Problems perceived and experienced by health professionals rendering social service in Ancash, Peru. 2015
Problemas percibidos y experimentados por profesionales de salud durante el servicio social en Ancash, Perú. 2015
DOI:
https://doi.org/10.15446/revfacmed.v65n3.59055Palabras clave:
Primary Health Care, Rural Health, Health Personnel, Job Satisfaction (en)Atención primaria de salud, Salud rural, Personal de salud, Satisfacción en el trabajo (es)
Descargas
Introduction: Social health services in Peru have certain problems such as unsafe work conditions, mortality associated with traffic accidents and poor insurance coverage.
Objective: To describe the problems perceived and experienced by health professionals who render Rural and Urban Marginal Health Service (SERUMS in Spanish) in Ancash (Peru), and to evaluate their association with the profession and the category of the facilities where SERUMS is rendered.
Materials and methods: In April 2015, an analytical cross-sectional study was carried out in professionals who were rendering SERUMS in facilities of the Ministry of Health in Ancash. Surveys were applied to collect general data, and characteristics and problems of SERUMS.
Results: 364 surveys were analyzed. 79.3% were females, and the average age was 27.4±5.0 years. During SERUMS, 80.0% of participants perceived lack of supplies, 54.4% perceived excessive workload, and 14.7% suffered some traffic accident. Being a physician and working in I-1 health facilities were factors associated with suffering traffic accidents and other kind of accidents.
Conclusions: Respondents reported excessive workload, lack of supplies, and accidents. Accidents were more frequent in physicians and in I-1 health facilities.
Introducción. En Perú, durante el servicio social en salud se han reportado problemas como condiciones laborales riesgosas, mortalidad asociada a accidentes de tránsito y déficit de cobertura de aseguramiento.
Objetivo. Describir los problemas percibidos y experimentados por los profesionales de salud que realizan el Servicio Rural y Urbano Marginal de Salud (SERUMS) en Ancash, Perú, y evaluar su asociación con la práctica de los profesionales y la categoría del establecimiento donde se realiza el SERUMS.
Materiales y métodos. Durante abril del 2015, se realizó un estudio transversal analítico con profesionales de salud que realizaban el SERUMS en establecimientos del Ministerio de Salud de Ancash. Se aplicaron encuestas para recolectar datos generales, características y problemas del SERUMS.
Resultados. Se analizaron 364 encuestas. El 79.3% de los participantes fue de sexo femenino, la edad promedio fue de 27.4±5.0 años, 80.0% percibió carencia de insumos, 54.4% percibió carga laboral excesiva, y 14.7% sufrió algún accidente de tránsito durante el SERUMS. Ser médico y laborar en establecimientos I-1 fueron factores asociados a haber sufrido accidentes de tránsito y otros imprevistos.
Conclusiones. Los encuestados reportan carga laboral excesiva, carencia de insumos y accidentes. Los accidentes son más frecuentes en médicos y en establecimientos de categoría I-1.
Original research
DOI: https://doi.org/10.15446/revfacmed.v65n3.59055
Problems perceived and experienced by health professionals
rendering social service in Ancash, Peru. 2015
Problemas percibidos y experimentados por profesionales de salud
durante el servicio social en Ancash, Perú. 2015
Received: 14/07/2016. Accepted: 20/09/2016.
Álvaro Taype-Rondan1,2 • María Isabel Vidal-Torres3 • Kocfa Chung-Delgado4 • Jesús Maticorena-Quevedo4 • Percy Mayta-Tristán4,5
1 Universidad Peruana Cayetano Heredia - CRONICAS Center for Excellence in Chronic Diseases - Lima - Peru.
2 Universidad de San Martín de Porres - Centro de Epidemiología Clínica y Medicina Basada en Evidencias - Lima - Perú
3 Regional Health Directorate of Ancash - Regional SERUMS Coordination - Ancash - Peru.
4 Universidad Peruana de Ciencias Aplicadas - Faculty of Health Sciences - School of Medicine - Lima - Perú.
5 Universidad Científica del Sur - Research and Development Directorate - Lima - Perú.
Corresponding author: Álvaro Taype-Rondan. CRONICAS Center for Excellence in Chronic Diseases, Universidad Peruana
Cayetano Heredia. Avenida Armendariz 497, piso 2, Miraflores, Lima 18. Phone number: +51 1 2416978. Lima. Peru.
Email: alvaro.taype.r@gmail.com.
| Abstract |
Introduction: Social health services in Peru have certain problems such as unsafe work conditions, mortality associated with traffic accidents and poor insurance coverage.
Objective: To describe the problems perceived and experienced by health professionals who render Rural and Urban Marginal Health Service (SERUMS in Spanish) in Ancash (Peru), and to evaluate their association with the profession and the category of the facilities where SERUMS is rendered.
Materials and methods: In April 2015, an analytical cross-sectional study was carried out in professionals who were rendering SERUMS in facilities of the Ministry of Health in Ancash. Surveys were applied to collect general data, and characteristics and problems of SERUMS.
Results: 364 surveys were analyzed. 79.3% were females, and the average age was 27.4±5.0 years. During SERUMS, 80.0% of participants perceived lack of supplies, 54.4% perceived excessive workload, and 14.7% suffered some traffic accident. Being a physician and working in I-1 health facilities were factors associated with suffering traffic accidents and other kind of accidents.
Conclusions: Respondents reported excessive workload, lack of supplies, and accidents. Accidents were more frequent in physicians and in I-1 health facilities.
Keywords: Primary Health Care; Rural Health; Health Personnel; Job Satisfaction (MeSH).
Taype-Rondan A, Vidal-Torres MA, Chung-Delgado K, Maticorena-Quevedo J, Mayta-Tristán P. Problems perceived and experienced by health professionals rendering social service in Ancash, Peru. 2015. Rev. Fac. Med. 2017;65(3):441-6. English. doi: https://doi.org/10.15446/revfacmed.v65n3.59055.
| Resumen |
Introducción. En Perú, durante el servicio social en salud se han reportado problemas como condiciones laborales riesgosas, mortalidad asociada a accidentes de tránsito y déficit de cobertura de aseguramiento.
Objetivo. Describir los problemas percibidos y experimentados por los profesionales de salud que realizan el Servicio Rural y Urbano Marginal de Salud (SERUMS) en Ancash, Perú, y evaluar su asociación con la práctica de los profesionales y la categoría del establecimiento donde se realiza el SERUMS.
Materiales y métodos. Durante abril del 2015, se realizó un estudio transversal analítico con profesionales de salud que realizaban el SERUMS en establecimientos del Ministerio de Salud de Ancash. Se aplicaron encuestas para recolectar datos generales, características y problemas del SERUMS.
Resultados. Se analizaron 364 encuestas. El 79.3% de los participantes fue de sexo femenino, la edad promedio fue de 27.4±5.0 años, 80.0% percibió carencia de insumos, 54.4% percibió carga laboral excesiva, y 14.7% sufrió algún accidente de tránsito durante el SERUMS. Ser médico y laborar en establecimientos I-1 fueron factores asociados a haber sufrido accidentes de tránsito y otros imprevistos.
Conclusiones. Los encuestados reportan carga laboral excesiva, carencia de insumos y accidentes. Los accidentes son más frecuentes en médicos y en establecimientos de categoría I-1.
Palabras clave: Atención primaria de salud; Salud rural; Personal de salud; Satisfacción en el trabajo (DeCS).
Taype-Rondan A, Vidal-Torres MA, Chung-Delgado K, Maticorena-Quevedo J, Mayta-Tristán P. [Problemas percibidos y experimentados por profesionales de salud durante el servicio social en Ancash, Perú.] 2015. Rev. Fac. Med. 2017;65(3):441-6. English. doi: https://doi.org/10.15446/revfacmed.v65n3.59055.
Introduction
Given the inequities in the distribution of human resources in health, many countries establish social service policies, which encourage, condition or force health professionals to work in areas with poor access to health services to serve the most vulnerable populations (1-3). In Latin America, the obligatory nature of social service has been discussed in publications of Colombia (1), Mexico (2) and Peru (3).
In Peru, social service in health is known as Rural and Urban Marginal Health Service (SERUMS in Spanish) and the professionals who render their services are known as serumists. SERUMS regulates the practice of physicians, dentists, nurses, obstetricians, chemist-pharmacists, nutritionists, medical technologists, social workers, biologists, psychologists, veterinarians and sanitary engineers. Rendering SERUMS is mandatory to apply for positions in public entities, study professional specialization programs in Peru, and receive scholarships or other equivalent aids from the State (4).
SERUMS has managed to locate health professionals in many rural and remote areas of Peru. However, serious problems for professionals have been reported when rendering their services, such as the mandatory nature of the service, risky working conditions and real danger of death (3). In addition, studies carried out in physicians who render SERUMS have identified poor health insurance (5) and high mortality due, to a great extent, to traffic events (6,7).
In spite of the relevance of these problems, studies on serumists are scarce and have focused only on physicians. Due to the lack of information on the frequency of the problems and their risk groups, designing and prioritizing the corresponding interventions is difficult (8). Therefore, this study aims to describe the problems perceived and experienced by serumists in Ancash - Peru, and to evaluate their association with the professional practice of serumists and the category of the facilities where SERUMS is rendered.
Materials and methods
Study design and context
An analytical cross - sectional study was carried out applying surveys to healthcare professionals rendering SERUMS in Ancash, Peru.
In Peru, health facilities are divided into first, second and third level of care. First level prioritizes health prevention and promotion, and is divided into four categories: I-1, I-2, I-3 and I-4. Usually, category I-1 includes facilities with few equipment and are found in most rural areas away from reference health centers (9).
SERUMS is regulated by Law 23330 (4), which establishes that it must be rendered in public health facilities of the Ministry of Health (MINSA), Social Security (EsSalud) or the Health Departments of the Armed Forces and the National Police of Peru for a year. Each year two processes are opened to award contracts: one in May (with the highest number of open positions) and another in October (with fewer positions).
Participants
This study included health professionals who were rendering SERUMS at a MINSA facility in Ancash during April 2015. This region was chosen because of the logistical support provided by the Regional Health Directorate of Ancash (DIRESA-Ancash). Working with MINSA health facilities was agreed because more serumist specialists are found there, and contact between them and the SERUMS coordinators, who were in charge of applying the surveys, is more frequent.
DIRESA-Ancash is divided into six geographically distributed health networks: Pacífico Sur (South Pacific), Pacífico Norte (North Pacific), Huaylas Sur (South Huaylas), Huaylas Norte (North Huaylas), Conchucos Sur (South Conchucos) and Conchucos Norte (North Conchucos). Each health network has a SERUMS coordinator, who is in charge of directing the work of the serumist specialists in their network.
During April 2015, 644 health professionals were rendering SERUMS in DIRESA-Ancash: 573 (89.0%) were located in MINSA health facilities, 42 (6.5%) in EsSalud health facilities, and 29 (4.5%) in health facilities of the Health Departments of the Armed Forces and the National Police.
Out of 573 MINSA members, the coordinators managed to involve 364 (63.5%), all of whom agreed to participate in this study. The health network with the highest percentage of respondents was Conchucos Sur (92.3%), and the lowest percentage was observed in Pacífico Norte (23.6%) (Figure 1).
Procedures
DIRESA-Ancash permission was requested to carry out the study and, with their support, the SERUMS coordinators of each health network in Ancash were trained to apply the surveys and respond the questions raised by serumists. The telephone number of the principal investigator was provided in all the surveys so that serum specialists could contact him in case of doubt.
In order to apply the surveys in their respective network, the SERUMS coordinators used two methods: a) applying the survey to serumists in person during meetings and supervision sessions in the health facilities, and b) sending the surveys to the health facilities where the serumists worked. In both cases, the participants used an envelope to submit their answers anonymously. This data collection was conducted throughout April 2015.
Then, two authors typed the surveys twice in the Excel 2010 program (Microsoft Corporation, USA), while a third author verified if both versions coincided. Mismatches were typed again.
Variables
The survey was developed by the researchers and included the following sections: general data such as age, sex, marital status, place where the undergraduate program was studied, financing of the university where the undergraduate program was studied, profession, year of graduation, as well as characteristics of the SERUMS such as type of contract, category of the health facility, process of enrollment in SERUMS (2014-I or 2014-II), at least three months being the head of the health facility, SERUMS problems, among others.
Regarding problems with SERUMS, the survey inquired about experiencing the following during the past month or at some point of their SERUMS: perception of lack of supplies that has prevented the basic management of a patient, some traffic accidents while working or traveling to the health facility, some other accidents (blows, burns, falls, etc.) while working that has caused incapacity for at least a few hours, or some theft while working.
In addition, data on other variables that are not included in this article were collected and will be presented in a subsequent analysis. These variables correspond to the following parts of the survey: difficulty of SERUMS, violence during SERUMS, depressive symptoms during the last two weeks, professional expectations and retention.
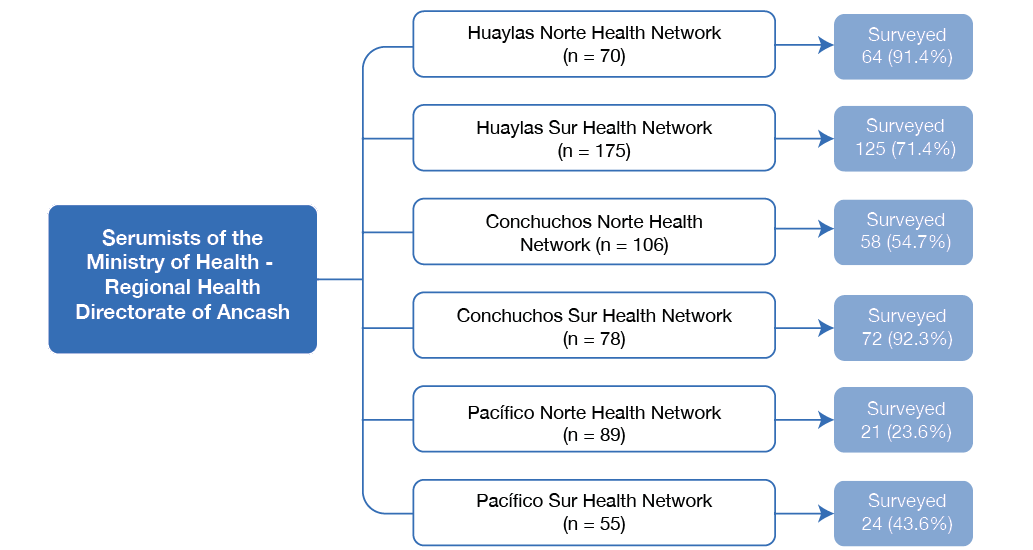
Figure 1. Serumists from the Ministry of Health surveyed in each of the six networks of the Ancash Regional Health Directorate.
Source: Own elaboration based on the data obtained in the study.
Analysis plan
Data analysis was performed using the statistical software Stata v14.0 (StataCorp LP, USA). Central tendency measures, dispersion measures, absolute frequencies and relative frequencies were used for a descriptive presentation of the results. Prevalence ratios (PR) and 95% confidence intervals (95%CI) were estimated using crude and adjusted Poisson regressions with robust variance. p<0.05 was considered statistically significant.
The regression models evaluated the association between five outcomes of interest (excessive workload in last month, lack of supplies in last month, traffic accident during SERUMS, another type of accident during SERUMS, robbery during SERUMS), and two variables of interest (being a physician and rendering SERUMS in a category I-1 health facility).
For multiple regression models, the associations were adjusted for sex, age, undergraduate studies in Ancash, years passed since graduation until starting SERUMS, having a remunerated SERUMS contract, having served as head of the health facility for at least three months during SERUMS, rending SERUMS at an I-1 health facility, and being a physician.
Ethical considerations
The project was approved by the Ethics Committee of Hospital Nacional Docente Madre-Niño San Bartolomé (RCEI-40). Surveys were voluntary and anonymous, so participants signed an informed consent. The confidentiality of the collected data was preserved.
Results
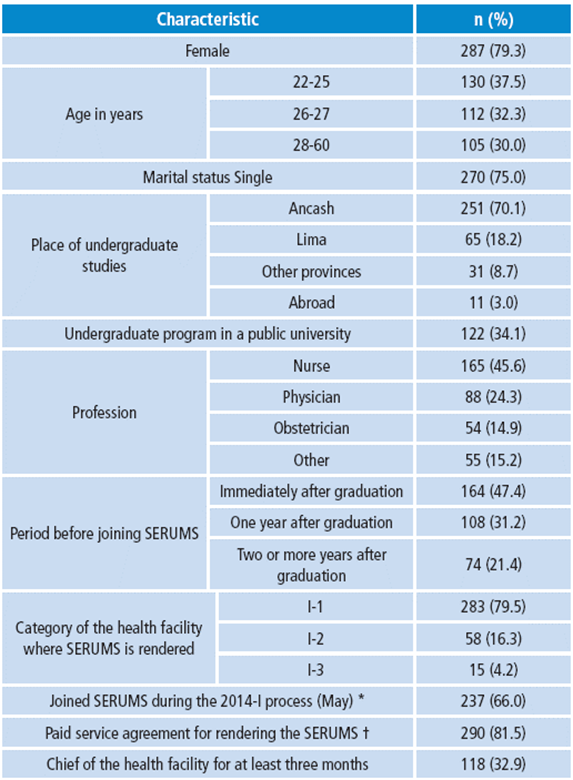
364 surveys were applied to professionals who rendered SERUMS at MINSA facilities in Ancash in April 2015. 79.3% were female, the mean age was 27.4±5.0, 75.0% were single, 70.1% studied an undergraduate program in a university of Ancash, 45.6% were nurses, 24.3% were physicians, 47.4% entered the SERUMS just after graduating, 79.5% were rendering SERUMS in an I-1 health facility, and 81.5% were rendering SERUMS and being remunerated (Table 1).
When evaluating the problems faced by serumists during their service, it was found that 80.0% perceived that they lacked the necessary supplies for the basic management of a patient, and 51.6% perceived it during the last month. 54.4% perceived that the workload was excessive at some point, while 28.8% perceived it in the last month. 14.7% suffered some traffic accident during SERUMS while working or when traveling to their workplace, and 4.0% suffered it in the last month. 26.2% suffered other accidents (bumps, burns, falls, etc.) during SERUMS, which made them unable to work for at least a few hours, and 9.3% suffered an accident during the last month. 12.4% were robbed during SERUMS activities, and 9.3% was robbed during the last month (Table 2).
When evaluating the association between variables in the adjusted model, it was observed that rendering SERUMS at an I-1 health facility was associated with traffic accidents (PR=2.64; 95%CI: 1.00-6.99) and to suffering another accident during SERUMS (PR=2.81; 95%CI: 1.26-6.26). Similarly, being a physician was a factor associated with suffering another accident during SERUMS (PR=1.66; 95%CI: 1.00-2.75) (Table 3).
Table 1. Characteristics of the surveyed population (n=364).
|
Characteristic |
n (%) |
||
|
Female |
287 (79.3) |
||
|
Age in years |
22-25 |
130 (37.5) |
|
|
26-27 |
112 (32.3) |
||
|
28-60 |
105 (30.0) |
||
|
Marital status Single |
270 (75.0) |
||
|
Place of undergraduate studies |
Ancash |
251 (70.1) |
|
|
Lima |
65 (18.2) |
||
|
Other provinces |
31 (8.7) |
||
|
Abroad |
11 (3.0) |
||
|
Undergraduate program in a public university |
122 (34.1) |
||
|
Profession |
Nurse |
165 (45.6) |
|
|
Physician |
88 (24.3) |
||
|
Obstetrician |
54 (14.9) |
||
|
Other |
55 (15.2) |
||
|
Period before joining SERUMS |
Immediately after graduation |
164 (47.4) |
|
|
One year after graduation |
108 (31.2) |
||
|
Two or more years after graduation |
74 (21.4) |
||
|
Category of the health facility where SERUMS is rendered |
I-1 |
283 (79.5) |
|
|
I-2 |
58 (16.3) |
||
|
I-3 |
15 (4.2) |
||
|
Joined SERUMS during the 2014-I process (May) * |
237 (66.0) |
||
|
Paid service agreement for rendering the SERUMS † |
290 (81.5) |
||
|
Chief of the health facility for at least three months |
118 (32.9) |
||
* The others entered during the 2014-II process (October).
† The others had an equivalent contract (ad honorem).
Source: Own elaboration based on data obtained in the study.
Table 2. Problems perceived and experienced sometime during SERUMS and sometime during the last month.
|
Problems |
Total |
Level of the health facility |
Profession |
||||
|
I-1 |
I-2/I-3 |
Nurse |
Physician |
Other |
|||
|
Sometime during the SERUMS |
Lack of supplies |
280 (80.0) * |
221 (79.8) |
59 (80.8) |
119 (73.9) |
75 (85.2) |
91 (85.1) |
|
Excessive workload |
191 (54.4) |
159 (56.6) |
32 (45.7) |
96 (60.0) |
47 (53.4) |
49 (44.9) |
|
|
Traffic accidents |
50 (14.7) |
45 (16.6) |
5 (7.3) |
19 (12.2) |
19 (22.4) |
12 (11.5) |
|
|
Other accidents |
91 (26.2) |
84 (30.3) |
7 (10.0) |
37 (23.0) |
35 (41.2) |
21 (19.6) |
|
|
Thefts |
43 (12.4) |
36 (12.9) |
7 (10.3) |
19 (11.8) |
16 (18.2) |
9 (8.7) |
|
|
Sometime during the past month |
Lack of supplies |
129 (51.6) |
98 (50.3) |
31 (56.4) |
52 (45.6) |
33 (54.1) |
47 (59.5) |
|
Excessive workload |
84 (28.8) |
70 (30.6) |
14 (22.2) |
44 (34.7) |
18 (25.0) |
22 (22.5) |
|
|
Traffic accidents |
13 (4.0) |
10 (3.9) |
3 (4.4) |
5 (3.3) |
2 (2.6) |
6 (5.8) |
|
|
Other accidents |
29 (9.3) |
29 (11.8) |
0 (0.0) |
16 (10.7) |
6 (8.8) |
8 (8.0) |
|
|
Thefts |
13 (3.9) |
12 (4.5) |
1 (1.5) |
9 (5.8) |
3 (3.7) |
1 (1.0) |
|
* n (%).
Source: Own elaboration based on data obtained in the study.
Table 3. Variables observed and their association with working in a category I-1 health facility or being a physician.
|
Characteristic |
Health facility of category I-1 |
Medical profession |
||
|
Crude |
Adjusted † |
Crude |
Adjusted ‡ |
|
|
Lack of supplies in the last month |
0.99 |
0.94 |
1.09 |
0.99 |
|
Excessive workload in the last month |
1.24 |
1.07 |
0.99 |
0.95 |
|
Traffic accidents during SERUMS |
2.29 |
2.64 |
1.87 |
1.49 |
|
Other accidents during SERUMS |
3.03 |
2.81 |
1.90 |
1.66 |
|
Thefts during SERUMS |
1.25 |
1.13 |
1.72 |
1.99 |
* PR (95%CI).
† Adjusted for sex, age, university region, year of graduation (delay), equivalent contract, head of health facility and profession.
‡ Adjusted for sex, age, university region, year of graduation (delay), equivalent contract, head of health facility and health facility category.
Source: Own elaboration based on data obtained in the study.
Discussion
Excessive workload
54.4% of respondents perceived that the workload during SERUMS was excessive at some point, while 28.8% perceived it in the last month. These high figures could reflect the lack of staff in the health facilities where SERUMS is rendered, as well as inadequate training of serumists or lack of support from senior staff of the health facility.
Serumists often have little work experience. In addition, they must perform administrative and institutional management tasks for which they may not have adequate preparation during undergraduate training. It is therefore necessary to explore this workload and to evaluate proposed solutions such as telemedicine —which has proven to be effective to reduce the burden on health professionals working in rural areas in other countries— (10) or different training methods to assist serumists in their clinical and administrative work.
Lack of supplies
51.6% of the respondents said that the lack of supplies hindered the fulfillment of their duties some time during the last month. These shortcomings are characteristic in rural health services worldwide, especially in low and middle-income countries. They usually occur because budgets prioritize urban areas, while the budget allocated to rural areas is misapplied under the belief that these areas are “small cities” and that their health facilities are supplied in the same way as urban areas (11,12).
In Peru, first level health facilities are designed to carry out mostly promotional and preventive activities and to manage a small group of pathologies, deriving the most complex conditions to higher-level health facilities (13). However, this is not always possible due to the patients’ fear, their economic status, the need for immediate action, the distance from higher-level health facilities or their denial to receive patients. These situations force health professionals to treat pathologies for which they do not have enough supplies (14, 15), and to provide suboptimal care that ends up promoting health inequity in rural areas (12).
To intervene this inequity, it is necessary to study in depth the lack of supplies and the best ways to overcome the situation. A recent qualitative study indicates that the interviewed serumists require diagnostic tests for specific decisions such as making a differential diagnosis between malaria and pneumonia in the jungle (14). These studies would identify the particular needs of each region and guide an efficient investment in supplies that could be used in rural areas (16).
In addition, it is important for health personnel at all levels of care to know what kind of pathologies they can treat in the health facilities where they are working and how they should refer patients to the next level of care. These issues could be assessed during pre-SERUMS training (17,18).
Accidents
In Peru, the estimated incidence of traffic incidents in persons over 18 years of age was 223 per 100 000 people in 2008 (19). This study found that 14.7% of the respondents (14 700 per 100 000 people) reported being involved in a traffic accident during their SERUMS (that is, during the last 6 or 12 months). Despite the methodological differences between the cited study and this study, it is possible to assume that serumists have a high risk of suffering this type of accidents compared the rest of Peruvian inhabitants.
A report that only included serumist physicians in the 2006-2009 period identified traffic accidents as the leading cause of death, with a record of 7 deaths by traffic accidents out of 5 531 medical professionals (126.6 deaths per 100 000) (6). This incidence is much higher than that observed in reports of deaths among young physicians in other countries (20). Moreover, during that period, the estimated incidence of fatal traffic incidents among Peruvian citizens over the age of 18 was only 20 per 100 000 inhabitants (19).
The models evaluated in this study show that the prevalence of suffering traffic accidents during SERUMS is higher for physicians than for non-physicians, although, in the adjusted analysis, this association is not significant. This may occur because physicians make more trips, either referring patients or returning to their cities of origin, which may be quite distant, and because more than two thirds of the physicians surveyed have completed their studies in regions other than Ancash. Furthermore, an association between traffic accidents and SERUMS was found in relation to a category I-1 facility; this can be attributed to the remoteness and difficult access to these health facilities and their annexes.
Unfortunately, national data on mortality in non-medical serumists is not available. Data on other consequences of traffic accidents, such as temporary or permanent disability, are not available either. These data are necessary to develop and evaluate prevention
policies (21).
The prevalence of other accidents (blows, burns, falls, etc.) while fulfilling serumist work was also higher in category I-1 health facilities. This may happen due to the fact that the communities served by these health facilities are more distant, which forces professionals to move for great distances to provide care, often using unsafe means of transportation in irregular terrains that may cause failures. In addition, these accidents were more prevalent in physicians, perhaps because they are more likely to move to remote locations, even to other villages, to treat their patients.
Unfortunately, many serumists do not have health insurance to protect them in case of accidents. Reports show that within three months after starting the contract, only 6.6% of the serumist physicians are provided with a social health insurance coverage for accidents and death (5), which causes multiple expenses and inconveniences to serumists who are involved in these accidents.
Now that the risks to which serumists are exposed are known, it is imperative that the relevant authorities take action. It is necessary to monitor the minimum security and access conditions to health facilities, to give serumists the possibility of accumulating days off to reduce the number of trips, and to provide vehicles or fuel for mobilization to remote communities. Interventions and monitoring should be prioritized for the groups at risk, in other words, physicians and those who work at I-1 health facilities.
It should be noted that this problem affects staff satisfaction and negatively influences the retention of health personnel (22), since it discourages serumist workers from working at the first level of care, as suggested by a previous cohort (23).
Limitations
This study has some limitations, such as the fact that our outcomes of interest were evaluated in a subjective way, according to the perception of the surveyor. In addition, the SERUMS coordinators could not find 36.5% of the serumists. It is possible that the missing population corresponds to those who render SERUMS in the most remote health facilities and, therefore, those who have more problems; hence, the results may underestimate the true magnitude of this issue.
Likewise, the extrapolation of the results is limited only to serumists of MINSA health facilities in Ancash. Serumists working for other health care providers or in other regions are likely to provide very different figures, which should be the subject of future studies.
The size of the sample included in this study has a power greater than 80% to determine PR values greater than 2.1 using multiple Poisson regressions, calculated with the PASS program v13.0 (NCSS, LLC, USA.). This implies that some associations could not be statistically confirmed due to the small size of the sample. However, no more subjects could be obtained since this was a census evaluation.
Strengths
To the knowledge of the authors, this is the first study to carry out a quantitative evaluation of the problems reported by the professionals who render SERUMS in Peru. The results reveal the magnitude of certain problems and identify two risk groups, which will help to develop and implement interventions to improve the working conditions of the serumist specialists.
Conclusions
The professionals who render SERUMS in Ancash suffer from excessive workload, lack of supplies, accidents and thefts. Being a physician and working in category I-1 health facilities are factors associated with suffering traffic accidents and other accidents that endanger integrity and even life. The relevant health authorities must supervise access and security conditions in such health facilities, prioritizing the identified risk groups.
Authors’ contributions
This article was planned by ATP and PMT. ATR and MIVT were in charge of data collection. ATP, KCD, JMQ and PMT analized and interpreted the data. Finally, all authors participated in the drafting and approval of the final version of this document.
Conflict of interest
During the study, María Isabel Vidal-Torres was in charge of the Regional Coordination of SERUMS in the Regional Health Directorate of Ancash. The remaining authors do not state any conflicts of interest regarding the publication of this article.
Funding
The Regional Health Directorate of Ancash financed the printing of the instruments for data collection and application. The authors financed the remaining expenses.
Acknowledgement
The authors would like to express their gratitude to the authorities of the Regional Health Directorate of Ancash for granting their permission to conduct this study, and to the SERUMS coordinators of the Ancash health networks for their support in data collection.
References
1.Moya MJ. Servicio social obligatorio en Colombia: incertidumbre de los recién graduados en medicina. Rev. Méd. Risaralda. 2014;20(2):114-120.
2.Nigenda G. Servicio social en medicina en México. Una reforma urgente y posible. Salud Publica Mex. 2013;55(5):519-27.
3.Mayta-Tristán P, Poterico JA, Galán-Rodas E, Raa-Ortiz D. El requisito obligatorio del servicio social en salud del Perú: discriminatorio e inconstitucional. Rev. perú. med. exp. salud publica. 2014;31(4):781-7.
4.Perú. Ministerio de Salud. Decreto Supremo 005-97-SA de 1997: Reglamento de la Ley 23330, Ley del Servicio Rural y Urbano Marginal de Salud - SERUMS. Lima: Diario Oficial El Peruano; 1997.
5.Mejía CR, Quiñones-Laveriano DM, Espinoza KG, Quezada-Osoria C. Deficiente cobertura de aseguramiento a médicos durante el servicio rural y urbano-marginal en Perú. Rev. perú. med. exp. salud publica. 2013;30(2):220-3.
6.Galán-Rodas E, Díaz-Vélez C, Villena J, Maguiña C. Mortalidad de médicos que realizan el servicio rural (SERUMS) en Perú, 2006-2009. Rev. perú. med. exp. salud publica. 2010;27(3):483-4.
7.Wong P. Los nuevos mártires de la medicina en el Perú. An. Fac. med. 2009,70(2):151-2.
8.Inga-Berrospi F, Taype-Rondán Á, Purizaca-Rosillo N. La problemática del médico serumista en el Perú: conclusiones de la Segunda Convención Nacional de Médicos Serumistas, 2013. An Fac. med. 2014;75(3):271-2.
9.Perú. Ministerio de Salud. Resolución Ministerial 546 de 2011 (agosto 15): Norma Técnica de Salud “Categorías de establecimientos del sector salud”. Lima: Diario Oficial El Peruano; agosto 15 de 2011.
10.Qin R, Dzombak R, Amin R, Mehta K. Reliability of a telemedicine system designed for rural Kenya. J Prim Care Community Health. 2013;4(3):177-81.
11.World Health Organization. Increasing access to health workers in remote and rural areas through improved retention. Global policy recommendations. Geneva: WHO; 2010.
12.Strasser R. Rural health around the world: challenges and solutions. Fam Pract. 2003;20(4):457-63.
13.Muench J, Hoffman K, Ponce J, Calderón M, Meenan RT, Fiestas F. La atención primaria en los Estados Unidos y la experiencia peruana en perspectiva. Rev. perú. med. exp. salud publica. 2013;30(2):297-302.
14.Anticona-Huaynate CF, Pajuelo-Travezaño MJ, Correa M, Mayta-Malpartida H, Oberhelman R, Murphy LL, et al. Diagnostics barriers and innovations in rural areas: insights from junior medical doctors on the frontlines of rural care in Peru. BMC Health Serv Res. 2015;15(1):454.
15.Humphreys JS, Jones JA, Jones MP, Mildenhall D, Mara PR, Chater B, et al. The influence of geographical location on the complexity of rural general practice activities. Med J Aust. 2003;179(8):416-20.
16.Chin CD, Linder V, Sia SK. Lab-on-a-chip devices for global health: Past studies and future opportunities. Lab Chip. 2007;7(1):41-57.
17.Taype-Rondán Á, Inga-Berrospi F, Celestino RC, Bastidas F. Percepción de médicos recién egresados sobre las habilidades clínicas adquiridas durante el pregrado en Lima, Perú. Rev. méd. Chile. 2015;143(4):540-2.
18.Strasser R. Training for rural practice. Lessons from Australia. Can Fam Physician. 2001;47:2196-8.
19.Miranda JJ, López-Rivera LA, Quistberg DA, Rosales-Mayor E, Gianella C, Paca-Palao A, et al. Epidemiology of road traffic incidents in Peru 1973–2008: incidence, mortality, and fatality. PLoS One. 2014;9(6):e99662.
20.Muula AS. Country of residence and death among medical graduates from the Malawi College of Medicine, 1992-2002. S Afr Med J. 2006;96(8):662.
21.Murray CJ. Towards good practice for health statistics: lessons from the Millennium Development Goal health indicators. Lancet. 2007;369(9564):862-73.
22.Strasser RP, Harvey D, Burley M. The health service needs of small rural communities. Aust J Rural Health. 1994;2(2):7-13.
23.Mejía CR, Quiñones-Laveriano DM. SERUMS y la migración de médicos: a propósito de una cohorte de médicos de Lima. Rev. perú. med. exp. salud publica. 2015;32(2):405-6.
Recibido: 14 de julio de 2016; Aceptado: 20 de septiembre de 2016
Abstract
Introduction:
Social health services in Peru have certain problems such as unsafe work conditions, mortality associated with traffic accidents and poor insurance coverage.
Objective:
To describe the problems perceived and experienced by health professionals who render Rural and Urban Marginal Health Service (SERUMS in Spanish) in Ancash (Peru), and to evaluate their association with the profession and the category of the facilities where SERUMS is rendered.
Materials and methods:
In April 2015, an analytical cross-sectional study was carried out in professionals who were rendering SERUMS in facilities of the Ministry of Health in Ancash. Surveys were applied to collect general data, and characteristics and problems of SERUMS.
Results:
364 surveys were analyzed. 79.3% were females, and the average age was 27.4±5.0 years. During SERUMS, 80.0% of participants perceived lack of supplies, 54.4% perceived excessive workload, and 14.7% suffered some traffic accident. Being a physician and working in I-1 health facilities were factors associated with suffering traffic accidents and other kind of accidents.
Conclusions:
Respondents reported excessive workload, lack of supplies, and accidents. Accidents were more frequent in physicians and in I-1 health facilities.
Keywords:
Primary Health Care, Rural Health, Health Personnel, Job Satisfaction (MeSH).Resumen
Introducción.
En Perú, durante el servicio social en salud se han reportado problemas como condiciones laborales riesgosas, mortalidad asociada a accidentes de tránsito y déficit de cobertura de aseguramiento.
Objetivo.
Describir los problemas percibidos y experimentados por los profesionales de salud que realizan el Servicio Rural y Urbano Marginal de Salud (SERUMS) en Ancash, Perú, y evaluar su asociación con la práctica de los profesionales y la categoría del establecimiento donde se realiza el SERUMS.
Materiales y métodos.
Durante abril del 2015, se realizó un estudio transversal analítico con profesionales de salud que realizaban el SERUMS en establecimientos del Ministerio de Salud de Ancash. Se aplicaron encuestas para recolectar datos generales, características y problemas del SERUMS.
Resultados.
Se analizaron 364 encuestas. El 79.3% de los participantes fue de sexo femenino, la edad promedio fue de 27.4±5.0 años, 80.0% percibió carencia de insumos, 54.4% percibió carga laboral excesiva, y 14.7% sufrió algún accidente de tránsito durante el SERUMS. Ser médico y laborar en establecimientos I-1 fueron factores asociados a haber sufrido accidentes de tránsito y otros imprevistos.
Conclusiones.
Los encuestados reportan carga laboral excesiva, carencia de insumos y accidentes. Los accidentes son más frecuentes en médicos y en establecimientos de categoría I-1.
Palabras clave:
Atención primaria de salud, Salud rural, Personal de salud, Satisfacción en el trabajo (DeCS).Introduction
Given the inequities in the distribution of human resources in health, many countries establish social service policies, which encourage, condition or force health professionals to work in areas with poor access to health services to serve the most vulnerable populations 13. In Latin America, the obligatory nature of social service has been discussed in publications of Colombia 1, Mexico 2 and Peru 3.
In Peru, social service in health is known as Rural and Urban Marginal Health Service (SERUMS in Spanish) and the professionals who render their services are known as serumists. SERUMS regulates the practice of physicians, dentists, nurses, obstetricians, chemist-pharmacists, nutritionists, medical technologists, social workers, biologists, psychologists, veterinarians and sanitary engineers. Rendering SERUMS is mandatory to apply for positions in public entities, study professional specialization programs in Peru, and receive scholarships or other equivalent aids from the State 4.
SERUMS has managed to locate health professionals in many rural and remote areas of Peru. However, serious problems for professionals have been reported when rendering their services, such as the mandatory nature of the service, risky working conditions and real danger of death 3. In addition, studies carried out in physicians who render SERUMS have identified poor health insurance 5 and high mortality due, to a great extent, to traffic events 6,7.
In spite of the relevance of these problems, studies on serumists are scarce and have focused only on physicians. Due to the lack of information on the frequency of the problems and their risk groups, designing and prioritizing the corresponding interventions is difficult 8. Therefore, this study aims to describe the problems perceived and experienced by serumists in Ancash - Peru, and to evaluate their association with the professional practice of serumists and the category of the facilities where SERUMS is rendered.
Materials and methods
Study design and context
An analytical cross - sectional study was carried out applying surveys to healthcare professionals rendering SERUMS in Ancash, Peru.
In Peru, health facilities are divided into first, second and third level of care. First level prioritizes health prevention and promotion, and is divided into four categories: I-1, I-2, I-3 and I-4. Usually, category I-1 includes facilities with few equipment and are found in most rural areas away from reference health centers 9.
SERUMS is regulated by Law 23330 4, which establishes that it must be rendered in public health facilities of the Ministry of Health (MINSA), Social Security (EsSalud) or the Health Departments of the Armed Forces and the National Police of Peru for a year. Each year two processes are opened to award contracts: one in May (with the highest number of open positions) and another in October (with fewer positions).
Participants
This study included health professionals who were rendering SERUMS at a MINSA facility in Ancash during April 2015. This region was chosen because of the logistical support provided by the Regional Health Directorate of Ancash (DIRESA-Ancash). Working with MINSA health facilities was agreed because more serumist specialists are found there, and contact between them and the SERUMS coordinators, who were in charge of applying the surveys, is more frequent.
DIRESA-Ancash is divided into six geographically distributed health networks: Pacífico Sur (South Pacific), Pacífico Norte (North Pacific), Huaylas Sur (South Huaylas), Huaylas Norte (North Huaylas), Conchucos Sur (South Conchucos) and Conchucos Norte (North Conchucos). Each health network has a SERUMS coordinator, who is in charge of directing the work of the serumist specialists in their network.
During April 2015, 644 health professionals were rendering SERUMS in DIRESA-Ancash: 573 (89.0%) were located in MINSA health facilities, 42 (6.5%) in EsSalud health facilities, and 29 (4.5%) in health facilities of the Health Departments of the Armed Forces and the National Police.
Out of 573 MINSA members, the coordinators managed to involve 364 (63.5%), all of whom agreed to participate in this study. The health network with the highest percentage of respondents was Conchucos Sur (92.3%), and the lowest percentage was observed in Pacífico Norte (23.6%) (Figure 1).
Source: Own elaboration based on the data obtained in the study.
Figure 1: Serumists from the Ministry of Health surveyed in each of the six networks of the Ancash Regional Health Directorate.
Procedures
DIRESA-Ancash permission was requested to carry out the study and, with their support, the SERUMS coordinators of each health network in Ancash were trained to apply the surveys and respond the questions raised by serumists. The telephone number of the principal investigator was provided in all the surveys so that serum specialists could contact him in case of doubt.
In order to apply the surveys in their respective network, the SERUMS coordinators used two methods: a) applying the survey to serumists in person during meetings and supervision sessions in the health facilities, and b) sending the surveys to the health facilities where the serumists worked. In both cases, the participants used an envelope to submit their answers anonymously. This data collection was conducted throughout April 2015.
Then, two authors typed the surveys twice in the Excel 2010 program (Microsoft Corporation, USA), while a third author verified if both versions coincided. Mismatches were typed again.
Variables
The survey was developed by the researchers and included the following sections: general data such as age, sex, marital status, place where the undergraduate program was studied, financing of the university where the undergraduate program was studied, profession, year of graduation, as well as characteristics of the SERUMS such as type of contract, category of the health facility, process of enrollment in SERUMS (2014-I or 2014-II), at least three months being the head of the health facility, SERUMS problems, among others.
Regarding problems with SERUMS, the survey inquired about experiencing the following during the past month or at some point of their SERUMS: perception of lack of supplies that has prevented the basic management of a patient, some traffic accidents while working or traveling to the health facility, some other accidents (blows, burns, falls, etc.) while working that has caused incapacity for at least a few hours, or some theft while working.
In addition, data on other variables that are not included in this article were collected and will be presented in a subsequent analysis.
These variables correspond to the following parts of the survey: difficulty of SERUMS, violence during SERUMS, depressive symptoms during the last two weeks, professional expectations and retention.
Analysis plan
Data analysis was performed using the statistical software Stata v14.0 (StataCorp LP, USA). Central tendency measures, dispersion measures, absolute frequencies and relative frequencies were used for a descriptive presentation of the results. Prevalence ratios (PR) and 95% confidence intervals (95%CI) were estimated using crude and adjusted Poisson regressions with robust variance. p<0.05 was considered statistically significant.
The regression models evaluated the association between five outcomes of interest (excessive workload in last month, lack of supplies in last month, traffic accident during SERUMS, another type of accident during SERUMS, robbery during SERUMS), and two variables of interest (being a physician and rendering SERUMS in a category I-1 health facility).
For multiple regression models, the associations were adjusted for sex, age, undergraduate studies in Ancash, years passed since graduation until starting SERUMS, having a remunerated SERUMS contract, having served as head of the health facility for at least three months during SERUMS, rending SERUMS at an I-1 health facility, and being a physician.
Ethical considerations
The project was approved by the Ethics Committee of Hospital Nacional Docente Madre-Niño San Bartolomé (RCEI-40). Surveys were voluntary and anonymous, so participants signed an informed consent. The confidentiality of the collected data was preserved.
Results
364 surveys were applied to professionals who rendered SERUMS at MINSA facilities in Ancash in April 2015. 79.3% were female, the mean age was 27.4±5.0, 75.0% were single, 70.1% studied an undergraduate program in a university of Ancash, 45.6% were nurses, 24.3% were physicians, 47.4% entered the SERUMS just after graduating, 79.5% were rendering SERUMS in an I-1 health facility, and 81.5% were rendering SERUMS and being remunerated (Table 1).
* The others entered during the 2014-II process (October). † The others had an equivalent contract (ad honorem). Source: Own elaboration based on data obtained in the study.Table 1: Characteristics of the surveyed population (n=364).
When evaluating the problems faced by serumists during their service, it was found that 80.0% perceived that they lacked the necessary supplies for the basic management of a patient, and 51.6% perceived it during the last month. 54.4% perceived that the workload was excessive at some point, while 28.8% perceived it in the last month. 14.7% suffered some traffic accident during SERUMS while working or when traveling to their workplace, and 4.0% suffered it in the last month. 26.2% suffered other accidents (bumps, burns, falls, etc.) during SERUMS, which made them unable to work for at least a few hours, and 9.3% suffered an accident during the last month. 12.4% were robbed during SERUMS activities, and 9.3% was robbed during the last month (Table 2).
* n (%). Source: Own elaboration based on data obtained in the study.Table 2: Problems perceived and experienced sometime during SERUMS and sometime during the last month.
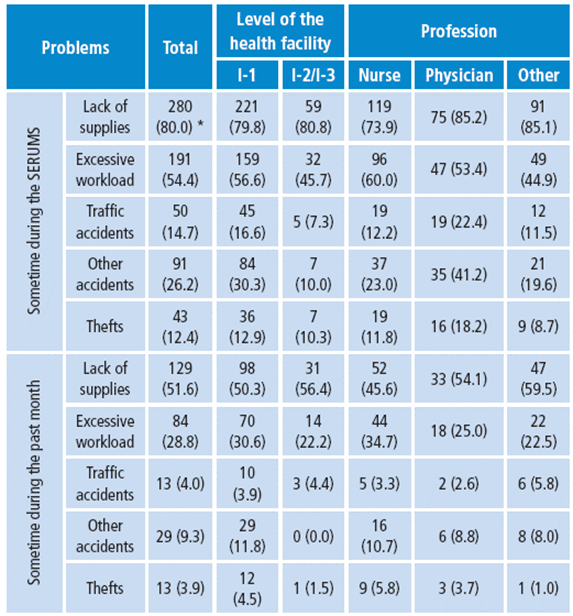
When evaluating the association between variables in the adjusted model, it was observed that rendering SERUMS at an I-1 health facility was associated with traffic accidents (PR=2.64; 95%CI: 1.00-6.99) and to suffering another accident during SERUMS (PR=2.81; 95%CI: 1.26-6.26). Similarly, being a physician was a factor associated with suffering another accident during SERUMS (PR=1.66; 95%CI: 1.00-2.75) (Table 3).
* PR (95%CI). † Adjusted for sex, age, university region, year of graduation (delay), equivalent contract, head of health facility and profession. ‡ Adjusted for sex, age, university region, year of graduation (delay), equivalent contract, head of health facility and health facility category. Source: Own elaboration based on data obtained in the study.Table 3: Variables observed and their association with working in a category I-1 health facility or being a physician.

Discussion
Excessive workload
54.4% of respondents perceived that the workload during SERUMS was excessive at some point, while 28.8% perceived it in the last month. These high figures could reflect the lack of staff in the health facilities where SERUMS is rendered, as well as inadequate training of serumists or lack of support from senior staff of the health facility.
Serumists often have little work experience. In addition, they must perform administrative and institutional management tasks for which they may not have adequate preparation during undergraduate training. It is therefore necessary to explore this workload and to evaluate proposed solutions such as telemedicine -which has proven to be effective to reduce the burden on health professionals working in rural areas in other countries- 10 or different training methods to assist serumists in their clinical and administrative work.
Lack of supplies
51.6% of the respondents said that the lack of supplies hindered the fulfillment of their duties some time during the last month. These shortcomings are characteristic in rural health services worldwide, especially in low and middle-income countries. They usually occur because budgets prioritize urban areas, while the budgef a/Zocated to rural areas is misapplied under the belief that these areas are "small cities" and that their health facilities are supplied in the same way as urban areas 11,12.
In Peru, first level health facilities are designed to carry out mostly promotional and preventive activities and to manage a small group of pathologies, deriving the most complex conditions to higher-level health facilities 13. However, this is not always possible due to the patients' fear, their economic status, the need for immediate action, the distance from higher-level health facilities or their denial to receive patients. These situations force health professionals to treat pathologies for which they do not have enough supplies (14, 15), and to provide suboptimal care that ends up promoting health inequity in rural areas 12.
To intervene this inequity, it is necessary to study in depth the lack of supplies and the best ways to overcome the situation. A recent qualitative study indicates that the interviewed serumists require diagnostic tests for specific decisions such as making a differential diagnosis between malaria and pneumonia in the jungle 14. These studies would identify the particular needs of each region and guide an efficient investment in supplies that could be used in rural areas 16.
In addition, it is important for health personnel at all levels of care to know what kind of pathologies they can treat in the health facilities where they are working and how they should refer patients to the next level of care. These issues could be assessed during pre-SERUMS training 17,18.
Accidents
In Peru, the estimated incidence of traffic incidents in persons over 18 years of age was 223 per 100 000 people in 2008 19. This study found that 14.7% of the respondents (14 700 per 100 000 people) reported being involved in a traffic accident during their SERUMS (that is, during the last 6 or 12 months). Despite the methodological differences between the cited study and this study, it is possible to assume that serumists have a high risk of suffering this type of accidents compared the rest of Peruvian inhabitants.
A report that only included serumist physicians in the 2006-2009 period identified traffic accidents as the leading cause of death, with a record of 7 deaths by traffic accidents out of 5 531 medical professionals (126.6 deaths per 100 000) 6. This incidence is much higher than that observed in reports of deaths among young physicians in other countries 20. Moreover, during that period, the estimated incidence of fatal traffic incidents among Peruvian citizens over the age of 18 was only 20 per 100 000 inhabitants 19.
The models evaluated in this study show that the prevalence of suffering traffic accidents during SERUMS is higher for physicians than for non-physicians, although, in the adjusted analysis, this association is not significant. This may occur because physicians make more trips, either referring patients or returning to their cities of origin, which may be quite distant, and because more than two thirds of the physicians surveyed have completed their studies in regions other than Ancash. Furthermore, an association between traffic accidents and SERUMS was found in relation to a category I-1 facility; this can be attributed to the remoteness and difficult access to these health facilities and their annexes.
Unfortunately, national data on mortality in non-medical serumists is not available. Data on other consequences of traffic accidents, such as temporary or permanent disability, are not available either. These data are necessary to develop and evaluate prevention policies 21.
The prevalence of other accidents (blows, burns, falls, etc.) while fulfilling serumist work was also higher in category I-1 health facilities. This may happen due to the fact that the communities served by these health facilities are more distant, which forces professionals to move for great distances to provide care, often using unsafe means of transportation in irregular terrains that may cause failures. In addition, these accidents were more prevalent in physicians, perhaps because they are more likely to move to remote locations, even to other villages, to treat their patients.
Unfortunately, many serumists do not have health insurance to protect them in case of accidents. Reports show that within three months after starting the contract, only 6.6% of the serumist physicians are provided with a social health insurance coverage for accidents and death 5, which causes multiple expenses and inconveniences to serumists who are involved in these accidents.
Now that the risks to which serumists are exposed are known, it is imperative that the relevant authorities take action. It is necessary to monitor the minimum security and access conditions to health facilities, to give serumists the possibility of accumulating days off to reduce the number of trips, and to provide vehicles or fuel for mobilization to remote communities. Interventions and monitoring should be prioritized for the groups at risk, in other words, physicians and those who work at I-1 health facilities.
It should be noted that this problem affects staff satisfaction and negatively influences the retention of health personnel 22, since it discourages serumist workers from working at the first level of care, as suggested by a previous cohort 23.
Limitations
This study has some limitations, such as the fact that our outcomes of interest were evaluated in a subjective way, according to the perception of the surveyor. In addition, the SERUMS coordinators could not find 36.5% of the serumists. It is possible that the missing population corresponds to those who render SERUMS in the most remote health facilities and, therefore, those who have more problems; hence, the results may underestimate the true magnitude of this issue.
Likewise, the extrapolation of the results is limited only to serumists of MINSA health facilities in Ancash. Serumists working for other health care providers or in other regions are likely to provide very different figures, which should be the subject of future studies.
The size of the sample included in this study has a power greater than 80% to determine PR values greater than 2.1 using multiple Poisson regressions, calculated with the PASS program v13.0 (NCSS, LLC, USA.). This implies that some associations could not be statistically confirmed due to the small size of the sample. However, no more subjects could be obtained since this was a census evaluation.
Strengths
To the knowledge of the authors, this is the first study to carry out a quantitative evaluation of the problems reported by the professionals who render SERUMS in Peru. The results reveal the magnitude of certain problems and identify two risk groups, which will help to develop and implement interventions to improve the working conditions of the serumist specialists.
Conclusions
The professionals who render SERUMS in Ancash suffer from excessive workload, lack of supplies, accidents and thefts. Being a physician and working in category I-1 health facilities are factors associated with suffering traffic accidents and other accidents that endanger integrity and even life. The relevant health authorities must supervise access and security conditions in such health facilities, prioritizing the identified risk groups.
Acknowledgement
The authors would like to express their gratitude to the authorities of the Regional Health Directorate of Ancash for granting their permission to conduct this study, and to the SERUMS coordinators of the Ancash health networks for their support in data collection.
References
Referencias
Moya MJ. Servicio social obligatorio en Colombia: incertidumbre de los recién graduados en medicina. Rev. Méd. Risaralda. 2014;20(2):114-120.
Nigenda G. Servicio social en medicina en México. Una reforma urgente y posible. Salud Publica Mex. 2013;55(5):519-27.
Mayta-Tristán P, Poterico JA, Galán-Rodas E, Raa-Ortiz D. El requisito obligatorio del servicio social en salud del Perú: discriminatorio e inconstitucional. Rev. perú. med. exp. salud publica. 2014;31(4):781-7.
Perú. Ministerio de Salud. Decreto Supremo 005-97-SA de 1997: Reglamento de la Ley 23330, Ley del Servicio Rural y Urbano Marginal de Salud - SERUMS. Lima: Diario Oficial El Peruano; 1997.
Mejía CR, Quiñones-Laveriano DM, Espinoza KG, Quezada-Osoria C. Deficiente cobertura de aseguramiento a médicos durante el servicio rural y urbano-marginal en Perú. Rev. perú. med. exp. salud publica. 2013;30(2):220-3.
Galán-Rodas E, Díaz-Vélez C, Villena J, Maguiña C. Mortalidad de médicos que realizan el servicio rural (SERUMS) en Perú, 2006-2009. Rev. perú. med. exp. salud publica. 2010;27(3):483-4.
Wong P. Los nuevos mártires de la medicina en el Perú. An. Fac. med. 2009,70(2):151-2.
Inga-Berrospi F, Taype-Rondán Á, Purizaca-Rosillo N. La problemática del médico serumista en el Perú: conclusiones de la Segunda Convención Nacional de Médicos Serumistas, 2013. An Fac. med. 2014;75(3):271-2.
Perú. Ministerio de Salud. Resolución Ministerial 546 de 2011 (agosto 15): Norma Técnica de Salud “Categorías de establecimientos del sector salud”. Lima: Diario Oficial El Peruano; agosto 15 de 2011.
Qin R, Dzombak R, Amin R, Mehta K. Reliability of a telemedicine system designed for rural Kenya. J Prim Care Community Health. 2013;4(3):177-81.
World Health Organization. Increasing access to health workers in remote and rural areas through improved retention. Global policy recommendations. Geneva: WHO; 2010.
Strasser R. Rural health around the world: challenges and solutions. Fam Pract. 2003;20(4):457-63.
Muench J, Hoffman K, Ponce J, Calderón M, Meenan RT, Fiestas F. La atención primaria en los Estados Unidos y la experiencia peruana en perspectiva. Rev. perú. med. exp. salud publica. 2013;30(2):297-302.
Anticona-Huaynate CF, Pajuelo-Travezaño MJ, Correa M, Mayta-Malpartida H, Oberhelman R, Murphy LL, et al. Diagnostics barriers and innovations in rural areas: insights from junior medical doctors on the frontlines of rural care in Peru. BMC Health Serv Res. 2015;15(1):454.
Humphreys JS, Jones JA, Jones MP, Mildenhall D, Mara PR, Chater B, et al. The influence of geographical location on the complexity of rural general practice activities. Med J Aust. 2003;179(8):416-20.
Chin CD, Linder V, Sia SK. Lab-on-a-chip devices for global health: Past studies and future opportunities. Lab Chip. 2007;7(1):41-57.
Taype-Rondán Á, Inga-Berrospi F, Celestino RC, Bastidas F. Percepción de médicos recién egresados sobre las habilidades clínicas adquiridas durante el pregrado en Lima, Perú. Rev. méd. Chile. 2015;143(4):540-2.
Strasser R. Training for rural practice. Lessons from Australia. Can Fam Physician. 2001;47:2196-8.
Miranda JJ, López-Rivera LA, Quistberg DA, Rosales-Mayor E, Gianella C, Paca-Palao A, et al. Epidemiology of road traffic incidents in Peru 1973–2008: incidence, mortality, and fatality. PLoS One. 2014;9(6):e99662.
Muula AS. Country of residence and death among medical graduates from the Malawi College of Medicine, 1992-2002. S Afr Med J. 2006;96(8):662.
Murray CJ. Towards good practice for health statistics: lessons from the Millennium Development Goal health indicators. Lancet. 2007;369(9564):862-73.
Strasser RP, Harvey D, Burley M. The health service needs of small rural communities. Aust J Rural Health. 1994;2(2):7-13.
Mejía CR, Quiñones-Laveriano DM. SERUMS y la migración de médicos: a propósito de una cohorte de médicos de Lima. Rev. perú. med. exp. salud publica. 2015;32(2):405-6.
Cómo citar
APA
ACM
ACS
ABNT
Chicago
Harvard
IEEE
MLA
Turabian
Vancouver
Descargar cita
Licencia
Derechos de autor 2017 Revista de la Facultad de Medicina

Esta obra está bajo una licencia Creative Commons Reconocimiento 3.0 Unported.
-