologist.
Conclusion.Obesity, especially morbid obesity in
pregnant women, represents a challenge for anesthesia
management. Updated knowledge of physiology and
the conditions related to obesity in pregnancy is
necessary; medical services must be prepared to provide
optimum and safe obstetric anesthesia, analgesia and
post-operation care.
Key words: obesity, pregnancy, obstetrics, anesthesia,
general anesthesia.
Navarro-Vargas JR, Aldana-Díaz JL, Eslava-
Schamalbach JH. Gestational obesity as a determinant of
general anesthesia technique for caesarean delivery: a case
report. rev.fac.med. 2009; 57: 281-286.
Resumen
Antecedentes. La incidencia de obesidad ha tenido un
incremento importante en los últimos años a nivel global.
Este comportamiento epidémico ha llevado a la presentación
cada vez más frecuente de pacientes obstétricas con
diversos grados de obesidad para procedimientos
anestésicos. La obesidad en la paciente gestante tiene asociación
con desenlaces adversos maternos y fetales, incremento
en el riesgo de hipertensión y trastornos
hipertensivos, diabetes, macrosomía fetal, nacimiento por
cesárea, además de dificultad para realizar técnicas
neuroaxiales y para el manejo de la vía aérea.
Material y métodos.Este es un reporte de caso de una
paciente obesa extrema programada para cesárea segmentaria
y esterilización tubárica. Se intentó la realización del procedimiento
bajo anestesia neuroaxial subaracnoidea y
epidural, sin éxito. Esto condicionó el empleo de anestesia
general. Se realizó una revisión personal de la literatura que
incluye las complicaciones relacionadas con obesidad durante
la gestación de relevancia para el anestesiólogo.
Conclusión. La obesidad, especialmente cuando es extrema,
representa un reto para el manejo anestésico de la
paciente obstétrica. Es importante conocer la fisiología y
las condiciones asociadas con la obesidad en la gestación
y disponer de los recursos necesarios para conducir de
forma segura la analgesia, la anestesia obstétrica y el cuidado
postoperatorio.
Palabras clave: obesidad, gestación, anestesia obstétrica,
anestesia general
Navarro-Vargas JR, Aldana-Díaz JL, Eslava-
Schamalbach JH. Obesidad en la gestación como determinante
de técnica anestésica general para cesárea: reporte
de caso. rev.fac.med. 2009; 57: 281-286.
Introduction Obesity and being overweight represent a public
health problem in both developed and
underdeveloped countries (1). Such epidemic
behavior poses new challenges for individual
medical practice and health systems (2-3).. There
has been an increase in the prevalence of obesity
and being overweight in reproductive-aged
women; this has been estimated as being 30.2
percent and 56.7 percent respectively in the USA,
leading to a high prevalence of obesity during
pregnancy and complications arising from this (4). In our country on 30 September 2009, became a
presidential signing the law ordering the
Colombian state, caring for all citizens who are
morbidly obese (5). According to National Health
Survey, in Colombia there are 5.7 million of obese
and 15.4 million with overweight. Approximately
49 percent of women between 14 and 64 years
and 39 percent of men in this age range suffer
from obesity (6). The literature contains different definitions for
normality, being overweight and obesity; the most
accepted one relies on the body mass index
(BMI), normality being established as having
18.524.9 Kg/m2
BMI, being overweight as 25
29.9 Kg/m2
BMI and obesity being classified into
the following three categories: class 1 3035 Kg/
m2
BMI, class 2 3540 Kg/m2
BMI and class 3
and extreme obesity > 40 Kg/m2
BMI (7). Obesity is defined as being a gain in weight
during pregnancy greater than 110120 percent
of ideal body weight by first prenatal control,
absolute pregnant weight greater than 90 kg or
greater than 30 kg/ m2 BMI. Some limits to
weight-gain have also been defined according
to pre-pregnancy weight. An obese patient
should undergo a weight increase of less than
7.5 kg, an overweight one 7.5 to 12.5 kg and
normal weight female 12.5 to 15 kg (6). Around
6 percent to 10 percent of pregnancies are
associated with obesity, 0.43 percent to 3 percent
corresponding to extreme obesity (8).
Obstetric complications of obesity
2MD. Postgraduate student in Anaesthesiology and Reanimation, Universidad Nacional de Colombia, Bogotá.
3MD. MSC. PhD. Director, Clinical Research Institute, Universidad Nacional de Colombia, Bogotá
Correspondencia: jrnavarrov@unal.edu.co
Regarding fetal complications, the greater incidence of congenital malformations should be stressed, especially neural tube defects (11-12), fetal macrosomia, as conditioning complications during labor (dystocia of the shoulders and caesarean section) (7). Obstetric ecographys usefulness is limited for detecting such alterations from the technical point of view (2).
Increased fatty tissue hampers invasive and noninvasive monitoring of blood-pressure and airway management for the anesthesiologist (13). The latter risk is of special interest according to reports of such high intubation failure rate (up to 33%), representing (together with gastric aspiration) the main causes of anesthesia-related deaths (13-14). It may be impossible to perform regional techniques if suitable length devices are not available and they also present a greater failure rate than when used in patients who are not obese (13). Gestational obesity is a preventable risk factor which must be a priority in public health measures orientated towards promoting healthy life-styles and training health service providers so that they intervene through education and preventing associated complications (7-9).
Clinical case
The case of a 33-year old patient who was 38 weeks pregnant is reported; she was programmed for caesarean section plus tubaric sterilization at La Victoria Instituto Materno Infantil Hospital (state hospital company) in Bogotá, Colombia.She had an obstetric history of three pregnancies, having had two eutocic vaginal births. Pregnancy was controlled to full term; she was classified as being extremely obese, weighing 152 Kg (64.1 Kg/m2 BMI). She had a background of hypohyroidism diagnosed four years ago; this had been controlled by receiving 50 mcg/ day of Lthyroxin. She had no background of chronic hypertension or hypertensive complications of pregnancy. Gestational diabetes was excluded during prenatal controls.
The following vital signs were noted during physical examination: FC 117, Fr 18, PA 119/82 M 94; predicted difficulty for laryngoscope: 7 cm chin-thyroid distance, 5 cm oral aperture, regular cervical mobility, 1 tonguepharynx ratio; removable upper prosthesis; abdomen having abundant adipose panicula and pregnant uterus. There were no other remarkable alterations. Paraclinical signs: Hb 13, 37.8 percent hematocrite, 0.72 mg/dL creatinine, 108 mL/min creatinine clearance, negative proteinuria.
The informed consent was signed and the risks and complications were explained; it was decided to use a neuroaxial subarachnoideal anesthetic technique. A conventional surgical table was used, 18 g peripheral venous access, pulse oxymetry, cardiovisoscopy and non-invasive blood pressure monitoring with standard adult-sized tube (12 cm).
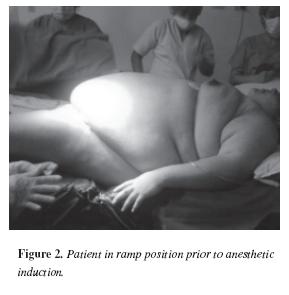
A lumbar puncture was unsuccessfully attempted using Quincke caliber 27 g 88 mm needle . Faced by such limitation, another attempt was made at epidural anesthesia with Touhy caliber 17 91 mm needle without managing to localize the epidural space. The patient was then given general anesthesia in view of the impossibility of performing a regional technique. She received 10 mg metoclopramide and 50 mg ranitidine 20 minutes before anesthetic induction. Rapid sequence induced with 150 mcg fentanyl, 400 mcg sodium thiopental, 200 mg succinilcoline; orotracheal intubation in ramp position using 7.5 mm tube, Cormack and Lehane laryngoscopy I. Inhalatory maintenance with 2.6 percent sevofluorane and additional relaxation with 20 mg rocuronium. Three gynecologistobstetricians participated in the procedure, 10 minute cutaneous incision extraction time. Female new-born, weighed 2,820 g, 45 cm length, 36 week gestational age (Capurro), 4, 9, 10 Apgar at 1, 5 and 10 minutes, respectively. Diagnosed as pre-term new-born; weight adequate for gestational age. She was hospitalized in the neonatal unit for basic care as she presented hypoglycemia.
Reversal of neuromuscular block with 2 mg neostigmin, 1 mg atropine applied. Awake extubation. No complications were presented. Time in surgery was 75 minutes and time under anesthetic 90 minutes (figure 1) (figure 2).
Discussion
Obesity significantly increases the incidence of cesarean birth, 20.7, 33.8 and 47.4 percent for nulipar patients having normal, obese and morbid obese BMI, respectively (15). There is also an association with increased risk of morbidity, mortality and operation and anesthetic complications (7-16).Such context poses the need for multidisciplinary management since the moment of pre-anesthetic evaluation for the early detection of alterations during the course of pregnancy and minimizing the maternal and fetal risk of adverse events occurring. Suitable communication is required between obstetricians, anesthesiologists and nursing personnel for managing the obese patient during labor or cesarean section (13). The indications for a cesarean section must have already been very clearly defined, being identical to those for non-obese patients and vaginal birth should have been promoted by offering epidural analgesia (15).
The technical limitations must be recognized, as must the lack of availability of sufficient resources conditioning using general anesthesia for this procedure. The necessary equipment must be available in operating rooms for monitoring these patients, such as non-invasive blood pressure measurement tubes, suitable surgical tables for 300 kg weights, suitable length needles for subarachnoideal (Spinocan 120 mm Braun, Germany), epidural (Perican 150 mm, Braun, Germany) and anesthetic combined puncture (Spocan 150 mm, Braun, Germany) (13-17).
In spite of the preference for regional anesthesia for carrying out cesarean section (due to the possibility of encountering difficulty when managing the airway and the risk of bronchoaspiration), choosing subarachnoideal anesthesia could be inadequate given the following considerations. Firstly, local anesthetic dissemination could be unpredictable and high levels of spinal blocking could be reached.
A lesser average volume of cephalorachidian liquid and the presence of soft fatty tissue have been found in intervertebral foramen in obese patients as an explanation for lower anesthetic requirement (13), added to increased intra-abdominal pressure, cava and ingurgitation compression of the epidural venous plexus (18). Secondly, a single dose of anesthetic could prove insufficient, assuming a technically more timeconsuming procedure having probable complications such as uterine atony and excessive intra-operation bleeding (13).
Even though the continuous epidural technique could resolve this problem, a greater than 25 percent failure rate has been reported for this technique in these patients (19) due to difficulty in localizing the space and blocking sacral roots, thereby leading to visceral pain when manipulating the uterine segment and the bladder. It would thus seem more useful to recur to the combined technique for achieving subarachnoideal blocking quality and epidural catheter flexibility (13).
Balki et al., studied 46 obese parturients, with pregnancy body mass index (BMI) > 30 Kg/ M2 (MBI: 33-86 Kg/M2), requesting labor epidural analgesia. They demonstrated that ultrasound imaging in the transverse plane had a strong correlation between the ultrasound estimated distance to the epidural space and the actual distance measured by the needle in obese parturients. They suggest that prepuncture lumbar ultrasound may be a useful guide to facilitate the placement of epidural needles in obese parturients (20).
General anesthesia appears to be an alternative in elective cesarean section today and the sole technique for use with the critical obstetric patient (21). Difficulty should be foreseen for intubation, pre-oxygenating and in having resources available for managing the difficult airway; prophylaxis using gastric aspiration with particulate antacids and prokinetics should be considered (13-22). In spite of this technique being used, no reduction in Apgar score has been demonstrated in the newborn at 5 and 10 minutes when extraction (cutaneous incision extraction time) has been less than five minutes (21). Extraction took 10 minutes in the case reported here. The availability of a neonatal critical care unit thus becomes fundamental for the above and other neonatal complications related to the obesitygestational diabetes spectrum.
Publishing this case has been aimed at alerting obstetric attention-providing institutions to the deficiencies which many of them present in terms of providing integral attention for this type of patient and the fruit of pregnancy. It has also highlighted the challenge implied in its anesthetic-surgical management.
References
1. Cretikos M, Valenti L, Britt H, Baur L. General practice management of overweight and obesity in children and adolescents in Australia. Med Care. 2008; 46: 1163-1169.2. Catalano P. Management of obesity in pregnancy. Obstet Gynecol. 2007; 109: 419-33.
3. World Health Organization. Obesity: preventing and managing a global epidemic. World Health Organ Tech Rep Ser. 2000; 894: 1-4.
4. Ogden CL, Flegal KM, Carrol MD, Jonhson CL. Prevalence and trends in overweight among US children and adolescents. JAMA. 2002; 288: 1728-32.
5. Castro L, Avina R. Maternal obesity and pregnancy outcomes. Curr Opin Obstet Gynecol. 2002; 14: 601- 606.
6. Colprensa. Obesidad será problema de salud pública. Cali-Colombia. 30 de septiembre de 2009.
7. Encuesta Nacional de Salud ENS. Centro de Proyectos para el Desarrollo (Cendex), de la Universidad Javeriana, y la firma Sistemas Especializados de Información (SEI). 2007.
8. Cedergren, M. Maternal morbid obesity and the risk of adverse pregnancy outcome. Obstet Gynecol. 2004; 103: 2219-2224.
9. Hall L, Neubert G. Obesity and Pregnancy. Obstetrical & Gynecological Survey. 2005; 60, 4: 253-260.
10. Cnattingius S, Bergstrom R, Lipworth L, Kramer MS. Pre-pregnancy weight and the risk of adverse pregnancy outcomes. N Engl J Med 1998; 338: 147-152.
11. Ramechenderan J, Bradford J, McLean M. Maternal obesity and pregnancy complications: A review. Aust & New Zealand J of Obsts & Gyn. 2008; 48: 228-235.
12. Shu S, Kim S, Lau J, Schmid C, Dietz P, Callaghan W, Curtis K. Maternal obesity and risk of stillbirth: a meta-analysis. Am J Obstet Gynecol. 2007. 197: 223-228.
13. Soens M, Jayanthie B, Van Zundert A. Obstetric anesthesia for the obese and morbidity obese patient: an ounce of prevention is worth more than a pound of treatment. Acta Anaesthesiol Scand. 2008; 52: 6-19.
14. Goldszmidt E. Principles and practices of obstetric airway management. Anesthesiology Clin. 2008; 26: 109-125.
15. Weiss J, Malone F, Emig D. Obesity, obstetric complications and cesarean delivery rate a population based screening study. Am J Obstet Gynecol. 2004; 190: 1092-1097.
16. Perlow J, Morgan M. Massive maternal obesity and perioperative cesarean morbidity. Am J Obstet Gynecol. 1994; 170: 560-564.
17. Spinal Anesthesia Needles Spinocan Pencan Atraucan. Available on internet (November 2008): www.bbraun.com/index.cfm
18. Hill C, Pickinpaugh J. Physiologic changes in pregnancy. Surg Clin N Am. 2008; 88: 391-401.
19. Hood D, Dewan D, Kashtan K. Anesthesia outcome in the morbid obese parturient. Anesthesiology. 1993; 79: 1210-1218.
20. Balki M, Lee Y, Halpern S, Carvalho J. Ultrasound Imaging of the lumbar spine in the transverse plane: The correlation between estimated and actual depth to the epidural space in obese parturients. Anesth & Analg. 2009; 108: 1876-1881.
21. Affolabi B, Lesi F, Merah N. Regional versus general anaesthesia for caesarean section (Review). The Cochrane Library. 2008; 3: 1-44.
22. Gyte G, Richens Y. Routine prophylactic drugs in normal labour for reducing gastric aspiration and its effects (Review). The Cochrane Library. 2008; 3: 1- 24.
Referencias
Cretikos M, Valenti L, Britt H, Baur L. General practice management of overweight and obesity in children and adolescents in Australia. Med Care. 2008; 46: 1163-1169.
Catalano P. Management of obesity in pregnancy. Obstet Gynecol. 2007; 109: 419-33.
World Health Organization. Obesity: preventing and managing a global epidemic. World Health Organ Tech Rep Ser. 2000; 894: 1-4.
Ogden CL, Flegal KM, Carrol MD, Jonhson CL. Prevalence and trends in overweight among US children and adolescents. JAMA. 2002; 288: 1728-32.
Castro L, Avina R. Maternal obesity and pregnancy outcomes. Curr Opin Obstet Gynecol. 2002; 14: 601- 606.
Colprensa. Obesidad será problema de salud pública. Cali-Colombia. 30 de septiembre de 2009.
Encuesta Nacional de Salud ENS. Centro de Proyectos para el Desarrollo (Cendex), de la Universidad Javeriana, y la firma Sistemas Especializados de Información (SEI). 2007.
Cedergren, M. Maternal morbid obesity and the risk of adverse pregnancy outcome. Obstet Gynecol. 2004; 103: 2219-2224.
Hall L, Neubert G. Obesity and Pregnancy. Obstetrical & Gynecological Survey. 2005; 60, 4: 253-260.
Cnattingius S, Bergstrom R, Lipworth L, Kramer MS. Pre-pregnancy weight and the risk of adverse pregnancy outcomes. N Engl J Med 1998; 338: 147-152.
Ramechenderan J, Bradford J, McLean M. Maternal obesity and pregnancy complications: A review. Aust & New Zealand J of Obsts & Gyn. 2008; 48: 228-235.
Shu S, Kim S, Lau J, Schmid C, Dietz P, Callaghan W, Curtis K. Maternal obesity and risk of stillbirth: a meta-analysis. Am J Obstet Gynecol. 2007. 197: 223-228.
Soens M, Jayanthie B, Van Zundert A. Obstetric anesthesia for the obese and morbidity obese patient: an ounce of prevention is worth more than a pound of treatment. Acta Anaesthesiol Scand. 2008; 52: 6-19.
Goldszmidt E. Principles and practices of obstetric airway management. Anesthesiology Clin. 2008; 26: 109-125.
Weiss J, Malone F, Emig D. Obesity, obstetric complications and cesarean delivery rate –a population based screening study. Am J Obstet Gynecol. 2004; 190: 1092-1097.
Perlow J, Morgan M. Massive maternal obesity and perioperative cesarean morbidity. Am J Obstet Gynecol. 1994; 170: 560-564.
Spinal Anesthesia Needles – Spinocan – Pencan– Atraucan–. Available on internet (November 2008): www.bbraun.com/index.cfm
Hill C, Pickinpaugh J. Physiologic changes in pregnancy. Surg Clin N Am. 2008; 88: 391-401.
Hood D, Dewan D, Kashtan K. Anesthesia outcome in the morbid obese parturient. Anesthesiology. 1993; 79: 1210-1218.
Balki M, Lee Y, Halpern S, Carvalho J. Ultrasound Imaging of the lumbar spine in the transverse plane: The correlation between estimated and actual depth to the epidural space in obese parturients. Anesth & Analg. 2009; 108: 1876-1881.
Affolabi B, Lesi F, Merah N. Regional versus general anaesthesia for caesarean section (Review). The Cochrane Library. 2008; 3: 1-44.
Gyte G, Richens Y. Routine prophylactic drugs in normal labour for reducing gastric aspiration and its effects (Review). The Cochrane Library. 2008; 3: 1- 24.
Cómo citar
APA
ACM
ACS
ABNT
Chicago
Harvard
IEEE
MLA
Turabian
Vancouver
Descargar cita
Visitas a la página del resumen del artículo
Descargas
Licencia
Derechos de autor 2009 Revista de la Facultad de Medicina

Esta obra está bajo una licencia Creative Commons Reconocimiento 3.0 Unported.
-