Bilateral testicular pain as an acute aortic dissection symptom
Dolor testicular bilateral como presentación de disección aórtica aguda
DOI:
https://doi.org/10.15446/revfacmed.v64n3.53257Palabras clave:
Aortic Diseases, Dissection, Acute Pain, Referred Pain, Chest Pain, Testis (en)Enfermedades aórticas, Disección, Dolor agudo, Dolor referido, Dolor en el pecho, Testículo (es)
Descargas
Acute aortic dissection is a serious cardiovascular event and the most common acute disease of the great vessels. According to the anatomical distribution of the compromised aorta, the Stanford Group classifies it into type A and type B. Its prognosis depends on its early identification and treatment, as the mortality rate in type A increases rapidly with each hour of delay of diagnosis.
Clinical manifestations of aortic dissection may be varied, which makes its early diagnosis difficult. Regarding its diagnosis, genital pain is one of the rarest symptoms. In this paper, the case of a patient who initially attended a health care institution due to acute bilateral testicular pain and was eventually diagnosed with acute aortic dissection is presented.
La disección aórtica aguda es un evento cardiovascular catastrófico que corresponde a la más común de las enfermedades agudas de los grandes vasos. Según la distribución anatómica de la aorta comprometida, el grupo de Stanford la clasifica en dos tipos: A y B. Su pronóstico depende de la identificación y manejo tempranos, siendo la tasa de mortalidad rápidamente creciente en el tipo A con cada hora que se retrasa el diagnóstico.
Las manifestaciones clínicas de la disección aórtica pueden ser múltiples, lo que dificulta su diagnóstico precoz. Dentro de las formas de presentación, una de las más infrecuentes es el dolor en los genitales. Se presenta el caso clínico de un paciente que consulta inicialmente por un dolor agudo testicular bilateral y que finalmente es diagnosticado con disección aórtica aguda.
case report
DOI: https://doi.org/10.15446/revfacmed.v64n3.53257
Bilateral testicular pain as an acute aortic dissection symptom
Dolor testicular bilateral como presentación de disección aórtica aguda
Received: 10/10/2015. Accepted: 24/01/2016.
Gloria Mercedes Guarín-Loaiza¹ • Laura Cristina Nocua-Báez1 • Gladys Alfonso-Hernández1
1 Universidad Nacional de Colombia - Bogotá Campus - Faculty of Medicine - Department of Internal Medicine - Bogotá, D.C. - Colombia.
Corresponding author: Gloria Mercedes-Loaiza Guarín. Department of Internal Medicine, Faculty of Medicine, Universidad Nacional de Colombia. Carrera 30 No. 45-03, building 471, office 510. Phone number: +57 1 3165000, ext.: 15011; mobile phone: + 57 3123815771. Bogotá, D.C. Colombia. Email: gmguarinlo@unal.edu.co.
| Abstract |
Acute aortic dissection is a serious cardiovascular event and the most common acute disease of the great vessels. According to the anatomical distribution of the compromised aorta, the Stanford Group classifies it into type A and type B. Its prognosis depends on its early identification and treatment, as the mortality rate in type A increases rapidly with each hour of delay of diagnosis.
Clinical manifestations of aortic dissection may be varied, which makes its early diagnosis difficult. Regarding its diagnosis, genital pain is one of the rarest symptoms. In this paper, the case of a patient who initially attended a health care institution due to acute bilateral testicular pain and was eventually diagnosed with acute aortic dissection is presented.
Keywords: Aortic Diseases; Dissection; Acute Pain; Referred Pain; Chest Pain; Testis (MeSH).
Guarín-Loaiza GM, Nocua-Baez LC, Alfonso-Hernández G. Bilateral testicular pain as an acute aortic dissection symptom. Rev. Fac. Med. 2016;64(3):571-4. English. doi: https://doi.org/10.15446/revfacmed.v64n3.53257.
| Resumen |
La disección aórtica aguda es un evento cardiovascular catastrófico que corresponde a la más común de las enfermedades agudas de los grandes vasos. Según la distribución anatómica de la aorta comprometida, el grupo de Stanford la clasifica en dos tipos: A y B. Su pronóstico depende de la identificación y manejo tempranos, siendo la tasa de mortalidad rápidamente creciente en el tipo A con cada hora que se retrasa el diagnóstico.
Las manifestaciones clínicas de la disección aórtica pueden ser múltiples, lo que dificulta su diagnóstico precoz. Dentro de las formas de presentación, una de las más infrecuentes es el dolor en los genitales. Se presenta el caso clínico de un paciente que consulta inicialmente por un dolor agudo testicular bilateral y que finalmente es diagnosticado con disección aórtica aguda.
Palabras clave: Enfermedades aórticas; Disección; Dolor agudo; Dolor referido; Dolor en el pecho; Testículo (DeCS).
Guarín-Loaiza GM, Nocua-Baez LC, Alfonso-Hernández G. [Dolor testicular bilateral como presentación de disección aórtica aguda]. Rev. Fac. Med. 2016;64(3):571-4. English. doi:
https://doi.org/10.15446/revfacmed.v64n3.53257.
Introduction
Acute aortic dissection (AAD) is part of the acute aortic syndrome and is defined as an emergency condition involving the aorta, which can lead to rupture of the carotid intima and media (1). AAD occurs when an ulcer or a tear in the arterial intimal layer allows passage of blood and the appearance of a false light between this and the middle or muscular layer of the vessel (1); this break spreads and causes a catastrophic event, which corresponds to the most common acute diseases of large vessels.
This syndrome was described for the first time by Laennec in 1826 (2). In autopsy studies, a prevalence of 0.2% to 0.8% was determined, and in population works, an incidence of 0.5 to 4 cases per 100 000 inhabitants per year (3) is estimated. The most important risk factors include age, male gender —male: female ratio 2:1 to 5:1 according to the series— (3), poorly controlled hypertension (HTA) in 65-75% of patients and pre-existing aortic disease (1).
Different classifications of aortic dissection have been described; the Stanford group is currently used and describes two types: A, which corresponds to the originated in the ascending aorta and is extended at least to the aortic arch, and B, which begins in the descending aorta and usually is distal to the left subclavian artery (1).
The typical clinical manifestation of the disease is chest pain, heart failure, syncope, shock, paraplegia and even mesenteric commitment with bleeding in the gastrointestinal tract (4).
The AAD prognosis is bleak in the context of late identification and management, with the mortality rate as high as 1% per hour (1).
This study presents an AAD case with an atypical manifestation of the disease, corresponding to type B according to the Stanford group.
Case presentation
The case of a 49-year-old male, who consulted a second-level hospital due to a clinical picture of sudden bilateral testicular pain of 30 minutes of evolution, which began after trying to stand after being in squatting position, did not improve with rest, irradiated to the lumbar region and prevented supine position. The intensity was rated 10/10 in the analog pain scale. 15 minutes after the patient had moderate intensity oppressive retrosternal chest pain with marked and intermittent 3/10 diaphoresis; there was persistence of severe back pain.
Medical history showed a patient with hypertension diagnosed eight years before, with poor adherence to treatment, obstructive sleep apnea hypopnea syndrome (OSAHS) which made the use of supplemental oxygen necessary, and morbid obesity with BMI of 35 kg/m2. In the review of systems, the patient was classified as class III in the New York Heart Association (NYHA) Functional classification scale and reported an episode of hematuria 15 days before admission.
Physical examination found an obese, alert, algic, diaphoretic patient, with high blood pressure, tachycardia and low oxygen saturation corrected by nasal cannula suplencia, and grade II jugular venous distention at 45 degrees. Cardiopulmonary, abdominal, urinary and genital examination had no apparent abnormalities. The pressure values of all four limbs were abnormal with marked decrease in the right leg, greater than 20 mmHg compared to the left leg. Table 1 summarizes the findings in the patient’s vital signs.
Table 1. Patient’s vital signs at the time of initial assessment.
|
Vital signs |
- |
Right upper limb |
Left upper limb |
Right lower limb |
Left lower limb |
|
BP Average initial BP |
- |
250/150 183 |
- - |
- - |
- - |
|
BP after labetalol |
- - |
186/102 130 |
182/102 128.6 |
170/110 130 |
198/114 142 |
|
Heart rate beats/minute |
100 |
- |
- |
- |
- |
|
Respiratory rate breaths/minute |
20 |
- |
- |
- |
- |
|
Saturation with FiO2 0.24 |
92% |
- |
- |
- |
- |
BP: blood pressure. Source: Own elaboration based on the data obtained in the study.
Paraclinical examinations showed polycythemia, positive troponin, microscopic hematuria, impaired renal function, arterial blood gases with chronic respiratory acidosis and moderate oxygenation disorder, electrocardiogram axis shifted to the right and signs of overload of the right ventricle with dynamic changes in the T wave in leads V4-V5. Chest radiography was performed with cardiomegaly at the expense of the right cavities and pre-capillary pulmonary hypertension without mediastinal widening.
Hypertensive emergency was considered with aorta or heart target organs, probable acute myocardial infarction (AMI) without ST-segment elevation, and electrocardiographic findings related to the axis and ventricular overload were correlated with his OSAHS history. Treatment was started with intravenous labetalol to control blood pressure and heart rate, pain was managed with opioids, oxygen therapy was administered through a nasal cannula, among others. A computed tomography (CT), with contrast material, of the chest and abdomen and protocol for the aorta were performed; CT showed AAD with extensive thoracoabdominal flap extending from the aortic arch, in antegrade direction, until the origin of the inferior mesenteric artery (Figure 1, 2 and 3).
Figure 1. CT angiography of the chest. Arrows: extensive aortic dissection with inferiorly dissection flap from the aortic arch along the thoracic aorta. Source: Own elaboration based on the data obtained in the study.

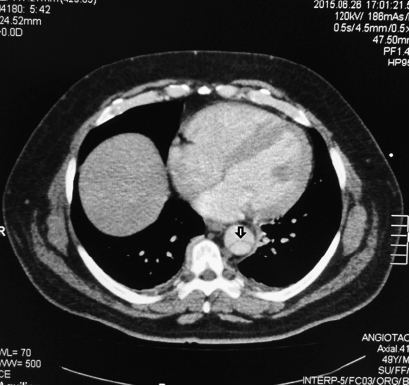
Figure 2. CT angiography of the chest. Arrow: aortic dissection from the middle third of the aortic arch, which is thick and has usual course without aneurysmal dilation inside. Source: Own elaboration based on the data obtained in the study.

Figure 3. CT angiography of the abdomen. Arrow: aortic dissection that involves the abdominal aorta approximately to the origin of the inferior mesenteric artery. Source: Document obtained during the course of the study.
The patient was admitted to the intensive care unit, sent to an institution of higher complexity of care to be assessed by cardiovascular surgery physicians, who considered non-operative management, and discharged him from the institution with medical treatment and strict control of risk factors.
Both the patient and the health institution gave their consent to the publication of this case.
Discussion
AAD is a condition that can occur in clinical practice and is similar to other more common entities such as AMI and pulmonary thromboembolism. Its diagnosis requires high clinical suspicion, especially if, as in this case, there are risk factors such as hypertension, which is found in 75% of patients with this type of aortic dissection (5,6).
Although most patients present with acute and severe abdominal or chest pain, described as a “tearing sensation”, this pain may spread to the back, gluteus, groin, legs, or lumbar region (1,5); in despite of this being the most common characteristic (7,8), some patients may be asymptomatic: chest pain may be absent in 10-33% of cases (1,4).
The first symptom of the evaluated patient was bilateral testicular pain as the predominant symptom. The patient was a young man with a rare age for infra-diaphragmatic or abdominal AAD, which, added to the previous history of hematuria (confirmed through urinalysis), raised the suspicion of urolithiasis. Given the coexistence of chest pain, persistent severe back pain and high blood pressure, with great difference in data between the legs, AAD diagnosis was suspected.
The presentation of hypertension in the emergency department can be found in 45% of patients (8) and abdominal and back pain have been previously reported as more frequent in patients with type B AAD (1,7,9).
Differential systolic blood pressure higher than 20 mmHg in both arms had been determined as an independent predictor of the presence of acute aortic syndrome, but some recent studies have reported this condition as a normal finding in patients without this diagnosis (9). In this case, high pressure values were seen in all four limbs and with very different data between the two lower limbs, which helped increase the suspicion of the diagnosis.
Additional studies, such as electrocardiogram and chest X-ray, may not show pathological findings (1). The dissection of the right coronary artery is associated with acute myocardial infarction with ST elevation in the lower face (10), which is not evident in this case, since AAD extended only until the arch, without involving the ascending aorta. 12% to 15% of patients have normal x
X-rays (6), especially if the damage is limited to the ascending aorta (1), so an X-ray with normal mediastinum does not rule out AAD; for example, radiological findings did not suggest the syndrome in this patient.
Renal failure can occur in 10% of patients with type B dissection, as in this case: creatinine 1.39 mg/dl, with estimated glomerular filtration rate of 50 ml/min. The cause of this situation is related to hypoperfusion and strokes when the renal arteries (7) are involved, which often requires additional studies to establish the AAD diagnosis. As to chest CT with aorta protocol, sensitivity of 99% and specificity 00% for this diagnosis was found (9). Similarly, determining the role of markers such as D-dimer, which, with a negative value in a low-risk patient, helps to exclude the diagnosis (11) has been attempted.
Moreover, within the atypical manifestations of AAD, bilateral testicular pain is described in few previous publications. Two cases in Europe are found: one patient in Italy, who was confirmed dissection of the abdominal aorta (12), and another in the UK, who presented a clinical picture of six months that was initially treated as pyelonephritis and epididymitis, but was diagnosed with type A AAD during the study of acute renal failure (13). There are also two reports in North America, both in the United States: the first related to a patient admitted with hypertension, who presented with cardiac arrest due to pulseless electrical activity and received type A AAD diagnosis at necropsy (14); the second is related to a patient who, despite the history of nephrolithiasis and persistent hypertension, received type B AAD diagnosis (15). No cases have been reported in Colombia or in Latin America.
Regarding the clinical picture, differential diagnoses that may arise when a patient presents with scrotal pain localized in the testicular region are urolithiasis, orchitis, epididymitis, prostatitis, varicocele, spermatocele, hydrocele, strangulated hernia, acute appendicitis, vasculitis, testicular torsion, among others (13).
Although suspected aortic dissection is suggested in most previously reported clinical cases, it should be noted that usually these entities are not present with bilateral testicular pain (12-14), which is why the variability of the clinical picture may be secondary to the intrinsic anatomic structure of the aortic wall, and which may cause the patient to present with systemic symptoms or signs secondary to hypoperfusion (5). Bilateral testicular pain, such as in this patient, can be explained by an expanding aneurysm or hematoma that compresses ilioinguinal or genitofemoral nerves within the psoas muscle (13,14).
As to the procedure, the group of specialists of the institution chose a medical treatment according to the literature, where there is no conclusive data of a difference between mortality rates and optimal medical treatment or endovascular therapy, survival of 95.6% against 89.6%, respectively (1). In cases of uncomplicated type B AAD —absence of persistent or recurrent pain, difficulty controlling blood pressure values, progression of the dissection or poor perfusion with rupture and hemothorax, periaortic or mediastinal hematoma— considering surgical treatment is not necessary, since surgery can increase mortality rates up to 50% (1).
Conclusions
The clinical presentation of the AAD is variable, so it should be suspected in atypical clinical pictures such as bilateral testicular pain, especially if pathological findings are not present at physical examination, there is persistent pain, history and clinical hypertension and additional risk factors. Clinical suspicion is the most important fact for early diagnosis, since it is the main determinant of survival in these patients due to the high mortality of AAD.
This case is the first report made of AAD in Colombia and Latin America with clinical presentation of bilateral testicular pain, which helps broaden the spectrum of differential diagnosis in patients arriving in the emergency department with sudden, severe scrotal pain and that should raise the diagnostic suspicion of this disease.
Conflict of interests
None stated by the authors.
Funding
None stated by the authors.
Acknowledgements
None stated by the authors.
References
1.Erbel R, Aboyans V, Boileau C, Bossone E, Bartolomeo RD, Eggebrecht H, et al. 2014 ESC Guidelines on the diagnosis and treatment of aortic diseases. Eur. Heart J. 2014;35(41):2873-926. http://doi.org/f3pkkr.
2.Patel PD, Arora RR. Pathophysiology, diagnosis, and management of aortic dissection. Ther. Adv. Cardiovasc. Dis. 2008;2(6):439-68. http://doi.org/bc9mrz.
3.Pacini D, Di Marco L, Fortuna D, Belotti LM, Gabbieri D, Zussa C, et al. Acute aortic dissection: epidemiology and outcomes. Int. J. Cardiol. 2013;167(6):2806-12. http://doi.org/bpj9.
4.Sica G, Bocchini G, Guida F, Supino FS, Tanga M, Scaglione M. Cardiothoracic Imaging Aortic Dissection – The Great Simulator. Eur. Med. Imaging. Rev. 2008;17-9.
5.Braverman AC. Acute aortic dissection: Clinician update. Circulation. 2010;122(2):184-8. http://doi.org/fvr745.
6.Nienaber CA, Clough RE. Management of acute aortic dissection. Lancet. 2015;385(9970):800-11. http://doi.org/f259tv.
7.Tsai TT, Nienaber CA, Eagle KA. Acute aortic Syndromes. Circulation. 2005;112(24):3802-13. http://doi.org/bsb3c3.
8.Klompas M. Does This Patient Have an Acute Thoracic Aortic Dissection? JAMA. 2002;287(17):2262-72. http://doi.org/dpp7d7.
9.Diercks DB, Promes SB, Schuur JD, Shah K, Valente JH, Cantrill SV. Clinical Policy: Critical Issues in the Evaluation and Management of Adult Patients With Suspected Acute Nontraumatic Thoracic Aortic Dissection. Ann. Emerg. Med. 2015;65(1):32-42. http://doi.org/bpkc.
10.Braunwald E. Capítulo 56. Enfermedades de la aorta. In: Libby P, Bonow R, Mann D, Zipes D, editors. Braunwald E. Tratado de Cardiología. Texto de Medicina Cardiovascular. Volumen 1. 8th ed. Elsevier Saunders; 2009. [Cited 2016 Mar 19]. Available from: https://goo.gl/EWG0Cj.
11.Asha SE, Miers JW. A Systematic Review and Meta-analysis of D-dimer as a Rule-out Test for Suspected Acute Aortic Dissection. Ann. Emerg. Med. 2015;66(4):368-78. http://doi.org/bpkd.
12.Cacciotti L, Camastra GS, Musarò S, Passaseo I, Ansalone G. Abdominal aortic dissection with atypical presentation. Intern. Emerg. Med. 2011;6(2):193-4. http://doi.org/dwb6jn.
13.Jarvis S, Donohoe P, Huang D, Macdougall IC. Unusual presentation of Aortic Dissection with Bilateral Testicular Pain and Rapidly Deteriorating Renal Function. Urology. 2014;83(5):989-91.
http://doi.org/f2rg66.
14.Chan-Tack KM. Aortic Dissection Presenting as Bilateral Testicular Pain. N. Engl. J. Med. 2000;343(16):1199. http://doi.org/bq387p.
15.Siddiqui MS, Haider I. Testicular Pain, Trouble Voiding and Hypertension: “Dissecting the Possibilities.” JACC. 2014;63(12):A700.
http://doi.org/f2qxk4.
Referencias
Erbel R, Aboyans V, Boileau C, Bossone E, Bartolomeo RD, Eggebrecht H, et al. 2014 ESC Guidelines on the diagnosis and treatment of aortic diseases. Eur. Heart J. 2014;35(41):2873-926. http://doi. org/f3pkkr.
Patel PD, Arora RR. Pathophysiology, diagnosis, and management of aortic dissection. Ther. Adv. Cardiovasc. Dis. 2008;2(6):439-68. http://doi. org/bc9mrz.
Pacini D, Di Marco L, Fortuna D, Belotti LM, Gabbieri D, Zussa C, et al. Acute aortic dissection: epidemiology and outcomes. Int. J. Cardiol. 2013;167(6):2806-12. http://doi. org/bpj9.
Sica G, Bocchini G, Guida F, Supino FS, Tanga M, Scaglione M. Cardiothoracic Imaging Aortic Dissection – The Great Simulator. Eur. Med. Imaging. Rev. 2008;17-9.
Braverman AC. Acute aortic dissection: Clinician update. Circulation. 2010;122(2):184-8. http://doi. org/fvr745.
Nienaber CA, Clough RE. Management of acute aortic dissection. Lancet. 2015;385(9970):800-11. http://doi. org/f259tv.
Tsai TT, Nienaber CA, Eagle KA. Acute aortic Syndromes. Circulation. 2005;112(24):3802-13. http://doi. org/bsb3c3.
Klompas M. Does This Patient Have an Acute Thoracic Aortic Dissection? JAMA. 2002;287(17):2262-72. http://doi. org/dpp7d7.
Diercks DB, Promes SB, Schuur JD, Shah K, Valente JH, Cantrill SV. Clinical Policy: Critical Issues in the Evaluation and Management of Adult Patients With Suspected Acute Nontraumatic Thoracic Aortic Dissection. Ann. Emerg. Med. 2015;65(1):32-42. http://doi. org/bpkc.
Braunwald E. Capítulo 56. Enfermedades de la aorta. In: Libby P, Bonow R, Mann D, Zipes D, editors. Braunwald E. Tratado de Cardiología. Texto de Medicina Cardiovascular. Volumen 1. 8th ed. Elsevier Saunders; 2009. [Cited 2016 Mar 19]. Available from: https://goo. gl/EWG0Cj.
Asha SE, Miers JW. A Systematic Review and Meta-analysis of D-dimer as a Rule-out Test for Suspected Acute Aortic Dissection. Ann. Emerg. Med. 2015;66(4):368-78. http://doi. org/bpkd.
Cacciotti L, Camastra GS, Musarò S, Passaseo I, Ansalone G. Abdominal aortic dissection with atypical presentation. Intern. Emerg. Med. 2011;6(2):193-4. http://doi. org/dwb6jn.
Jarvis S, Donohoe P, Huang D, Macdougall IC. Unusual presentation of Aortic Dissection with Bilateral Testicular Pain and Rapidly Deteriorating Renal Function. Urology. 2014;83(5):989-91.
http://doi. org/f2rg66.
Chan-Tack KM. Aortic Dissection Presenting as Bilateral Testicular Pain. N. Engl. J. Med. 2000;343(16):1199. http://doi. org/bq387p.
Siddiqui MS, Haider I. Testicular Pain, Trouble Voiding and Hypertension: “Dissecting the Possibilities. ” JACC. 2014;63(12):A700.
http://doi. org/f2qxk4.
Cómo citar
APA
ACM
ACS
ABNT
Chicago
Harvard
IEEE
MLA
Turabian
Vancouver
Descargar cita
CrossRef Cited-by
1. Ramy Mando, Daniel Tim, Anthony DeCicco, Justin Trivax, Ivan Hanson. (2020). Master of the Masquerade: An Atypical Presentation of Acute Aortic Dissection. Case Reports in Cardiology, 2020, p.1. https://doi.org/10.1155/2020/5743985.
Dimensions
PlumX
Visitas a la página del resumen del artículo
Descargas
Licencia
Derechos de autor 2017 Revista de la Facultad de Medicina

Esta obra está bajo una licencia Creative Commons Reconocimiento 3.0 Unported.
-