Experience and results of laparoscopic inguinal herniorrhaphy
Experiencia y resultados de la herniorrafia inguinal por laparoscopia
DOI:
https://doi.org/10.15446/revfacmed.v65n3.56429Palabras clave:
Hernia, Laparoscopy, Recurrence (en)Hernia, Laparoscopia, Recurrencia (es)
Descargas
Introduction: Due to the invention of minimally invasive surgery, inguinal hernia repair by laparoscopy has become a common procedure. This paper presents the results of 92 inguinal hernia repairs by laparoscopy performed using the transabdominal pre-peritoneal technique (TAPP) between August 2001 and January 2014.
Objective: To present our results regarding recurrence rate, postoperative pain and need for conversion.
Materials and methods: The results of the procedure using TAPP were retrospectively analyzed based on an average follow-up time of 8 years.
Results: Three (3.2%) cases required conversion, three (3.2%) were recurrent and six (6.4%) presented chronic pain.
Conclusion: Laparoscopic hernia repair by TAPP is a safe procedure. Effectiveness and complication rates have shown to be similar to open and TEP techniques.
Introducción. Con la invención de la cirugía poco invasiva, la herniorrafia inguinal por laparoscopia se ha convertido en un procedimiento de realización frecuente. En el presente artículo se publican los resultados de 92 herniorrafias inguinales por laparoscopia realizadas con técnica transabdominal preperitoneal (TAPP) entre agosto de 2001 y enero de 2014.
Objetivo. Presentar resultados en cuanto a tasa de recurrencia, dolor post-operatorio y necesidad de conversión en las herniorrafias inguinales por laparoscopia analizadas.
Materiales y métodos. Se analizaron de manera retrospectiva los resultados del procedimiento realizando técnica TAPP con seguimiento promedio de 8 años.
Resultados. Se presentaron tres (3.2%) casos que requirieron conversión, tres (3.2%) de recurrencia y seis (6.4%) de dolor crónico.
Conclusión. La herniorrafia por laparoscopia con técnica TAPP es un procedimiento seguro; esta tiene tasas similares de efectividad y complicaciones a la técnica abierta y totalmente extraperitoneal TEP.
Original research
DOI: https://doi.org/10.15446/revfacmed.v65n3.56429
Experience and results of laparoscopic inguinal herniorrhaphy
Experiencia y resultados de la herniorrafia inguinal por laparoscopia
Received: 24/03/2016. Accepted: 19/06/2016.
Héctor René Hazbón1 • David Felipe López-Atehortua1
1 Universidad Nacional de Colombia - Bogotá Campus - Faculty of Medicine - Department of Surgery - Bogotá D.C. - Colombia.
Corresponding author: David Felipe López-Atehortua. Departament of Surgery, Faculty of Medicine, Universidad Nacional de Colombia. Carrera 30 No 45-03, building 471, office 107. Phone number: +57 1 316500, ext.: 15031; Mobile number: +57 3113389109. Bogotá D.C. Colombia. Email: daflopezat@unal.edu.co.
| Abstract |
Introduction: Due to the invention of minimally invasive surgery, inguinal hernia repair by laparoscopy has become a common procedure. This paper presents the results of 92 inguinal hernia repairs by laparoscopy performed using the transabdominal pre-peritoneal technique (TAPP) between August 2001 and January 2014.
Objective: To present our results regarding recurrence rate, postoperative pain and need for conversion.
Materials and methods: The results of the procedure using TAPP were retrospectively analyzed based on an average follow-up time of 8 years.
Results: Three (3.2%) cases required conversion, three (3.2%) were recurrent and six (6.4%) presented chronic pain.
Conclusion: Laparoscopic hernia repair by TAPP is a safe procedure. Effectiveness and complication rates have shown to be similar to open and TEP techniques.
Keywords: Hernia; Laparoscopy; Recurrence (MeSH).
Hazbón HR, López-Atehortua DF. Experience and results of laparoscopic inguinal herniorrhaphy. Rev. Fac. Med. 2017;65(3):429-32. English. doi: https://doi.org/10.15446/revfacmed.v65n3.56429.
| Resumen |
Introducción. Con la invención de la cirugía poco invasiva, la herniorrafia inguinal por laparoscopia se ha convertido en un procedimiento de realización frecuente. En el presente artículo se publican los resultados de 92 herniorrafias inguinales por laparoscopia realizadas con técnica transabdominal preperitoneal (TAPP) entre agosto de 2001 y enero de 2014.
Objetivo. Presentar resultados en cuanto a tasa de recurrencia, dolor post-operatorio y necesidad de conversión en las herniorrafias inguinales por laparoscopia analizadas.
Materiales y métodos. Se analizaron de manera retrospectiva los resultados del procedimiento realizando técnica TAPP con seguimiento promedio de 8 años.
Resultados. Se presentaron tres (3.2%) casos que requirieron conversión, tres (3.2%) de recurrencia y seis (6.4%) de dolor crónico.
Conclusión. La herniorrafia por laparoscopia con técnica TAPP es un procedimiento seguro; esta tiene tasas similares de efectividad y complicaciones a la técnica abierta y totalmente extraperitoneal TEP.
Palabras clave: Hernia; Laparoscopia; Recurrencia (DeCS).
David Felipe López-Atehortua. [Experiencia y resultados de la herniorrafia inguinal por laparoscopia] Rev. Fac. Med. 2017;65(3):429-32. English. doi: https://doi.org/10.15446/revfacmed.v65n3.56429.
Introduction
Abdominal wall hernias have been historically reported in human beings. The first reference on this pathology was found in the Ebers papyrus, written in 1560 BC, which defined it as a tumor in the genital area where the intestines move. The history of studies and treatment attempts dates back to the fourth century BC with Hippocrates. In this period, anatomical descriptions were obtained through multiple studies in cadavers, as well as hundreds of fruitless procedures that included skin and herniary sac cuts —despite of not knowing its content—, which could lead to death. Eventually, inguinal sclerosing drugs were implemented (1-5).
The implementation of the laparoscopic procedure began in the 1990s as reported by Ger (6), Schultz (7), Corbitt (8) and Filipi (9). Later, other techniques were developed with excellent results, including the totally extraperitoneal repair (TEP), transabdominal preperitoneal repair (TAPP), internal ring closure, mesh plugs and onlay mesh techniques. The first two techniques use the principle described by Stoppa (10), which states that the mesh is placed in the preperitoneal space.
Endoscopy has been established in the last years as the most preferred technique for the management of inguinal wall defects. This procedure has shown benefits in terms of aesthetics, postoperative pain and size of surgical wounds (11-13). In terms of costs, TEP approach is cheaper than TAPP. However, both are more expensive than open surgery in relation to direct costs, but have equivalent social costs, since social productivity is better in laparoscopic approaches because patients resume their activities faster (12). TAPP technique is performed by placing three laparoscopy trocars on the umbilical area (10mm) and on each flank (5mm). The pneumoperitoneum with carbon dioxide is achieved by inserting a Veress needle at the Palmer’s point, and increasing intra-abdominal pressure up to 12 mmHg. After obtaining adequate pressure, the umbilical port is located to insert the optic, and a 5mm trocar is positioned under direct vision on each flank to avoid injuries in abdominal organs.
Then, once the reference points of the inguinal region have been identified, a horizontal cut in the anterior parietal peritoneum is made about 2cm above the anterior superior iliac spine until the medial umbilical ligament. Such cut is made underneath the ipsilateral side of the hernia. The next step is to dissect the preperitoneal space by sectioning the areolar tissue with a hyfrecator or scissors. Then, the dissection of the medial part is initiated until visualizing an adequate dissection of the Retzius space and the pubic symphysis, so that the pectineum or Cooper’s ligament can be observed. This procedure is done laterally, visualizing the inferior gonadal and epigastric vessels. The preperitoneal is exposed until about 3cm lateral to the anterior superior iliac spine.
The hernia sac is then identified and released from the cord elements using traction-countertraction maneuvers until they are properly reduced. Afterwards, through the umbilical trocar, a 15x12cm low density polypropylene mesh is inserted into the preperitoneal space. The cover mesh is extended near the lateral half of the Retzius space, attached to a Cooper’s ligament with a titanium fastener. The lateral extension is continued until adequately covering the inguinal region, and the mesh is fixed to the lateral side of the abdominal wall avoiding the vascular triangle and pain in the posterior face of the anterior and lateral rectus muscle of the transverse muscle fibers. Finally, after achieving adequate extension, the preperitoneal space is closed with continuous suture in the parietal peritoneum using a 2-0 gauge polyglactin (14-16).
This study reports the experience gained by the authors while managing 92 cases of inguinal herniorrhaphy by laparoscopy using the TAPP technique from August 2001 to January 2014. Data were obtained retrospectively based on a follow-up period between 8 and 120 months
Materials and methods
Inguinal hernia diagnosis was given by a physician specialist in general surgery based on clinical findings. No diagnostic images were taken. The laparoscopic technique used in all patients was inguinal herniorrhaphy via transabdominal preperitoneal pathway. The study was carried out on men and women of legal age who presented with both primary and recurrent inguinal hernia, as well as unilateral or bilateral hernias.
The clinical records of patients who underwent laparoscopic inguinal herniorrhaphy between August 2001 and January 2014 were retrospectively reviewed. The studied clinical outcomes included complications such as postoperative pain (defined as persistent pain for more than 2 months), need for conversion to open surgery and hernia recurrence. The follow-up was personally performed by a general surgeon during the first month, and then by telephone with an average of 2 956 days of follow-up.
Results
Laparoscopic inguinal herniorrhaphy was performed in 100 patients, out of which 92 were successfully monitored after the intervention (Table 1). In the unilateral group, the most common type of primary hernia was indirect (58.2%), while all the hernias in the bilateral group all were direct/direct (57.2%). In the reproduced unilateral group, the most frequent type was indirect (50%) (Table 2).
Table 1. Characteristics of patients.
|
Total sample |
n=92 (100%) |
|
Male |
70 (76%) |
|
Female |
22 (24%) |
|
Age in years at the time of the procedure (mean ± SD) |
51.15±16.05 |
|
Primary |
81 (88.04%) |
|
Reproduced |
11 (11.96%) |
|
Unilateral |
77 (83.7%) |
|
Bilateral |
15 (16.3%) |
|
Comorbidities |
29 (31.5%) |
|
Hypertension |
11 (11.9%) |
|
Diabetes mellitus |
2 (2.2%) |
|
COPD |
2 (2.2%) |
Source: Own elaboration based on the data obtained in the study.
Table 2. Classification of inguinal hernias.
|
Primary (%) |
|
|
Unilateral (%) |
Unilateral (%) |
|
• Indirect: 39 (58.2%) • Direct: 19 (28.3%) • Indirect and femoral: 6 (9%) • Pantaloon: 3 (4.5%) |
• Direct/direct: 8 (57.2%) • Indirect/indirect: 5 (35.7%) • Direct/femoral: 1 (7.1%) |
|
Reproduced (%) |
|
|
Unilateral (%) |
Bilateral (%) |
|
• Indirect: 5 (50%) • Direct: 2 (20%) • Combined: 2 (20%) • Femoral: 1 (10%) |
• Indirect/indirect: 1 (100%) |
Source: Own elaboration based on the data obtained in the study.
The operating time of primary unilateral inguinal herniorrhaphy, excluding patients requiring conversion, was 39.9±19.5 minutes. For the primary bilateral group, time was estimated at 67.27±26.6 minutes, and in the unilateral reproductive group at 46.5±25.4 minutes (Figure 1). Regarding hospital stay, 87 (94.5%) procedures were outpatient, 4 (4.3%) patients required hospitalization for one day, and 1 (1.1%) patient required hospitalization for three days. The latter patient underwent prostatectomy during the same surgery, which required post-operative hospitalization. Furthermore, three conversion (3.2%) cases occurred due to large fibrosis around the hernial sac area.
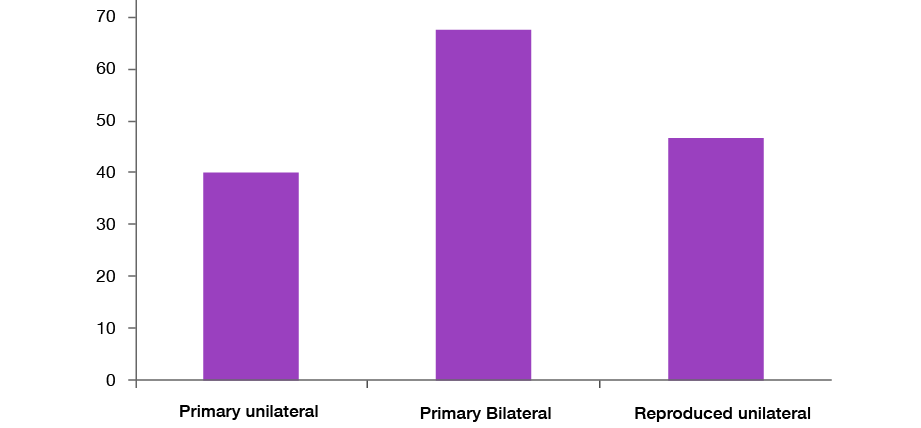
Figure 1. Average operating times among each group expressed in minutes.
Source: Own elaboration based on the data obtained in the study.
Regarding complications, no infection cases of the operative site were observed; 3 (3.2%) cases presented with seroma; 3 (3.2%) developed inguinal hematoma —2 handled with medication and 1 with surgical drainage—; 1 (1.1%) case had epigastric lesions that were controlled by laparoscopy; 3 (3.2%) cases documented hernia recurrence, and 6 (6.4%) cases had post-operative pain for more than 2 months (Table 3).
Table 3. Complications observed during inguinal herniorrhaphy.
|
Type of complication |
n=92 (100%) |
|
Infection |
0 (0%) |
|
Seroma |
3 (3.2%) |
|
Hematoma |
3 (3.2%) |
|
Epigastric vessel injury |
1 (1.1%) |
|
Recurrence |
3 (3.2%) |
|
Postoperative pain |
6 (6.4%) |
|
Conversion |
3 (3.2%) |
Source: Own elaboration based on the data obtained in the study.
Discussion
The first inguinal herniorrhaphy by laparoscopy was described by Ger et al. (17) in 1990, which consisted in covering the defect with a mesh. In 1992, Arregui et al. (18) described the TAPP technique, and in 1993 McKernan et al. (19) presented the TEP technique. In 2010, during the European Association of Endoscopic Surgery Congress, attended by 100 surgeons, it was concluded that the most widely used laparoscopic herniorrhaphy technique is TAPP (20). Unfortunately, no literature was found in Colombia which could be used to compare our results. However, they are good when compared to international studies.
The mean surgical time in this series (39.9 minutes for primary unilateral and 67.27 minutes for primary bilateral) was within the ranges described in larger series (unilateral 25-102 minutes, and bilateral 38-123 minutes) (21,22).
As for early complications, no injuries in intra-abdominal organs were observed, nor conditions that would endanger the life of patients in the short-term. Additionally, no association was found between comorbidities and seroma and hematoma complications. Nevertheless, among the patients that required conversion to open technique, there was a case with a history of Fournier gangrene, which was probably associated with the great adhesion process found intraoperatively around the sac that could not be reduced by the endoscopy.
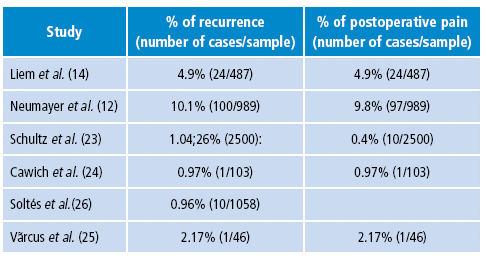
With regard to recurrence, the three cases presented here are among the first 50 studies performed, which may suggest that they are associated with the learning curve. When attempting associations with the chronic pain presented by the six patients who reported it, no data were found within the variables studied. Moreover, the range was within those described in the literature (11,12,23,24,25) (Table 4).
Table 4. Recurrence and postoperative pain.
|
Study |
% of recurrence |
% of postoperative pain (number of cases/sample) |
|
Liem et al. (14) |
4.9% (24/487) |
4.9% (24/487) |
|
Neumayer et al. (12) |
10.1% (100/989) |
9.8% (97/989) |
|
Schultz et al. (23) |
1.04;26% (2500): |
0.4% (10/2500) |
|
Cawich et al. (24) |
0.97% (1/103) |
0.97% (1/103) |
|
Soltés et al.(26) |
0.96% (10/1058) |
|
|
Vãrcus et al. (25) |
2.17% (1/46) |
2.17% (1/46) |
Source: Own elaboration based on the data obtained in the study.
Conclusion
Laparoscopic herniorrhaphy with TAPP technique is considered to be a safe procedure, with a low rate of complications, which can be performed by expert hands in short surgical times with low recurrence rates. In addition, due to the experience and the temporality of recurrence, it could be suggested that the learning curve for performing the procedure is 50 cases under the supervision of an expert.
Conflict of interest
None stated by the authors.
Funding
None stated by the authors.
Acknowledgement
None stated by the authors.
References
1.Rutkow IM. A selective history of groin hernia surgery in the early 19th century. The anatomic atlases of Astley Cooper, Franz Hesselbach, Antonio Scarpa, and Jules-Germain Cloquet. Surg Clin North Am. 1998;78(6):921-40. http://doi.org/fc8r3h.
2.Rutkow IM. The PerFix plug repair for groin hernias. Surg Clin North Am. 2003;83(5):1079-98. http://doi.org/cv7gpd.
3.Rutkow IM. Demographic, and socioeconomic aspects of hernia repair in the United States in 2003. Surg Clin North Am. 2003;83(5):1045-51. http://doi.org/b2s4ck.
4.Rutkow IM. A selective history of hernia surgery in the late eighteenth century: the treatises of Percivall Pott, Jean Louis Petit, D. August Gottlieb Richter, Don Antonio de Gimbernat, and Pieter. Surg Clin North Am. 2003;83(5):1021-44. http://doi.org/c6zzg8.
5.Carbonell-Tatay F. Hernia inguinocrural. Valencia: Ethicon; 2001.
6.Ger R. The laparoscopic management of groin hernias. Contemp Surg. 1991;39(4):15-9.
7.Schultz L, Graber J, Pietrafitta J, Hickok D. Laser laparoscopic herniorrhaphy: a clinical trial, preliminary results. J Laparoendosc Surg. 1990;1(1):41-5. http://doi.org/dsd3fz.
8.Corbitt JD Jr. Laparoscopic herniorrhaphy. Surg Laparosc Endosc. 1991;1(1):23-5.
9.Filipi CJ, Fitzgibbons RJ Jr, Salerno GM, Hart RO. Laparoscopic herniorrhaphy. Surg Clin North Am. 1992;72(5):1109-24. http://doi.org/b6r2.
10.Stoppa RE. The treatment of complicated groin and incisional hernias. World J Surg. 1989;13(5):545-54. http://doi.org/bvcbdv.
11.Liem MS, van der Graaf Y, van Steensel CJ, Boelhouwer RU, Clevers GJ, Meijer WS, et al. Comparison of conventional anterior surgery and laparoscopic surgery for inguinal hernia repair. N Engl J Med. 1997;336(22):1541-7.
12.Neumayer L, Giobbie-Hurder A, Jonasson O, Fitzgibbons R Jr, Dunlop D, Gibbs J, et al. Open mesh versus laparoscopic mesh repair of inguinal hernia. N Engl J Med. 2004;350(18):1819-27. http://doi.org/cbp5v3.
13.Eklund A, Rudberg C, Smedberg S, Enander LK, Leijonmarck CE, Osterberg J, et al. Short-term results of a randomized clinical trial comparing Lichtenstein open repair with totally extraperitoneal laparoscopic inguinal hernia repair. Br J Surg. 2006;93:1060-8. http://doi.org/ddmssd.
14.Liem MS, van Duyn EB, van der Graaf Y, van Vroonhoven TJ. Recurrences After Conventional Anterior and Laparoscopic Inguinal Hernia Repair: A Randomized Comparison. Ann Surg. 2003;237(1):136-41.
15.Hussain A, Nicholls J, El-Hasani S. Technical Tips Following More Than 2000 Transabdominal Preperitoneal (TAPP) Repair of the Groin Hernia. Surg Laparosc Endosc Percutan Tech. 2010;20(6):384-8. http://doi.org/b9sfxr.
16.Moldovanu R, Pavy G. Laparoscopic Transabdominal Pre-Peritoneal (TAPP) Procedure - Step-by-Step Tips and Tricks. Chirurgia. 2014;109(3):407-15.
17.Ger R, Monroe K, Duvivier R, Mishrick A. Management of indirect inguinal hernias by laparoscopic closure of the neck of the sac. Am J Surg. 1990;159(4):370 3. http://doi.org/cv8v5b.
18.Arregui ME, Davis CJ, Yucel O, Nagan RF. Laparoscopic mesh repair of inguinal hernia using a pre peritoneal approach: A preliminary report. Surg Laparosc Endosc. 1992;2(1):53 8.
19.McKernan JB, Laws HL. Laparoscopic repair of inguinal hernias using a totally extraperitoneal prosthetic approach. Surg Endosc. 1993;7(1):26-8. http://doi.org/fmqvjw.
20.Morales Conde S, Socas M, Fingerhut A. Endoscopic surgeons preferences for inguinal hernia repair: TEP, TAPP, or OPEN. Surg Endosc. 2012(26):2639 43. http://doi.org/f37tzj.
21.Ridings P, Evans DS. The transabdominal pre peritoneal (TAPP) inguinal hernia repair: A trip along the learning curve. J R Coll Surg Edinb. 2000;45(1):29 32.
22.Tatulli F, Chetta G, Caputi A, Mastrototaro P, Ruggieri T. Laparoscopic inguinal hernia repair: Audit of our experience with laparoscopic trans abdominal pro peritoneal repair (TAPP). Chir Ital. 2009;61(1):47 53.
23.Schultz I, Baca I, Götzen V. Laparoscopic inguinal hernia repair. Surg Endosc. 2001;15:582-84. http://doi.org/d8fv6d.
24.Cawich SO, Mohanty SK, Bonadie KO, Simpson LK, Johnson PB, Shan S, et al. Laparoscopic Inguinal Hernia Repair in a Developing Nation: Short term Outcomes in 103 Consecutive Procedures. J Surg Tech Case Rep. 2013;5(1):13-7. http://doi.org/b6r5.
25.Vãrcuş F, Dutã C, Dobrescu A, Lazãr F, Papurica M, Tarta C. Laparoscopic Repair of Inguinal Hernia TEP versus TAPP. Chirurgia. 2016;111(4):308-12.
26.Soltés M, Pazinka P, Ranodak J. [Laparoscopic hernioplasty TAPP in treatment of groin hernia – 10 years experience]. Rozhl Chir. 2010;89(6):384-9.
Recibido: 24 de marzo de 2016; Aceptado: 19 de junio de 2016
Abstract
Introduction:
Due to the invention of minimally invasive surgery, inguinal hernia repair by laparoscopy has become a common procedure. This paper presents the results of 92 inguinal hernia repairs by laparoscopy performed using the transabdominal pre-peritoneal technique (TAPP) between August 2001 and January 2014.
Objective:
To present our results regarding recurrence rate, postoperative pain and need for conversion.
Materials and methods:
The results of the procedure using TAPP were retrospectively analyzed based on an average follow-up time of 8 years.
Results:
Three (3.2%) cases required conversion, three (3.2%) were recurrent and six (6.4%) presented chronic pain.
Conclusion:
Laparoscopic hernia repair by TAPP is a safe procedure. Effectiveness and complication rates have shown to be similar to open and TEP techniques.
Keywords:
Hernia, Laparoscopy, Recurrence (MeSH).Resumen
Introducción.
Con la invención de la cirugía poco invasiva, la herniorrafia inguinal por laparoscopia se ha convertido en un procedimiento de realización frecuente. En el presente artículo se publican los resultados de 92 herniorrafias inguinales por laparoscopia realizadas con técnica transabdominal preperitoneal (TAPP) entre agosto de 2001 y enero de 2014.
Objetivo.
Presentar resultados en cuanto a tasa de recurrencia, dolor post-operatorio y necesidad de conversión en las herniorrafias inguinales por laparoscopia analizadas.
Materiales y métodos.
Se analizaron de manera retrospectiva los resultados del procedimiento realizando técnica TAPP con seguimiento promedio de 8 años.
Resultados.
Se presentaron tres (3.2%) casos que requirieron conversión, tres (3.2%) de recurrencia y seis (6.4%) de dolor crónico.
Conclusión.
La herniorrafia por laparoscopia con técnica TAPP es un procedimiento seguro; esta tiene tasas similares de efectividad y complicaciones a la técnica abierta y totalmente extraperitoneal TEP.
Palabras clave:
Hernia, Laparoscopia, Recurrencia (DeCS).Introduction
Abdominal wall hernias have been historically reported in human beings. The first reference on this pathology was found in the Ebers papyrus, written in 1560 BC, which defined it as a tumor in the genital area where the intestines move. The history of studies and treatment attempts dates back to the fourth century BC with Hippocrates. In this period, anatomical descriptions were obtained through multiple studies in cadavers, as well as hundreds of fruitless procedures that included skin and herniary sac cuts -despite of not knowing its content-, which could lead to death. Eventually, inguinal sclerosing drugs were implemented 1-5.
The implementation of the laparoscopic procedure began in the 1990s as reported by Ger 6, Schultz 7, Corbitt 8 and Filipi 9. Later, other techniques were developed with excellent results, including the totally extraperitoneal repair (TEP), transabdominal preperitoneal repair (TAPP), internal ring closure, mesh plugs and onlay mesh techniques. The first two techniques use the principle described by Stoppa 10, which states that the mesh is placed in the preperitoneal space.
Endoscopy has been established in the last years as the most preferred technique for the management of inguinal wall defects. This procedure has shown benefits in terms of aesthetics, postoperative pain and size of surgical wounds 11-13. In terms of costs, TEP approach is cheaper than TAPP. However, both are more expensive than open surgery in relation to direct costs, but have equivalent social costs, since social productivity is better in laparoscopic approaches because patients resume their activities faster 12. TAPP technique is performed by placing three laparoscopy trocars on the umbilical area (10mm) and on each flank (5mm). The pneumoperitoneum with carbon dioxide is achieved by inserting a Veress needle at the Palmer's point, and increasing intra-abdominal pressure up to 12 mmHg. After obtaining adequate pressure, the umbilical port is located to insert the optic, and a 5mm trocar is positioned under direct vision on each flank to avoid injuries in abdominal organs.
Then, once the reference points of the inguinal region have been identified, a horizontal cut in the anterior parietal peritoneum is made about 2cm above the anterior superior iliac spine until the medial umbilical ligament. Such cut is made underneath the ipsilateral side of the hernia. The next step is to dissect the preperitoneal space by sectioning the areolar tissue with a hyfrecator or scissors. Then, the dissection of the medial part is initiated until visualizing an adequate dissection of the Retzius space and the pubic symphysis, so that the pectineum or Cooper's ligament can be observed. This procedure is done laterally, visualizing the inferior gonadal and epigastric vessels. The preperitoneal is exposed until about 3cm lateral to the anterior superior iliac spine.
The hernia sac is then identified and released from the cord elements using traction-countertraction maneuvers until they are properly reduced. Afterwards, through the umbilical trocar, a 15x12cm low density polypropylene mesh is inserted into the preperitoneal space. The cover mesh is extended near the lateral half of the Retzius space, attached to a Cooper's ligament with a titanium fastener. The lateral extension is continued until adequately covering the inguinal region, and the mesh is fixed to the lateral side of the abdominal wall avoiding the vascular triangle and pain in the posterior face of the anterior and lateral rectus muscle of the transverse muscle fibers. Finally, after achieving adequate extension, the preperitoneal space is closed with continuous suture in the parietal peritoneum using a 2-0 gauge polyglactin 14-16.
This study reports the experience gained by the authors while managing 92 cases of inguinal herniorrhaphy by laparoscopy using the TAPP technique from August 2001 to January 2014. Data were obtained retrospectively based on a follow-up period between 8 and 120 months
Materials and methods
Inguinal hernia diagnosis was given by a physician specialist in general surgery based on clinical findings. No diagnostic images were taken. The laparoscopic technique used in all patients was inguinal herniorrhaphy via transabdominal preperitoneal pathway. The study was carried out on men and women of legal age who presented with both primary and recurrent inguinal hernia, as well as unilateral or bilateral hernias.
The clinical records of patients who underwent laparoscopic inguinal herniorrhaphy between August 2001 and January 2014 were retrospectively reviewed. The studied clinical outcomes included complications such as postoperative pain (defined as persistent pain for more than 2 months), need for conversion to open surgery and hernia recurrence. The follow-up was personally performed by a general surgeon during the first month, and then by telephone with an average of 2 956 days of follow-up.
Results
Laparoscopic inguinal herniorrhaphy was performed in 100 patients, out of which 92 were successfully monitored after the intervention (Table 1). In the unilateral group, the most common type of primary hernia was indirect (58.2%), while all the hernias in the bilateral group all were direct/direct (57.2%). In the reproduced unilateral group, the most frequent type was indirect (50%) (Table 2).
Source: Own elaboration based on the data obtained in the study.Table 1: Characteristics of patients.

Source: Own elaboration based on the data obtained in the study.Table 2: Classification of inguinal hernias.

The operating time of primary unilateral inguinal herniorrhaphy, excluding patients requiring conversion, was 39.9±19.5 minutes. For the primary bilateral group, time was estimated at 67.27±26.6 minutes, and in the unilateral reproductive group at 46.5±25.4 minutes (Figure 1). Regarding hospital stay, 87 (94.5%) procedures were outpatient, 4 (4.3%) patients required hospitalization for one day, and 1 (1.1%) patient required hospitalization for three days. The latter patient underwent prostatectomy during the same surgery, which required post-operative hospitalization. Furthermore, three conversion (3.2%) cases occurred due to large fibrosis around the hernial sac area.
Figure 1: Average operating times among each group expressed in minutes. Source: Own elaboration based on the data obtained in the study.
Regarding complications, no infection cases of the operative site were observed; 3 (3.2%) cases presented with seroma; 3 (3.2%) developed inguinal hematoma -2 handled with medication and 1 with surgical drainage-; 1 (1.1%) case had epigastric lesions that were controlled by laparoscopy; 3 (3.2%) cases documented hernia recurrence, and 6 (6.4%) cases had post-operative pain for more than 2 months (Table 3).
Source: Own elaboration based on the data obtained in the study.Table 3: Complications observed during inguinal herniorrhaphy.

Discussion
The first inguinal herniorrhaphy by laparoscopy was described by Ger et al. 17 in 1990, which consisted in covering the defect with a mesh. In 1992, Arregui et al. 18 described the TAPP technique, and in 1993 McKernan et al. 19 presented the TEP technique. In 2010, during the European Association of Endoscopic Surgery Congress, attended by 100 surgeons, it was concluded that the most widely used laparoscopic herniorrhaphy technique is TAPP 20. Unfortunately, no literature was found in Colombia which could be used to compare our results. However, they are good when compared to international studies.
The mean surgical time in this series (39.9 minutes for primary unilateral and 67.27 minutes for primary bilateral) was within the ranges described in larger series (unilateral 25-102 minutes, and bilateral 38-123 minutes) 21,22.
As for early complications, no injuries in intra-abdominal organs were observed, nor conditions that would endanger the life of patients in the short-term. Additionally, no association was found between comorbidities and seroma and hematoma complications. Nevertheless, among the patients that required conversion to open technique, there was a case with a history of Fournier gangrene, which was probably associated with the great adhesion process found intraoperatively around the sac that could not be reduced by the endoscopy.
With regard to recurrence, the three cases presented here are among the first 50 studies performed, which may suggest that they are associated with the learning curve. When attempting associations with the chronic pain presented by the six patients who reported it, no data were found within the variables studied. Moreover, the range was within those described in the literature 11,12,23,24,25 (Table 4).
Source: Own elaboration based on the data obtained in the study.Table 4: Recurrence and postoperative pain.
Conclusion
Laparoscopic herniorrhaphy with TAPP technique is considered to be a safe procedure, with a low rate of complications, which can be performed by expert hands in short surgical times with low recurrence rates. In addition, due to the experience and the temporality of recurrence, it could be suggested that the learning curve for performing the procedure is 50 cases under the supervision of an expert.
Acknowledgement
None stated by the authors.
References
Referencias
Rutkow IM. A selective history of groin hernia surgery in the early 19th century. The anatomic atlases of Astley Cooper, Franz Hesselbach, Antonio Scarpa, and Jules-Germain Cloquet. Surg Clin North Am. 1998;78(6):921-40. http://doi.org/fc8r3h.
Rutkow IM. The PerFix plug repair for groin hernias. Surg Clin North Am. 2003;83(5):1079-98. http://doi.org/cv7gpd.
Rutkow IM. Demographic, and socioeconomic aspects of hernia repair in the United States in 2003. Surg Clin North Am. 2003;83(5):1045-51. http://doi.org/b2s4ck.
Rutkow IM. A selective history of hernia surgery in the late eighteenth century: the treatises of Percivall Pott, Jean Louis Petit, D. August Gottlieb Richter, Don Antonio de Gimbernat, and Pieter. Surg Clin North Am. 2003;83(5):1021-44. http://doi.org/c6zzg8.
Carbonell-Tatay F. Hernia inguinocrural. Valencia: Ethicon; 2001.
Ger R. The laparoscopic management of groin hernias. Contemp Surg. 1991;39(4):15-9.
Schultz L, Graber J, Pietrafitta J, Hickok D. Laser laparoscopic herniorrhaphy: a clinical trial, preliminary results. J Laparoendosc Surg. 1990;1(1):41-5. http://doi.org/dsd3fz.
Corbitt JD Jr. Laparoscopic herniorrhaphy. Surg Laparosc Endosc. 1991;1(1):23-5.
Filipi CJ, Fitzgibbons RJ Jr, Salerno GM, Hart RO. Laparoscopic herniorrhaphy. Surg Clin North Am. 1992;72(5):1109-24. http://doi.org/b6r2.
Stoppa RE. The treatment of complicated groin and incisional hernias. World J Surg. 1989;13(5):545-54. http://doi.org/bvcbdv.
Liem MS, van der Graaf Y, van Steensel CJ, Boelhouwer RU, Clevers GJ, Meijer WS, et al. Comparison of conventional anterior surgery and laparoscopic surgery for inguinal hernia repair. N Engl J Med. 1997;336(22):1541-7.
Neumayer L, Giobbie-Hurder A, Jonasson O, Fitzgibbons R Jr, Dunlop D, Gibbs J, et al. Open mesh versus laparoscopic mesh repair of inguinal hernia. N Engl J Med. 2004;350(18):1819-27. http://doi.org/cbp5v3.
Eklund A, Rudberg C, Smedberg S, Enander LK, Leijonmarck CE, Osterberg J, et al. Short-term results of a randomized clinical trial comparing Lichtenstein open repair with totally extraperitoneal laparoscopic inguinal hernia repair. Br J Surg. 2006;93:1060-8. http://doi.org/ddmssd.
Liem MS, van Duyn EB, van der Graaf Y, van Vroonhoven TJ. Recurrences After Conventional Anterior and Laparoscopic Inguinal Hernia Repair: A Randomized Comparison. Ann Surg. 2003;237(1):136-41.
Hussain A, Nicholls J, El-Hasani S. Technical Tips Following More Than 2000 Transabdominal Preperitoneal (TAPP) Repair of the Groin Hernia. Surg Laparosc Endosc Percutan Tech. 2010;20(6):384-8. http://doi.org/b9sfxr.
Moldovanu R, Pavy G. Laparoscopic Transabdominal Pre-Peritoneal (TAPP) Procedure - Step-by-Step Tips and Tricks. Chirurgia. 2014;109(3):407-15.
Ger R, Monroe K, Duvivier R, Mishrick A. Management of indirect inguinal hernias by laparoscopic closure of the neck of the sac. Am J Surg. 1990;159(4):370 3. http://doi.org/cv8v5b.
Arregui ME, Davis CJ, Yucel O, Nagan RF. Laparoscopic mesh repair of inguinal hernia using a pre peritoneal approach: A preliminary report. Surg Laparosc Endosc. 1992;2(1):53 8.
McKernan JB, Laws HL. Laparoscopic repair of inguinal hernias using a totally extraperitoneal prosthetic approach. Surg Endosc. 1993;7(1):26-8. http://doi.org/fmqvjw.
Morales Conde S, Socas M, Fingerhut A. Endoscopic surgeons preferences for inguinal hernia repair: TEP, TAPP, or OPEN. Surg Endosc. 2012(26):2639 43. http://doi.org/f37tzj.
Ridings P, Evans DS. The transabdominal pre peritoneal (TAPP) inguinal hernia repair: A trip along the learning curve. J R Coll Surg Edinb. 2000;45(1):29 32.
Tatulli F, Chetta G, Caputi A, Mastrototaro P, Ruggieri T. Laparoscopic inguinal hernia repair: Audit of our experience with laparoscopic trans abdominal pro peritoneal repair (TAPP). Chir Ital. 2009;61(1):47 53.
Schultz I, Baca I, Götzen V. Laparoscopic inguinal hernia repair. Surg Endosc. 2001;15:582-84. http://doi.org/d8fv6d.
Cawich SO, Mohanty SK, Bonadie KO, Simpson LK, Johnson PB, Shan S, et al. Laparoscopic Inguinal Hernia Repair in a Developing Nation: Short term Outcomes in 103 Consecutive Procedures. J Surg Tech Case Rep. 2013;5(1):13-7. http://doi.org/b6r5.
Vãrcuş F, Dutã C, Dobrescu A, Lazãr F, Papurica M, Tarta C. Laparoscopic Repair of Inguinal Hernia TEP versus TAPP. Chirurgia. 2016;111(4):308-12.
Soltés M, Pazinka P, Ranodak J. [Laparoscopic hernioplasty TAPP in treatment of groin hernia – 10 years experience]. Rozhl Chir. 2010;89(6):384-9.
Cómo citar
APA
ACM
ACS
ABNT
Chicago
Harvard
IEEE
MLA
Turabian
Vancouver
Descargar cita
CrossRef Cited-by
1. Samir Quejada Cuesta, Simón Muñoz-González, Melany Andrea Ramírez-Salazar, Santiago Castro-Carmona, María Clara Mendoza-Arango, Johan Sebastián Herrera-Vargas, Juan David Martínez-Maya. (2026). Caracterización de la población sometida a herniorrafia inguinal laparoscópica en centros de alta complejidad en el Departamento de Antioquia. Revista Colombiana de Cirugía, https://doi.org/10.30944/20117582.3012.
Dimensions
PlumX
Visitas a la página del resumen del artículo
Descargas
Licencia
Derechos de autor 2017 Revista de la Facultad de Medicina

Esta obra está bajo una licencia Creative Commons Reconocimiento 3.0 Unported.
-