Characterization of congenital craniofacial anomalies in a specialized hospital of Risaralda, Colombia. 2010-2014
Caracterización de anomalías craneofaciales congénitas en hospital de cuarto nivel en Risaralda, Colombia, 2010-2014
DOI:
https://doi.org/10.15446/revfacmed.v66n2.61551Palabras clave:
Congenital Abnormalities, Skull, Face (en)Anomalías congénitas, Cráneo, Cara (es)
Descargas
Introduction: Congenital craniofacial malformations have a major impact on the lives of children and their relatives when the face is compromised since they may present along with cognitive deficits or altered facial appearance. There are no conclusive data on the presence of these malformations in the Coffee Region.
Objective: To identify the frequency of congenital craniofacial malformations during a 4-year period in a private institution of the city of Pereira, Risaralda, Colombia.
Materials and methods: Retrospective cross-sectional study. Data were collected from the medical records of 243 883 patients who were attended for the first time at a private health institution of the central-western region of Colombia. Statistical analysis was performed using the R software and Excel version 2007.
Results: Between January 2010 and December 2014, 1 807 patients with congenital craniofacial malformation were treated, which corresponds to 19.5% of the total of congenital anomalies, being cleft lip and palate the most frequent.
Conclusion: Although congenital cranial malformations occur frequently, there is little information about its etiology. Early diagnosis can prevent future complications that lead to deterioration of health or to an additional cost to the health system.
Introducción. Los defectos craneofaciales congénitos pueden causar un impacto en la vida de los niños y de sus familias cuando comprometen el rostro. Además, pueden estar acompañados de alteración de las funciones cerebrales o de la apariencia facial. No se tienen datos concluyentes sobre la presencia de estos defectos en el Eje Cafetero.
Objetivo. Identificar la frecuencia de las malformaciones craneofaciales congénitas en un periodo de cuatro años en una institución privada de la ciudad de Pereira, en Risaralda, Colombia.
Materiales y métodos. Estudio trasversal retrospectivo. La información fue recolectada a través del sistema de información de historias clínicas de pacientes que consultaron por primera vez en una institución privada de salud. El análisis estadístico fue realizado mediante el software R y Microsoft Excel versión 2007.
Resultados. Entre enero del 2010 y diciembre del 2014 se atendieron 1 807 pacientes con malformaciones craneofaciales congénitas, lo que corresponde al 19.5% del total de las anomalías congénitas. La hendidura labio-palatina fue la más frecuente.
Conclusiones. Aunque las malformaciones craneofaciales congénitas se presentan con frecuencia, se sabe muy poco de su etiología. El diagnóstico temprano puede prevenir futuras complicaciones que deterioren la salud o que generen un sobrecosto para el sistema de salud.
original research
DOI: https://doi.org/10.15446/revfacmed.v66n2.61551
Characterization of congenital craniofacial anomalies in a specialized hospital of Risaralda, Colombia. 2010-2014
Caracterización de anomalías craneofaciales congénitas en hospital de cuarto nivel en Risaralda, Colombia, 2010-2014
Received: 14/12/2016. Accepted: 15/02/2017.
Ximena Silva-Giraldo1,2 • Gloria Liliana Porras-Hurtado1,2
1 Clínica Comfamiliar - Pereira - Colombia.
2 Comfamiliar Health Research Group - Craniofacial Anomalies Research Line - Pereira - Colombia.
Corresponding author: Gloria Liliana Porras-Hurtado. Clínica Comfamiliar. Avenida circunvalar No. 3-01. Telephone number: +57 6 3135600, ext.: 2395. Pereira. Colombia. Email: gporras@comfamiliar.com.
| Abstract |
Introduction: Congenital craniofacial malformations have a major impact on the lives of children and their relatives when the face is compromised since they may present along with cognitive deficits or altered facial appearance. There are no conclusive data on the presence of these malformations in the Coffee Region.
Objective: To identify the frequency of congenital craniofacial malformations during a 4-year period in a private institution of the city of Pereira, Risaralda, Colombia.
Materials and methods: Retrospective cross-sectional study. Data were collected from the medical records of 243 883 patients who were attended for the first time at a private health institution of the central-western region of Colombia. Statistical analysis was performed using the R software and Excel version 2007.
Results: Between January 2010 and December 2014, 1 807 patients with congenital craniofacial malformation were treated, which corresponds to 19.5% of the total of congenital anomalies, being cleft lip and palate the most frequent.
Conclusion: Although congenital cranial malformations occur frequently, there is little information about its etiology. Early diagnosis can prevent future complications that lead to deterioration of health or to an additional cost to the health system.
Keywords: Congenital Abnormalities; Skull; Face (MeSH).
Silva-Giraldo X, Porras-Hurtado GL. Characterization of congenital craniofacial anomalies in a specialized hospital of Risaralda, Colombia. 2010-2014. Rev. Fac. Med. 2018;66(2)223-7. English. doi:
https://doi.org/10.15446/revfacmed.v66n2.61551.
| Resumen |
Introducción. Los defectos craneofaciales congénitos pueden causar un impacto en la vida de los niños y de sus familias cuando comprometen el rostro. Además, pueden estar acompañados de alteración de las funciones cerebrales o de la apariencia facial. No se tienen datos concluyentes sobre la presencia de estos defectos en el Eje Cafetero.
Objetivo. Identificar la frecuencia de las malformaciones craneofaciales congénitas en un periodo de cuatro años en una institución privada de la ciudad de Pereira, en Risaralda, Colombia.
Materiales y métodos. Estudio trasversal retrospectivo. La información fue recolectada a través del sistema de información de historias clínicas de pacientes que consultaron por primera vez en una institución privada de salud. El análisis estadístico fue realizado mediante el software R y Microsoft Excel versión 2007.
Resultados. Entre enero del 2010 y diciembre del 2014 se atendieron 1 807 pacientes con malformaciones craneofaciales congénitas, lo que corresponde al 19.5% del total de las anomalías congénitas. La hendidura labio-palatina fue la más frecuente.
Conclusiones. Aunque las malformaciones craneofaciales congénitas se presentan con frecuencia, se sabe muy poco de su etiología. El diagnóstico temprano puede prevenir futuras complicaciones que deterioren la salud o que generen un sobrecosto para el sistema de salud.
Palabras clave: Anomalías congénitas; Cráneo; Cara (DeCS).
Silva-Giraldo X, Porras-Hurtado GL. [Caracterización de anomalías craneofaciales congénitas en hospital de cuarto nivel en Risaralda, Colombia, 2010-2014]. Rev. Fac. Med. 2018;66(2):223-7. English. doi:
https://doi.org/10.15446/revfacmed.v66n2.61551.
Introduction
The frequency of congenital malformations is 310 per 10 000 births worldwide. Among them, craniofacial malformations represent between 10-15% of cases, including ear malformations with a prevalence of 74.1 per 10 000 births, followed by cleft lip and palate with 15.9 per 10 000 births. (1) Orofacial clefts are the most common and serious, and their frequency is highly variable depending on the population.
From an embryological perspective, the development of the head and neck begins with the formation of branchial or pharyngeal arches, which appear between the fourth and fifth week of intrauterine development. These arches are involved in the formation of the neck and the first and the second arches, in particular, play an important role in the formation of the face, which develops between the fourth and the twelfth week of the embryonic period. (2) The primary palate, the alveolar ridge and the premaxilla form during the sixth week, while the secondary palate ends its formation by the twelfth week. (3) Any noxa of environmental or genetic origin during this period can alter development, resulting in craniofacial malformations. (4)
Microtia, anotia or fistulas, preauricular appendages, facial clefts and craniosynostosis usually occur in isolation in 45-50% of cases. Moreover, they can be part of syndromic pictures, considered as syndromes, sequences, field defects or associations (5,6), such as the Charge syndrome, Townes-Brocks syndrome, BOR syndrome, Treacher Collins syndrome, diabetic embryopathy and facio-auricular-vertebra syndrome. (2) Some studies suggest that between 44-64% of patients with clefts have associated anomalies.
Congenital craniofacial malformations require early interdisciplinary management since they have an impact on the lives of children and their relatives when the face is involved, leaving sequels such as cognitive deficit or alteration of facial appearance. (7) There are no conclusive data on the presence of these malformations in the Coffee Region, so it is important to define a baseline regarding the most frequent cases in the region.
This study shows the frequency of congenital craniofacial malformations during a four-year period in a private institution of the city of Pereira in Risaralda, Colombia, with the purpose of providing data that allow proposing strategies for the prevention and management of these pathologies.
Materials and methods
This is an observational, descriptive and cross-sectional retrospective research. The information was extracted from an information system called Software AMAHO and SIIS, created in 2003 and patented on July 31, 2007 before the Ministry of the Interior and Justice of Colombia, which is part of institutional development initiatives and allows the interaction between clinical history, laboratory results and consultations for retrospective research.
This system stores daily records on care provided to the consulting population. For the period between January 2010 and December 2014, 243 883 patients were attended, generating 2 258 624 consultations, of which 1 435 451 were outpatient consultations, 116 485 inpatient consultations and 706 688 dental consultations. In other words, 25.9% of the inhabitants of the department of Risaralda were treated in this institution (according to DANE 2010-2014: 938 529 inhabitants). (8)
MySQL inquiries were made in the information system with the following inclusion criteria: patients from the department of Risaralda, first diagnosis associated with codes ICD-10Q000 to Q999 and codes K0701, K0704 and K0711, which are related to craniofacial malformation. Exclusion criteria were trauma and facial tumors. The variables included in the query were: entity of origin, age (since there was no cut-off point for age, the criteria was based on life cycles), sex, diagnosis according to ICD10 and health service that made the diagnosis.
Spreadsheets were used for data analysis and then exported to Software R version 3.1.3. An analysis of relative and absolute frequencies was carried out, together with the estimation of 95% confidence intervals for the general and specific prevalence of congenital craniofacial anomaly.
This study was approved by the Ethics Committee of the Institution and, according to resolution 8430 of 1993 of the Ministry of Health and Social Protection of Colombia, this research is classified as low risk.
Results
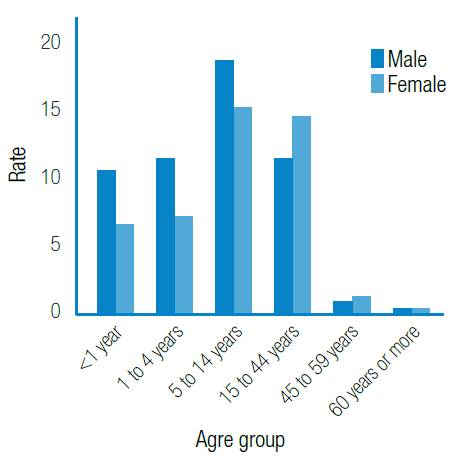
In the period between January 2010 and August 2014, 243 883 patients were treated achieving about 25.9% coverage for the department of Risaralda and its area of influence. Regarding this population (n=243 883), records related to congenital anomalies were found in 7 529 patients (3.08%, 95% CI 3.0-3.1). Of 7 529 patients with anomalies, 19.5% (95%CI 18.6-20.4) (n=1 494) had craniofacial malformations. The distribution of cases according to the variable of age and sex is shown in Figure 1.
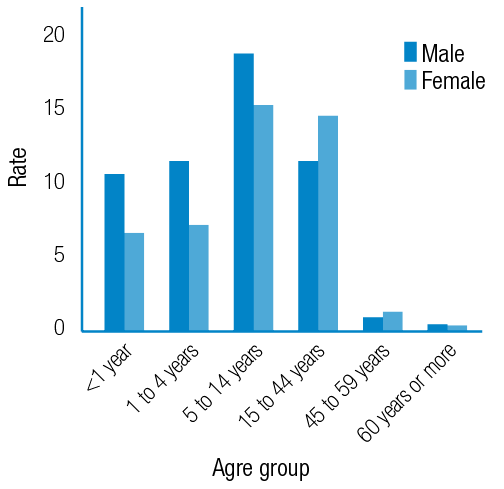
Figure 1. Frequency of patients with craniofacial anomalies by age and sex.
Source: Own elaboration based on the data obtained in the study.
A higher rate of craniofacial anomalies was observed in the age group of 5-14 years, which comprises 33.4% of the cases. The male sex is predominant with 58.4%, and a higher rate of diagnoses for both sexes was observed in the age group of 5-14 years. As for location, the distribution is presented in Figure 2.
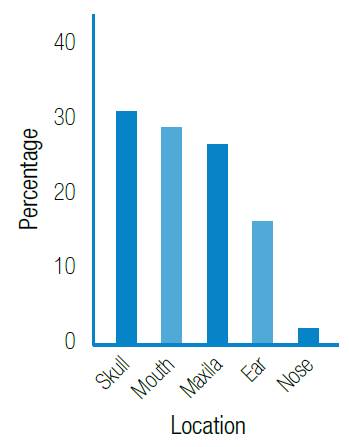
Places such as the mouth and skull represent about 60% of all craniofacial anomalies. The most frequent diagnoses include cleft lip and palate with 323 cases (18.9%) (Table 1), followed by retrognathism (11.7%), ankyloglossia (9.1%) and macrocephaly (9.0%). These diagnoses are associated with a 48.7% morbidity due to craniofacial anomaly.

Figure 2. Frequency of craniofacial anomalies according to anatomical location.
Source: Own elaboration based on the data obtained in the study.
Table 1. Cleft lip and palate distribution.
|
Group |
n |
% |
|
Cleft lip |
36 |
11.1 |
|
Cleft lip and palate |
133 |
41.2 |
|
Cleft palate |
154 |
47.7 |
Source: Own elaboration based on the data obtained in the study.
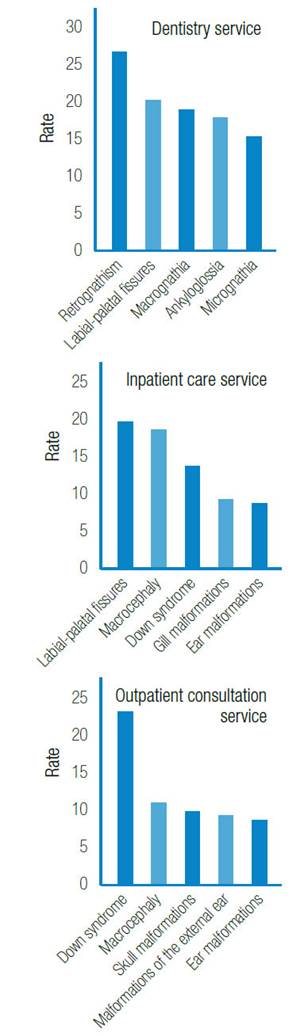
However, the order of diagnostic frequency varies according to the health service that treats the patient. Figure 3 shows this variation, with a greater proportion of retrognathism and cleft lip and palate diagnoses by the dentistry service, higher diagnosis of fissures and macrocephaly by the inpatient care service, and more Down syndrome, macrocephaly and skull deformities diagnosis by the outpatient consultation service. Regarding chromosomopathies, 79% of cases are Down syndrome.
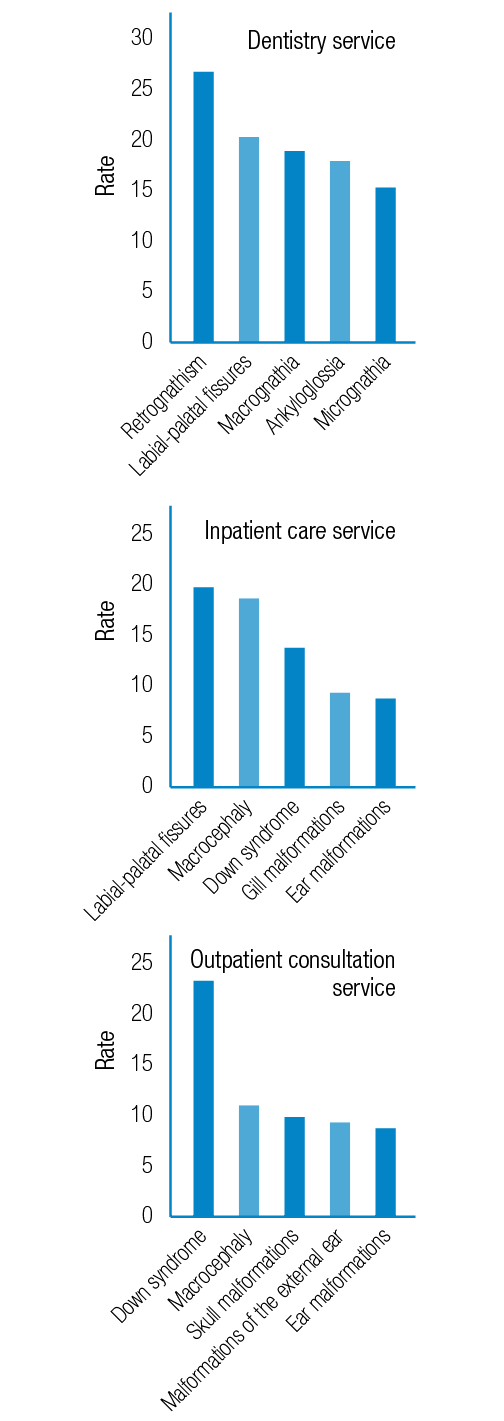
Figure 3. Frequency of patients with craniofacial anomaly by diagnosis and care service.
Source: Own elaboration based on the data obtained in the study.
Discussion
Consortiums such as FaceBase generate scientific initiatives to understand craniofacial malformations in an accelerated manner. Therefore, characterizing the population is the first step to propose diagnosis, therapy and prevention measures based on institutional reality and not on a global perspective. (9-11)
This study reports a rate of 3.1% of congenital defects, as well as a rate of 19.5% attributable to congenital craniofacial malformations among all anomalies; these figures are similar to those reported in the United States and other countries, including Colombia. (7-11) Congenital craniofacial malformations were observed more frequently in male patients, which coincides with the reports by Lisi A et al., who found that these malformations affect men more than women. (12) On the other hand, 323 lip and palate fissures were found, which corresponds to 1 in every 769 attended patients, a finding similar to that found in the literature, most often unilaterally and in the male gender (Table 1).
Oral cleft is one of the most frequent craniofacial congenital malformations, with a reported total prevalence between 1 and 2 per 1 000 live births. Considering differences in embryological development, epidemiology and patterns of family segregation, two types of clefts are observed: cleft lip with or without cleft palate (CL6P) and cleft palate (CP). They are more common in men than in women with a ratio of 2:1 (10) and may have a genetic or environmental etiology. The cause is unknown in 9.2% of cases, monogenic in 3.8%, chromosomal in 4.7% and only 0.6% attributable to teratogens. (13,14)
Worldwide, microtia and anotia have a prevalence of 0.1-2.5% and 0.1-0.6%, respectively. (1,15) Microtia can occur in isolation; however, the severity of this condition is associated with other pathologies such as vertebral anomalies, macrostomy, labial fissures, renal anomalies, facial asymmetry, cardiac defects, microphthalmia, holoprosencephaly and polydactyly. (10-11,16) In the studied population, microtia was reported with a frequency of 2.1%, which differs from other studies carried out in the country, which reported it as one of the most common. This may be related to the fact that this pathology is not reported in an appropriate manner; therefore, training and awareness among health professionals is important to improve diagnosis.
The high presence of retrognathia may suggest that a second assessment of patients with this diagnosis is necessary because of its correlation with Pierre Robin sequence (classic chain of micrognathia, glossoptosis and cleft palate). (11)
The most frequent diagnosis after retrognathia is ankyloglossia, an anomaly that has been defined differently over time. In 1982, it was defined as a frenulum that prevents the protrusion of the tongue, a frenulum that extends to the papillary surface of the tongue, and fissures in the tip of the tongue during normal movements. (17) In 2005, the definition changed to frenulum extending along 25–100% of tongue’s total length. (18) Ankyloglossia has a 4.2-10.7% worldwide prevalence (19). Proper diagnosis is important since this condition causes many difficulties such as limited protrusion of the tongue, difficulties for breastfeeding, impaired speech and lack of self-confidence. (20)
The high frequency of craniosynostosis in craniofacial deformities is confirmed by the literature, which reports an average of 1:2 000 live births. (21) About 60% of craniosynostoses are non-syndromic and 40% are syndromic. Although sagittal craniosynostosis is the most frequent within the non-syndromic craniosynostoses group, followed by metopic suture craniosynostosis (22), this study found a low frequency of 1:3 000 live births.
In 2010, the Colombian epidemiological surveillance system activated the mandatory reporting of congenital anomalies, which has required the development of institutional protocols for the systematic assessment of congenital anomalies in newborns. In 2012, the hospital in which the research was conducted joined the Latin American Collaborative Study of Congenital Malformations (ECLAMC by its acronym in Spanish) with a case-control methodology to intensify the search.
In 2013, the Nace una Sonrisa group, made up of professionals from the fields of Perinatology, Neonatology, Pediatrics, Genetics, Plastic Surgery, Maxillary Orthopedics, Phonoaudiology, Psychology, Social Work, Pediatric Dentistry, Maxillofacial Surgery and Orthodontics, was created to strengthen knowledge in each of these disciplines, thus achieving a comprehensive view, not only of diagnosis, but also of the treatment of craniofacial malformations.
Conclusions
The low frequency of microtia and craniosynostosis reported with respect to figures worldwide leads to intensify the active search of this cases and their proper notification. On the other hand, the characterization of the population allows greater optimization of both technological human resources and financial resources, since public health policies can be directed to address malformations with greater prevalence. Finally, an interdisciplinary team for craniofacial malformations care ensures timely management and increases the success of treatments.
Regarding the limitations of the study, the underreporting of diagnosis in hospital care and neonatology services is evident, since only some anomalies are described in the clinical history as lobed and retracted tongue, tongue hypoplasia and frenulum; only the dentistry service reports these observations as diagnosis.
Since this is a study with a cross-sectional design, including patients of any age and born in different places, it was not possible to identify the total base population to define the prevalence of craniofacial malformations in the region; only descriptions of the relative frequency were made based on medical records. Future studies should carry out an analysis of craniofacial malformations based on the identification of congenital anomalies and the epidemiological follow-up established by national standards.
Although congenital craniofacial malformations occur frequently, very little is known about their etiology. Health personnel lack clarity regarding its definition, classification and importance of diagnosing minor and major malformations, in order to look for associated pathologies.
Conflicts of interest
None stated by the authors.
Funding
None stated by the authors.
Acknowledgments
To Comfamiliar Risaralda for providing permanent training to its personnel.
References
1.Zarante I, López MA, Caro A, García-Reyes JC, Ospina JC. Impact and risk factors of craniofacial malformations in a Colombian population. Int. J. Pediatr. Otorhinolaryngol. 2009;73(10):1434-7. http://doi.org/fdknt4.
2.Vila-Morales D. Clasificación de las alteraciones cefalogénicas desde una visión integradora craneomaxilofacial. Rev. Cubana Estomatol. 2013;50(1):2-27.
3.Seifeldin SA. Is alveolar cleft reconstruction still controversial? (Review of literature). Saudi Dent J. 2016;28(1):3-11. http://doi.org/chs6.
4.Zarante I, Franco L, López C, Fernández N. Frecuencia de malformaciones congénitas: evaluación y pronóstico de 52.744 nacimientos en tres ciudades colombianas. Biomédica. 2010;30(1):65-71. http://doi.org/b4sm.
5.Shuper A, Merlob P, Grunebaum M, Reisner SH. The incidence of isolated craniosynostosis in the newborn infant. Am. J. Dis. Child. 1985;139(1):85-6.
6.Hunter AG, Rudd NL. Craniosynostosis. I. Sagittal synostosis: its genetics and associated clinical findings in 214 patients who lacked involvement of the coronal suture(s). Teratology. 1976;14(2):185-93. http://doi.org/fp3tf7.
7.Cifuentes-Cifuentes Y, Arteaga-Díaz C, Infante-Contreras C, Clavijo-López EG, Quintero-Guzmán C. Prevalencia y Caracterización de los Recién Nacidos con Anomalías Craneofaciales en el Instituto Materno Infantil de Bogotá. Rev. salud pública. 2008;10(3):423-32.
8.Colombia. Departamento Nacional de Planeación. DANE. 2015. [cited 2017 Dec 27]. Available from: https://goo.gl/Np2dSi.
9.Brinkley JF, Fisher S, Harris MP, Holmes G, Hooper JE, Jabs EW, et al. The FaceBase Consortium: a comprehensive resource for craniofacial researchers. Development. 2016;143(14):2677-88. http://doi.org/chs9.
10.Twigg SR, Wilkie AO. New insights into craniofacial malformations. Hum. Mol. Genet. 2015;24(R1):R50-9. http://doi.org/f7vbsn.
11.Neben CL, Roberts RR, Dipple KM, Merrill AE, Klein OD. Modeling craniofacial and skeletal congenital birth defects to advance therapies. Hum. Mol. Genet. 2016;25(R2):R86-R93. http://doi.org/f9p38z.
12.Lisi A, Botto LD, Rittler M, Castilla E, Bianca S, Bianchi F, et al. Sex and congenital malformations: an international perspective. Am. J. Med. Genet. A. 2005;134A(1):49-57. http://doi.org/fr82bh.
13.Rittler M, Lopez-Camelo JS, Castilla EE, Bermejo E, Cocchi G, Correa A, et al. Preferential associations between oral clefts and other major congenital anomalies. Cleft Palate Craniofac. J. 2008;45(5):525-32. http://doi.org/brddwq.
14.Luquetti DV, Cox TC, Lopez-Camelo J, Dutra Mda G, Cunningham ML, Castilla EE. Preferential Associated Anomalies in 818 Cases of Microtia in South America. Am. J. Med. Genet. A. 2013;161A(5):1051-7. http://doi.org/f94d97.
15.Sárközi A, Wyszynski DF, Czeizel AE. Oral clefts with associated anomalies: findings in the Hungarian Congenital Abnormality Registry. BMC Oral Health. 2005;5:4. http://doi.org/bd6wzs.
16.Luquetti DV., Heike CL, Hing AV., Cunningham ML, Cox TC. Microtia: Epidemiology and genetics. Am. J. Med. Genet. A. 2012;158A(1):124-39. http://doi.org/fnbtwb.
17.Ferrés-Amat E, Pastor-Vera T, Ferrés-Amat E, Mareque-Bueno J, Prats-Armengol J, Ferrés-Padró E. Multidisciplinary management of ankyloglossia in childhood. Treatment of 101 cases. A protocol. Med. Oral Patol. Oral Cir. Bucal. 2016;21(1):e39-47.
18.Ricke LA, Baker NJ, Madlon-Kay DJ, DeFor TA. Newborn tongue-tie: prevalence and effect on breast-feeding. J. Am. Board Fam. Pract. 2005;18(1):1-7.
19.Hogan M, Westcott C, Griffiths M. Randomized, controlled trial of division of tongue-tie in infants with feeding problems. J. Paediatr. Child Health. 2005;41(5-6):246-50. http://doi.org/ds7m9n.
20.Jangid K, Alexander AJ, Jayakumar ND, Varghese S, Ramani P. Ankyloglossia with cleft lip: A rare case report. J. Indian Soc. Periodontol. 2015;19(6):690-3. http://doi.org/chtf.
21.Vila-Morales D, Leyva-Mastrapa T, Alonso-Fernández L, Sánchez-Cabrales E, Lazo-Montero JC. Equipo cubano interdisciplinario de cirugía craneofacial en pediatría. Resultados de un quinquenio. Rev. Cubana Estomatol. 2010;47(1):62-80.
22.Mathijssen IM. Guideline for Care of Patients with the Diagnoses of Craniosynostosis: Working Group on Craniosynostosis. J. Craniofac. Surg. 2015;26(6):1735-807. http://doi.org/chtg.

Jean Marc Bourgery
“Traité complet de l’anatomie de l’homme”
Paris 1832-1854
Recibido: 14 de diciembre de 2016; Aceptado: 15 de febrero de 2017
Abstract
Introduction:
Congenital craniofacial malformations have a major impact on the lives of children and their relatives when the face is compromised since they may present along with cognitive deficits or altered facial appearance. There are no conclusive data on the presence of these malformations in the Coffee Region.
Objective:
To identify the frequency of congenital craniofacial malformations during a 4-year period in a private institution of the city of Pereira, Risaralda, Colombia.
Materials and methods:
Retrospective cross-sectional study. Data were collected from the medical records of243 883 patients who were attended for the first time at a private health institution of the central-western region of Colombia. Statistical analysis was performed using the R software and Excel version 2007.
Results:
Between January 2010 and December 2014, 1 807 patients with congenital craniofacial malformation were treated, which corresponds to 19.5% of the total of congenital anomalies, being cleft lip and palate the most frequent.
Conclusion:
Although congenital cranial malformations occur frequently, there is little information about its etiology. Early diagnosis can prevent future complications that lead to deterioration of health or to an additional cost to the health system.
Keywords:
Congenital Abnormalities, Skull, Face (MeSH).Resumen
Introducción.
Los defectos craneofaciales congénitos pueden causar un impacto en la vida de los niños y de sus familias cuando comprometen el rostro. Además, pueden estar acompañados de alteración de las funciones cerebrales o de la apariencia facial. No se tienen datos concluyentes sobre la presencia de estos defectos en el Eje Cafetero.
Objetivo.
Identificar la frecuencia de las malformaciones craneofaciales congénitas en un periodo de cuatro años en una institución privada de la ciudad de Pereira, en Risaralda, Colombia.
Materiales y métodos.
Estudio trasversal retrospectivo. La información fue recolectada a través del sistema de información de historias clínicas de pacientes que consultaron por primera vez en una institución privada de salud. El análisis estadístico fue realizado mediante el software R y Microsoft Excel versión 2007.
Resultados.
Entre enero del 2010 y diciembre del 2014 se atendieron 1 807 pacientes con malformaciones craneofaciales congénitas, lo que corresponde al 19.5% del total de las anomalías congénitas. La hendidura labio-palatina fue la más frecuente.
Conclusiones.
Aunque las malformaciones craneofaciales congénitas se presentan con frecuencia, se sabe muy poco de su etiología. El diagnóstico temprano puede prevenir futuras complicaciones que deterioren la salud o que generen un sobrecosto para el sistema de salud.
Palabras clave:
Anomalías congénitas, Cráneo, Cara (DeCS).Introduction
The frequency of congenital malformations is 310 per 10 000 births worldwide. Among them, craniofacial malformations represent between 10-15% of cases, including ear malformations with a prevalence of 74.1 per 10 000 births, followed by cleft lip and palate with 15.9 per 10 000 births. 1 Orofacial clefts are the most common and serious, and their frequency is highly variable depending on the population.
From an embryological perspective, the development of the head and neck begins with the formation of branchial or pharyngeal arches, which appear between the fourth and fifth week of intrauterine development. These arches are involved in the formation of the neck and the first and the second arches, in particular, play an important role in the formation of the face, which develops between the fourth and the twelfth week of the embryonic period. 2 The primary palate, the alveolar ridge and the premaxilla form during the sixth week, while the secondary palate ends its formation by the twelfth week. 3 Any noxa of environmental or genetic origin during this period can alter development, resulting in craniofacial malformations. 4
Microtia, anotia or fistulas, preauricular appendages, facial clefts and craniosynostosis usually occur in isolation in 45-50% of cases. Moreover, they can be part of syndromic pictures, considered as syndromes, sequences, field defects or associations 5,6, such as the Charge syndrome, Townes-Brocks syndrome, BOR syndrome, Treacher Collins syndrome, diabetic embryopathy and facio-auricular-vertebra syndrome. 2 Some studies suggest that between 44-64% of patients with clefts have associated anomalies.
Congenital craniofacial malformations require early interdisciplinary management since they have an impact on the lives of children and their relatives when the face is involved, leaving sequels such as cognitive deficit or alteration of facial appearance. 7 There are no conclusive data on the presence of these malformations in the Coffee Region, so it is important to define a baseline regarding the most frequent cases in the region.
This study shows the frequency of congenital craniofacial malformations during a four-year period in a private institution of the city of Pereira in Risaralda, Colombia, with the purpose of providing data that allow proposing strategies for the prevention and management of these pathologies.
Materials and methods
This is an observational, descriptive and cross-sectional retrospective research. The information was extracted from an information system called Software AMAHO and SIIS, created in 2003 and patented on July 31, 2007 before the Ministry of the Interior and Justice of Colombia, which is part of institutional development initiatives and allows the interaction between clinical history, laboratory results and consultations for retrospective research.
This system stores daily records on care provided to the consulting population. For the period between January 2010 and December 2014, 243 883 patients were attended, generating 2 258 624 consultations, of which 1 435 451 were outpatient consultations, 116 485 inpatient consultations and 706 688 dental consultations. In other words, 25.9% of the inhabitants of the department of Risaralda were treated in this institution (according to DANE 2010-2014: 938 529 inhabitants). 8
MySQL inquiries were made in the information system with the following inclusion criteria: patients from the department of Risaralda, first diagnosis associated with codes ICD-10Q000 to Q999 and codes K0701, K0704 and K0711, which are related to craniofacial malformation. Exclusion criteria were trauma and facial tumors. The variables included in the query were: entity of origin, age (since there was no cut-off point for age, the criteria was based on life cycles), sex, diagnosis according to ICD10 and health service that made the diagnosis.
Spreadsheets were used for data analysis and then exported to Software R version 3.1.3. An analysis of relative and absolute frequencies was carried out, together with the estimation of 95% confidence intervals for the general and specific prevalence of congenital craniofacial anomaly.
This study was approved by the Ethics Committee of the Institution and, according to resolution 8430 of 1993 of the Ministry of Health and Social Protection of Colombia, this research is classified as low risk.
Results
In the period between January 2010 and August 2014, 243 883 patients were treated achieving about 25.9% coverage for the department of Risaralda and its area of influence. Regarding this population (n=243 883), records related to congenital anomalies were found in 7 529 patients (3.08%, 95% CI 3.0-3.1). Of 7 529 patients with anomalies, 19.5% (95%CI 18.6-20.4) (n=1 494) had craniofacial malformations. The distribution of cases according to the variable of age and sex is shown in Figure 1.
Figure 1: Frequency of patients with craniofacial anomalies by age and sex.
A higher rate of craniofacial anomalies was observed in the age group of 5-14 years, which comprises 33.4% of the cases. The male sex is predominant with 58.4%, and a higher rate of diagnoses for both sexes was observed in the age group of 5-14 years. As for location, the distribution is presented in Figure 2.
Figure 2: Frequency of craniofacial anomalies according to anatomical location.
Places such as the mouth and skull represent about 60% of all craniofacial anomalies. The most frequent diagnoses include cleft lip and palate with 323 cases (18.9%) (Table 1), followed by retrognathism (11.7%), ankyloglossia (9.1%) and macrocephaly (9.0%). These diagnoses are associated with a 48.7% morbidity due to craniofacial anomaly.
Table 1: Cleft lip and palate distribution.

Source: Own elaboration based on the data obtained in the study.
However, the order of diagnostic frequency varies according to the health service that treats the patient. Figure 3 shows this variation, with a greater proportion of retrognathism and cleft lip and palate diagnoses by the dentistry service, higher diagnosis of fissures and macrocephaly by the inpatient care service, and more Down syndrome, macrocephaly and skull deformities diagnosis by the outpatient consultation service. Regarding chromosomopathies, 79% of cases are Down syndrome.
Figure 3: Frequency of patients with craniofacial anomaly by diagnosis and care service.
Discussion
Consortiums such as FaceBase generate scientific initiatives to understand craniofacial malformations in an accelerated manner. Therefore, characterizing the population is the first step to propose diagnosis, therapy and prevention measures based on institutional reality and not on a global perspective. 9-11
This study reports a rate of 3.1% of congenital defects, as well as a rate of 19.5% attributable to congenital craniofacial malformations among all anomalies; these figures are similar to those reported in the United States and other countries, including Colombia. 7-11 Congenital craniofacial malformations were observed more frequently in male patients, which coincides with the reports by Lisi A et al., who found that these malformations affect men more than women. 12 On the other hand, 323 lip and palate fissures were found, which corresponds to 1 in every 769 attended patients, a finding similar to that found in the literature, most often unilaterally and in the male gender (Table 1).
Oral cleft is one of the most frequent craniofacial congenital malformations, with a reported total prevalence between 1 and 2 per 1 000 live births. Considering differences in embryological development, epidemiology and patterns of family segregation, two types of clefts are observed: cleft lip with or without cleft palate (CL6P) and cleft palate (CP). They are more common in men than in women with a ratio of 2:1 10 and may have a genetic or environmental etiology. The cause is unknown in 9.2% of cases, monogenic in 3.8%, chromosomal in 4.7% and only 0.6% attributable to teratogens. 13,14
Worldwide, microtia and anotia have a prevalence of 0.1-2.5% and 0.1-0.6%, respectively. 1,15 Microtia can occur in isolation; however, the severity of this condition is associated with other pathologies such as vertebral anomalies, macrostomy, labial fissures, renal anomalies, facial asymmetry, cardiac defects, microphthalmia, holoprosencephaly and polydactyly. 10-11,16 In the studied population, microtia was reported with a frequency of 2.1%, which differs from other studies carried out in the country, which reported it as one of the most common. This may be related to the fact that this pathology is not reported in an appropriate manner; therefore, training and awareness among health professionals is important to improve diagnosis.
The high presence of retrognathia may suggest that a second assessment of patients with this diagnosis is necessary because of its correlation with Pierre Robin sequence (classic chain of micrognathia, glossoptosis and cleft palate). 11
The most frequent diagnosis after retrognathia is ankyloglossia, an anomaly that has been defined differently over time. In 1982, it was defined as a frenulum that prevents the protrusion of the tongue, a frenulum that extends to the papillary surface of the tongue, and fissures in the tip of the tongue during normal movements. 17 In 2005, the definition changed to frenulum extending along 25-100% of tongue's total length. 18 Ankyloglossia has a 4.2-10.7% worldwide prevalence 19. Proper diagnosis is important since this condition causes many difficulties such as limited protrusion of the tongue, difficulties for breastfeeding, impaired speech and lack of self-confidence. 20
The high frequency of craniosynostosis in craniofacial deformities is confirmed by the literature, which reports an average of 1:2 000 live births. 21 About 60% of craniosynostoses are non-syndromic and 40% are syndromic. Although sagittal craniosynostosis is the most frequent within the non-syndromic craniosynostoses group, followed by metopic suture craniosynostosis 22, this study found a low frequency of 1:3 000 live births.
In 2010, the Colombian epidemiological surveillance system activated the mandatory reporting of congenital anomalies, which has required the development of institutional protocols for the systematic assessment of congenital anomalies in newborns. In 2012, the hospital in which the research was conducted joined the Latin American Collaborative Study of Congenital Malformations (ECLAMC by its acronym in Spanish) with a case-control methodology to intensify the search.
In 2013, the Nace una Sonrisa group, made up of professionals from the fields of Perinatology, Neonatology, Pediatrics, Genetics, Plastic Surgery, Maxillary Orthopedics, Phonoaudiology, Psychology, Social Work, Pediatric Dentistry, Maxillofacial Surgery and Orthodontics, was created to strengthen knowledge in each of these disciplines, thus achieving a comprehensive view, not only of diagnosis, but also of the treatment of craniofacial malformations.
Conclusions
The low frequency of microtia and craniosynostosis reported with respect to figures worldwide leads to intensify the active search of this cases and their proper notification. On the other hand, the characterization of the population allows greater optimization of both technological human resources and financial resources, since public health policies can be directed to address malformations with greater prevalence. Finally, an interdisciplinary team for craniofacial malformations care ensures timely management and increases the success of treatments.
Regarding the limitations of the study, the underreporting of diagnosis in hospital care and neonatology services is evident, since only some anomalies are described in the clinical history as lobed and retracted tongue, tongue hypoplasia and frenulum; only the dentistry service reports these observations as diagnosis.
Since this is a study with a cross-sectional design, including patients of any age and born in different places, it was not possible to identify the total base population to define the prevalence of craniofacial malformations in the region; only descriptions of the relative frequency were made based on medical records. Future studies should carry out an analysis of craniofacial malformations based on the identification of congenital anomalies and the epidemiological follow-up established by national standards.
Although congenital craniofacial malformations occur frequently, very little is known about their etiology. Health personnel lack clarity regarding its definition, classification and importance of diagnosing minor and major malformations, in order to look for associated pathologies.
Acknowledgments
To Comfamiliar Risaralda for providing permanent training to its personnel.
References
Referencias
Zarante I, López MA, Caro A, García-Reyes JC, Ospina JC. Impact and risk factors of craniofacial malformations in a Colombian population. Int. J. Pediatr. Otorhinolaryngol. 2009;73(10):1434-7. http://doi.org/fdknt4.
Vila-Morales D. Clasificación de las alteraciones cefalogénicas desde una visión integradora craneomaxilofacial. Rev. Cubana Estomatol. 2013;50(1):2-27.
Seifeldin SA. Is alveolar cleft reconstruction still controversial? (Review of literature). Saudi Dent J. 2016;28(1):3-11. http://doi.org/chs6.
Zarante I, Franco L, López C, Fernández N. Frecuencia de malformaciones congénitas: evaluación y pronóstico de 52.744 nacimientos en tres ciudades colombianas. Biomédica. 2010;30(1):65-71. http://doi.org/b4sm.
Shuper A, Merlob P, Grunebaum M, Reisner SH. The incidence of isolated craniosynostosis in the newborn infant. Am. J. Dis. Child. 1985;139(1):85-6.
Hunter AG, Rudd NL. Craniosynostosis. I. Sagittal synostosis: its genetics and associated clinical findings in 214 patients who lacked involvement of the coronal suture(s). Teratology. 1976;14(2):185-93. http://doi.org/fp3tf7.
Cifuentes-Cifuentes Y, Arteaga-Díaz C, Infante-Contreras C, Clavijo-López EG, Quintero-Guzmán C. Prevalencia y Caracterización de los Recién Nacidos con Anomalías Craneofaciales en el Instituto Materno Infantil de Bogotá. Rev. salud pública. 2008;10(3):423-32.
Colombia. Departamento Nacional de Planeación. DANE. 2015. [cited 2017 Dec 27]. Available from: https://goo.gl/Np2dSi.
Brinkley JF, Fisher S, Harris MP, Holmes G, Hooper JE, Jabs EW, et al. The FaceBase Consortium: a comprehensive resource for craniofacial researchers. Development. 2016;143(14):2677-88. http://doi.org/chs9.
Twigg SR, Wilkie AO. New insights into craniofacial malformations. Hum. Mol. Genet. 2015;24(R1):R50-9. http://doi.org/f7vbsn.
Neben CL, Roberts RR, Dipple KM, Merrill AE, Klein OD. Modeling craniofacial and skeletal congenital birth defects to advance therapies. Hum. Mol. Genet. 2016;25(R2):R86-R93. http://doi.org/f9p38z.
Lisi A, Botto LD, Rittler M, Castilla E, Bianca S, Bianchi F, et al. Sex and congenital malformations: an international perspective. Am. J. Med. Genet. A. 2005;134A(1):49-57. http://doi.org/fr82bh.
Rittler M, Lopez-Camelo JS, Castilla EE, Bermejo E, Cocchi G, Correa A, et al. Preferential associations between oral clefts and other major congenital anomalies. Cleft Palate Craniofac. J. 2008;45(5):525-32. http://doi.org/brddwq.
Luquetti DV, Cox TC, Lopez-Camelo J, Dutra Mda G, Cunningham ML, Castilla EE. Preferential Associated Anomalies in 818 Cases of Microtia in South America. Am. J. Med. Genet. A. 2013;161A(5):1051-7. http://doi.org/f94d97.
Sárközi A, Wyszynski DF, Czeizel AE. Oral clefts with associated anomalies: findings in the Hungarian Congenital Abnormality Registry. BMC Oral Health. 2005;5:4. http://doi.org/bd6wzs.
Luquetti DV., Heike CL, Hing AV., Cunningham ML, Cox TC. Microtia: Epidemiology and genetics. Am. J. Med. Genet. A. 2012;158A(1):124-39. http://doi.org/fnbtwb.
Ferrés-Amat E, Pastor-Vera T, Ferrés-Amat E, Mareque-Bueno J, Prats-Armengol J, Ferrés-Padró E. Multidisciplinary management of ankyloglossia in childhood. Treatment of 101 cases. A protocol. Med. Oral Patol. Oral Cir. Bucal.2016;21(1):e39-47.
Ricke LA, Baker NJ, Madlon-Kay DJ, DeFor TA. Newborn tongue-tie: prevalence and effect on breast-feeding. J. Am. Board Fam. Pract. 2005;18(1):1-7.
Hogan M, Westcott C, Griffiths M. Randomized, controlled trial of division of tongue-tie in infants with feeding problems. J. Paediatr. Child Health. 2005;41(5-6):246-50. http://doi.org/ds7m9n.
Jangid K, Alexander AJ, Jayakumar ND, Varghese S, Ramani P. Ankyloglossia with cleft lip: A rare case report. J. Indian Soc. Periodontol. 2015;19(6):690-3. http://doi.org/chtf.
Vila-Morales D, Leyva-Mastrapa T, Alonso-Fernández L, Sánchez-Cabrales E, Lazo-Montero JC. Equipo cubano interdisciplinario de cirugía craneofacial en pediatría. Resultados de un quinquenio. Rev. Cubana Estomatol. 2010;47(1):62-80.
Mathijssen IM. Guideline for Care of Patients with the Diagnoses of Craniosynostosis: Working Group on Craniosynostosis. J. Craniofac. Surg. 2015;26(6):1735-807. http://doi.org/chtg.
Cómo citar
APA
ACM
ACS
ABNT
Chicago
Harvard
IEEE
MLA
Turabian
Vancouver
Descargar cita
CrossRef Cited-by
1. Meng Xie, Markéta Kaiser, Yaakov Gershtein, Daniela Schnyder, Ruslan Deviatiiarov, Guzel Gazizova, Elena Shagimardanova, Tomáš Zikmund, Greet Kerckhofs, Evgeny Ivashkin, Dominyka Batkovskyte, Phillip T. Newton, Olov Andersson, Kaj Fried, Oleg Gusev, Hugo Zeberg, Jozef Kaiser, Igor Adameyko, Andrei S. Chagin. (2024). The level of protein in the maternal murine diet modulates the facial appearance of the offspring via mTORC1 signaling. Nature Communications, 15(1) https://doi.org/10.1038/s41467-024-46030-3.
Dimensions
PlumX
Visitas a la página del resumen del artículo
Descargas
Licencia
Derechos de autor 2018 Revista de la Facultad de Medicina

Esta obra está bajo una licencia Creative Commons Reconocimiento 3.0 Unported.
Derechos de autor
Los autores deben aceptar transferir a la Revista de la Facultad de Medicina los derechos de autor de los artículos publicados. La editorial tiene el derecho del uso, reproducción, transmisión, distribución y publicación en cualquier forma o medio. Los autores no podrán permitir o autorizar el uso de la contribución sin el consentimiento escrito de la revista. Estos archivos están disponibles en https://goo.gl/EfWPdX y https://goo.gl/6zztk4 y deben cargarse en el paso 4 del envío OJS (archivos complementarios).
La carta de cesión de derechos de autor y la de responsabilidad de autoría deben ser entregadas junto con el original.
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
- Los autores/as conservarán sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación esta revista.
- Los autores/as podrán adoptar otros acuerdos de licencia no exclusiva de distribución de la versión de la obra publicada (p. ej.: depositarla en un archivo telemático institucional o publicarla en un volumen monográfico) siempre que se indique la publicación inicial en esta revista.
- Se permite y recomienda a los autores/as difundir su obra a través de Internet (p. ej.: en archivos telemáticos institucionales o en su página web) antes y durante el proceso de envío, lo cual puede producir intercambios interesantes y aumentar las citas de la obra publicada. (Véase El efecto del acceso abierto).